Abstract
Sustained low-efficiency dialysis is a hybrid form of kidney replacement therapy that has gained increasing popularity as an alternative to continuous forms of kidney replacement therapy in intensive care unit settings. During the COVID-19 pandemic, the shortage of continuous kidney replacement therapy equipment led to increasing usage of sustained low-efficiency dialysis as an alternative treatment for acute kidney injury. Sustained low-efficiency dialysis is an efficient method for treating hemodynamically unstable patients and is quite widely available, making it especially useful in resource-limited settings. In this review, we aim to discuss the various attributes of sustained low-efficiency dialysis and how it is comparable to continuous kidney replacement therapy in efficacy, in terms of solute kinetics and urea clearance, and the various formulae used to compare intermittent and continuous forms of kidney replacement therapy, along with hemodynamic stability. During the COVID-19 pandemic, there was increased clotting of continuous kidney replacement therapy circuits, which led to increased use of sustained low-efficiency dialysis alone or together with extra corporeal membrane oxygenation circuits. Although sustained low-efficiency dialysis can be delivered with continuous kidney replacement therapy machines, most centers use standard hemodialysis machines or batch dialysis systems. Even though antibiotic dosing differs between continuous kidney replacement therapy and sustained low-efficiency dialysis, reports of patient survival and renal recovery are similar for continuous kidney replacement therapy and sustained low-efficiency dialysis. Health care studies indicate that sustained low-efficiency dialysis has emerged as a cost-effective alternative to continuous kidney replacement therapy. Although there is considerable data to support sustained low-efficiency dialysis treatments for critically ill adult patients with acute kidney injury, there are fewer pediatric data, even so, currently available studies support the use of sustained low-efficiency dialysis for pediatric patients, particularly in resource-limited settings.
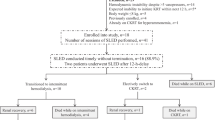
Graphical abstract



Similar content being viewed by others
Data availability
Not applicable.
References
Mittel AM et al (2021) Logistical considerations and clinical outcomes associated with converting operating rooms into an intensive care unit during the coronavirus disease 2019 pandemic in a New York city hospital. Anesth Analg 132(5):1182–1190
John S, Eckardt K (2007) Renal replacement strategies in the ICU. Chest 132(4):1379–1388
Berbece AN, Richardson RM (2006) Sustained low-efficiency dialysis in the ICU: cost, anticoagulation, and solute removal. Kidney Int 70(5):963–968
Tolwani AJ, Wheeler TS, Wille KM (2007) Sustained low-efficiency dialysis. Contrib Nephrol 156:320–324
Fliser D, Kielstein JT (2006) Technology insight: treatment of renal failure in the intensive care unit with extended dialysis. Nat Clin Pract Nephrol 2(1):32–39
Cullis B et al (2014) Peritoneal dialysis for acute kidney injury. Perit Dial Int 34(5):494–517
Ponce D et al (2013) A randomized clinical trial of high volume peritoneal dialysis versus extended daily hemodialysis for acute kidney injury patients. Int Urol Nephrol 45(3):869–878
Datt B et al (2017) To compare acute peritoneal dialysis with sustained low-efficiency dialysis in critically ill patients requiring renal replacement therapy. Indian J Nephrol 27(5):412–413
Marshall MR et al (2001) Sustained low-efficiency dialysis for critically ill patients requiring renal replacement therapy. Kidney Int 60(2):777–785
Brown P, Battistella M (2020) Principles of drug dosing in sustained low efficiency dialysis (SLED) and review of antimicrobial dosing literature. Pharmacy (Basel) 8(1):33
Demirjian SG, Teixeira JP (2021) Optimizing kidney replacement in critical care: SLED can play a bigger role in the ICU. Supp Feat Nephrol Time 13(3)
Morris PE et al (2008) Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 36(8):2238–2243
Liao Z et al (2003) Kinetic comparison of different acute dialysis therapies. Artif Organs 27(9):802–807
Gotch F (1995) Kinetic modeling in hemodialysis. In: Nissenson A, Fine R, Gentile D, Norwalk CT (eds) Clinical dialysis, 3rd edn. Appleton & Lange, pp 156–188
Clark WR et al (1999) Quantifying the effect of changes in the hemodialysis prescription on effective solute removal with a mathematical model. J Am Soc Nephrol 10(3):601–609
Clark WR et al (1994) A comparison of metabolic control by continuous and intermittent therapies in acute renal failure. J Am Soc Nephrol 4(7):1413–1420
Casino FG, Marshall MR (2004) Simple and accurate quantification of dialysis in acute renal failure patients during either urea non-steady state or treatment with irregular or continuous schedules. Nephrol Dial Transplant 19(6):1454–1466
Casino FG, Lopez T (1996) The equivalent renal urea clearance: a new parameter to assess dialysis dose. Nephrol Dial Transplant 11(8):1574–1581
Marshall MR et al (2002) Urea kinetics during sustained low-efficiency dialysis in critically ill patients requiring renal replacement therapy. Am J Kidney Dis 39(3):556–570
