Abstract
Background
Acute kidney injury (AKI) is common in the pediatric intensive care unit (ICU) and is associated with poorer clinical outcomes. There is scarce data to support an association between nutritional status and nutrient delivery in critically ill pediatric patients. Therefore, the present study aimed to identify the nutritional and clinical factors associated with the development of AKI during pediatric ICU stay.
Methods
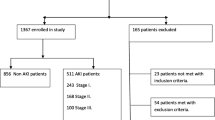
This prospective study included critically ill pediatric patients aged < 15 years who were admitted to the medical and surgical pediatric ICU. Clinical, laboratory, nutritional status, nutritional therapy parameters, and AKI data were recorded. Adjusted logistic regression was applied and expressed as odds ratio (OR) and 95% confidence interval (95%CI). P-value < 0.05 was considered significant.
Results
We enrolled 108 patients with a median age of 9 months (interquartile range/IQR 2.4–62.5), and 43.5% developed AKI. Sepsis/septic shock (OR 8.00; 95% CI 2.06–32.51, p = 0.003), higher severity of illness (OR 1.89; 95% CI 1.24–2.90, p = 0.003), hypoalbuminemia (OR 4.11; 95% CI 1.61–10.46, p = 0.006), edema (OR 3.42, 95% CI 1.10–10.67, p = 0.034), fluid overload (OR 3.52, 95% CI 1.56–7.96, p = 0.003), need for mechanical ventilation (OR 3.62, 95% CI 1.45–9.04, p = 0.006) and adequate protein intake (OR 0.79, 95% CI 0.63–1.00, p = 0.048) were associated with development of AKI.
Conclusions
Hypoalbuminemia, need for mechanical ventilation, fluid overload, severity of illness, sepsis/septic shock, and edema were risk factors for AKI in pediatric ICU. Furthermore, adequate protein intake is associated with AKI during pediatric ICU stay, making it important to implement nutritional assessment and nutritional therapy protocols for critically ill pediatric patients.
Graphical abstract

Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Kyle UG, Akcan-Arikan A, Orellana RA, Coss-Bu JA (2013) Nutrition support among critically ill children with AKI. Clin J Am Soc Nephrol 8(4):568–574. https://doi.org/10.2215/CJN.05790612
Costa CAD, Garcia PCR, Cabral DD, Tonial CT, Bruno F, Enloft PR, Velozo KDS (2018) Reducing malnutrition in critically ill pediatric patients. Rev Bras Ter Intensiva 30(2):160–165. https://doi.org/10.5935/0103-507X.20180034
Brown AM, Carpenter D, Keller G, Morgan S, Irving SY (2015) Enteral nutrition in the PICU: current status and ongoing challenges. J Pediatr Intensive Care 4(2):111–120. https://doi.org/10.1055/s-0035-1559806
Cleto-Yamane TL, Gomes CLR, Suassuna JHR, Nogueira PK (2019) Acute kidney injury epidemiology in pediatrics. J Bras Nefrol 41(2):275–283. https://doi.org/10.1590/2175-8239-JBN-2018-0127
Almeida JP, Valente IF, Lordelo MDR (2018) Association between pediatric risk, injury, failure, loss and end stage renal disease score and mortality in a pediatric intensive care unit: a retrospective study. Rev Bras Ter Intensiva 30(4):429–435. https://doi.org/10.5935/0103-507X.20180065
Leite HP, de Lima LF, de Oliveira Iglesias SB, Pacheco JC, de Carvalho WB (2013) Malnutrition may worsen the prognosis of critically ill children with hyperglycemia and hypoglycemia. JPEN J Parenter Enteral Nutr 37(3):335–341. https://doi.org/10.1177/0148607112458124
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Inter Suppl 2:1–138
Ramakrishnan N, Shankar B (2020) Nutrition support in critically ill patients with AKI. Indian J Crit Care Med 24(Suppl 3):S135–S139. https://doi.org/10.5005/jp-journals-10071-23397
Benichel CR, Meneguin S (2020) Risk factors for acute renal injury in intensive clinical patients. Acta Paul Enferm. https://doi.org/10.37689/acta-ape/2020AO0064
Slater A, Shann F, Pearson G (2003) Paediatric Index of Mortality (PIM) Study Group. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med 29(2):278–285. https://doi.org/10.1007/s00134-002-1601-2
Edwards JD, Houtrow AJ, Vasilevskis EE, Rehm RS, Markovitz BP, Graham RJ, Dudley RA (2012) Chronic conditions among children admitted to U.S. pediatric intensive care units: their prevalence and impact on risk for mortality and prolonged length of stay*. Crit Care Med 40(7):2196–2203. https://doi.org/10.1097/CCM.0b013e31824e68cf
Hassinger AB, Wald EL, Goodman DM (2014) Early postoperative fluid overload precedes acute kidney injury and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr Crit Care Med 15(2):131–138. https://doi.org/10.1097/PCC.0000000000000043
Merker M, Felder M, Gueissaz L, Bolliger R, Tribolet P, Kägi-Braun N, Gomes F, Hoess C, Pavlicek V, Bilz S, Sigrist S, Brändle M, Henzen C, Thomann R, Rutishauser J, Aujesky D, Rodondi N, Donzé J, Stanga Z, Mueller B, Schuetz P (2020) Association of baseline inflammation with effectiveness of nutritional support among patients with disease-related malnutrition: a secondary analysis of a randomized clinical trial. JAMA Netw Open 3(3):e200663. https://doi.org/10.1001/jamanetworkopen.2020.0663
World Health Organization (WHO) (1995) Expert committee on physical status: the use and interpretation of anthropometry. Physical status: the use and interpretation of anthropometry: report of a WHO expert committee. WHO technical report series, 854. Geneva: WHO
Chumlea WC, Guo SS, Steinbaugh ML (1994) Prediction of stature from knee height for black and white adults and children with application to mobility-impaired or handicapped persons. J Am Diet Assoc 94(12):1385–1388. https://doi.org/10.1016/0002-8223(94)92540-2. (1391; quiz 1389-90)
Engle WA, American Academy of Pediatrics Committee on Fetus and Newborn (2004) Age terminology during the perinatal period. Pediatrics 114(5):1362–1364. https://doi.org/10.1542/peds.2004-1915
Frisancho AR (1981) New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr 34(11):2540–2545. https://doi.org/10.1093/ajcn/34.11.2540
World Health Organization (WHO) (2006) WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: WHO
World Health Organization (WHO) (2007) WHO child growth standards: head circumference-for-age, arm circumference-for-age, triceps skinfold-for-age and subscapular skinfold-for-age: methods and development. Geneva: WHO
Mehta NM, Compher C, A.S.P.E.N. Board of Directors (2009) A.S.P.E.N Clinical Guidelines: nutrition support of the critically ill child. JPEN J Parenter Enteral Nutr. 33(3):260–276. https://doi.org/10.1177/0148607109333114
Joffe A, Anton N, Lequier L, Vandermeer B, Tjosvold L, Larsen B, Hartling L (2016) Nutritional support for critically ill children. Cochrane Database Syst Rev 5:e005144. https://doi.org/10.1002/14651858.CD005144.pub3
Jimenez L, Mehta NM, Duggan CP (2017) Timing of the initiation of parenteral nutrition in critically ill children. Curr Opin Clin Nutr Metab Care 20(3):227–231. https://doi.org/10.1097/MCO.0000000000000369
Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, Heyland DK (2009) The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 35(10):1728–1737. https://doi.org/10.1007/s00134-009-1567-4.Erratum.In:IntensiveCareMed.2009Oct;35(10):1821
Greathouse KC, Sakellaris KT, Tumin D, Katsnelson J, Tobias JD, Hayes D Jr, Yates AR (2018) Impact of early initiation of enteral nutrition on survival during pediatric extracorporeal membrane oxygenation. JPEN J Parenter Enteral Nutr 42(1):205–211. https://doi.org/10.1002/jpen.1032
Srinivasan V, Hasbani NR, Mehta NM, Irving SY, Kandil SB, Allen HC, Typpo KV, Cvijanovich NZ, Faustino EVS, Wypij D, Agus MSD, Nadkarni VM, Heart and Lung Failure-Pediatric Insulin Titration (HALF-PINT) Study Investigators (2020) Early enteral nutrition is associated with improved clinical outcomes in critically ill children: a secondary analysis of nutrition support in the heart and lung failure-pediatric insulin titration trial. Pediatr Crit Care Med. 21(3):213–221. https://doi.org/10.1097/PCC.0000000000002135
Slater MB, Gruneir A, Rochon PA, Howard AW, Koren G, Parshuram CS (2016) Risk factors of acute kidney injury in critically ill children. Pediatr Crit Care Med 17(9):e391-398. https://doi.org/10.1097/PCC.0000000000000859
Chang JW, Jeng MJ, Yang LY, Chen TJ, Chiang SC, Soong WJ, Wu KG, Lee YS, Wang HH, Yang CF, Tsai HL (2015) The epidemiology and prognostic factors of mortality in critically ill children with acute kidney injury in Taiwan. Kidney Int 87(3):632–639. https://doi.org/10.1038/ki.2014.299
Schrier RW (2010) Fluid administration in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol 5(4):733–739. https://doi.org/10.2215/CJN.00060110. (Epub 2010 Feb 18)
Ostermann M, Straaten HMO, Forni LG (2015) Fluid overload and acute kidney injury: cause or consequence? Crit Care 19:443. https://doi.org/10.1186/s13054-015-1163-7
Li Y, Wang J, Bai Z, Chen J, Wang X, Pan J, Li X, Feng X (2016) Early fluid overload is associated with acute kidney injury and PICU mortality in critically ill children. Eur J Pediatr 175(1):39–48. https://doi.org/10.1007/s00431-015-2592-7
Wiedermann CJ, Wiedermann W, Joannidis M (2010) Hypoalbuminemia and acute kidney injury: a meta-analysis of observational clinical studies. Intensive Care Med 36(10):1657–1665. https://doi.org/10.1007/s00134-010-1928-z. (Erratum in: Intensive Care Med. 2021 Feb;47(2):262)
Mehta P, Sinha A, Sami A, Hari P, Kalaivani M, Gulati A, Kabra M, Kabra SK, Lodha R, Bagga A (2012) Incidence of acute kidney injury in hospitalized children. Indian Pediatr 49(7):537–542. https://doi.org/10.1007/s13312-012-0121-6
Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM, PiñeresOlave BE, Hassinger AB, Szczepanska M, Deep A, Williams D, Sapru A, Roy JA, Nadkarni VM, Thomas NJ, Weiss SL, Furth S, Sepsis PRevalence, OUtcomes, and Therapies Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network (2016) Acute kidney injury in pediatric severe sepsis: an independent risk factor for death and new disability. Crit Care Med 44(12):2241–2250. https://doi.org/10.1097/CCM.0000000000002007
Mehta NM, Corkins MR, Lyman B et al (2013) Defining pediatric malnutrition: a paradigm shift toward etiology-related definitions. J Parenter Enter Nutr 37(4):460–481. https://doi.org/10.1177/0148607113479972
Modi P, Nasrin S, Hawes M et al (2015) Midupper arm circumference outperforms weight-based measures of nutritional status in children with Diarrhea. J Nutr 145(7):1582–1587. https://doi.org/10.3945/jn.114.209718
Funding
None.
Author information
Authors and Affiliations
Contributions
Ana Luiza Cim Ribeiro de Souza, Alberto Piovezani, Julia Carvalho Ventura, Maria Goretti Moreira Guimarães Penido, Nilzete Liberato Bresolin and Yara Maria Franco Moreno, were responsible and approved the research idea, study design, data acquisition, supervision or mentorship, article writing and the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest between the investigators and the patients, and other institutions.
Ethical approval
This study is part of a national multicenter project of pediatric ICUs with the aim of identifying nutritional and clinical variables that predict nutritional status deterioration—PICU-ScREEN Study (Pediatric Intensive Care Unit Score of Risk for Early prEdiction of Nutritional deterioration). The PICU-ScREEN study was approved by the local Institutional Review Board (no 2.471.812) and the Joana de Gusmão Children’s Hospital (no 2.714.446). The present study was approved by the local Institutional Review Board of the same Hospital (no 4.443.316).
Human and animal rights
The study including human participants has been performed in the accordance with the Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from the parents or guardians of all the patients enrolled in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro de Souza, A.L.C., Piovezani, A., Ventura, J.C. et al. Nutritional and clinical factors associated with acute kidney injury development in critically ill children. J Nephrol 36, 2601–2611 (2023). https://doi.org/10.1007/s40620-023-01787-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01787-6