Sargent JA, Gotch FA (1996) Principles and biophysics of dialysis. Replacement of renal function by dialysis. Springer, pp 34–102
Marshall MR et al (2004) Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant 19(4):877–884
Schlaeper C et al (1999) High clearance continuous renal replacement therapy with a modified dialysis machine. Kidney Int Suppl 72:S20–S23
Schwenger V et al (2012) Sustained low efficiency dialysis using a single-pass batch system in acute kidney injury—a randomized interventional trial: the renal replacement therapy study in intensive care unit patients. Crit Care 16(4):R140
Sethi SK et al (2018) Feasibility of sustained low efficiency dialysis in critically sick pediatric patients: a multicentric retrospective study. Hemodial Int 22(2):228–234
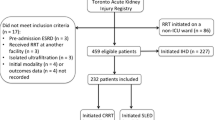
Kitchlu A et al (2015) Outcomes of sustained low efficiency dialysis versus continuous renal replacement therapy in critically ill adults with acute kidney injury: a cohort study. BMC Nephrol 16:127
Dalbhi SA et al (2021) Sustained low efficiency dialysis is non-inferior to continuous renal replacement therapy in critically ill patients with acute kidney injury: a comparative meta-analysis. Medicine (Baltimore) 100(51):e28118
Fieghen HE et al (2010) The hemodynamic tolerability and feasibility of sustained low efficiency dialysis in the management of critically ill patients with acute kidney injury. BMC Nephrol 11:32
Sethi SK et al (2018) Heparin free dialysis in critically sick children using sustained low efficiency dialysis (SLEDD-f): a new hybrid therapy for dialysis in developing world. PLoS ONE 13(4):e0195536
Robert R et al (2012) Benefits of an early cooling phase in continuous renal replacement therapy for ICU patients. Ann Intensive Care 2(1):40
Mustafa RA et al (2016) Effect of lowering the dialysate temperature in chronic hemodialysis: a systematic review and meta-analysis. Clin J Am Soc Nephrol 11(3):442–457
Regolisti G et al (2017) Treatment of metformin intoxication complicated by lactic acidosis and acute kidney injury: the role of prolonged intermittent hemodialysis. Am J Kidney Dis 70(2):290–296
Greco P et al (2019) Sustained low-efficiency dialysis for metformin-associated lactic acidosis in patients with acute kidney injury. J Nephrol 32(2):297–306
Lobo V (2018) Sustained low-efficiency dialysis (SLED) and hybrid therapies in children. In: Deep A, Goldstein SL (eds) Critical care nephrology and renal replacement therapy in children. Springer International Publishing, Cham, pp 291–306
Lonnemann G et al (2000) Extended daily veno-venous high-flux haemodialysis in patients with acute renal failure and multiple organ dysfunction syndrome using a single path batch dialysis system. Nephrol Dial Transplant 15(8):1189–1193
Dhondt A et al (2005) Dialysate partitioning in the genius batch hemodialysis system: effect of temperature and solute concentration. Kidney Int 67(6):2470–2476
Fassbinder W (2003) Experience with the GENIUS hemodialysis system. Kidney Blood Press Res 26(2):96–99
Polaschegg H-D (2010) Hemodialysis machine technology: a global overview. Expert Rev Med Devices 7(6):793–810
Therapy Handbook NxStage® Hemodialysis Treatment (2019) NxStage Medical, Inc.
(2022) Available from: https://www.baxter.com/sites/g/files/ebysai746/files/2017-11/Prismaflex-07.11-Brochure-New_Accts.pdf.
Overview of Prismaflex and Prismax. LHSC (2023) Available from: https://www.lhsc.on.ca/critical-care-trauma-centre/overview-of-prismaflex-and-prismax.
Vinsonneau C et al (2015) Renal replacement therapy in adult and pediatric intensive care : recommendations by an expert panel from the French intensive care society (SRLF) with the French society of anesthesia intensive care (SFAR) French group for pediatric intensive care emergencies (GFRUP) the French dialysis society (SFD). Ann Intensive Care 5(1):58
Ponce D et al (2012) High-volume peritoneal dialysis in acute kidney injury: indications and limitations. Clin J Am Soc Nephrol 7(6):887–894
Sutherland SM et al (2010) Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis 55(2):316–325
Bunchman TE, Donckerwolcke RA (1994) Continuous arterial-venous diahemofiltration and continuous veno-venous diahemofiltration in infants and children. Pediatr Nephrol 8(1):96–102
Raina R et al (2017) Treatment of AKI in developing and developed countries: an international survey of pediatric dialysis modalities. PLoS ONE 12(5):e0178233
Sethi SK et al (2020) Pediatric continuous renal replacement therapy (PCRRT) expert committee recommendation on prescribing prolonged intermittent renal replacement therapy (PIRRT) in critically ill children. Hemodial Int 24(2):237–251
Di Mario F et al (2022) Hypophosphatemia in critically ill patients undergoing sustained low-efficiency dialysis with standard dialysis solutions. Nephrol Dial Transplant 37(12):2505–2513
Di Mario F et al (2021) Prevention of hypomagnesemia in critically ill patients with acute kidney injury on continuous kidney replacement therapy: the role of early supplementation and close monitoring. J Nephrol 34(4):1271–1279
Caires RA et al (2016) Sustained low-efficiency extended dialysis (SLED) with single-pass batch system in critically-ill patients with acute kidney injury (AKI). J Nephrol 29(3):401–409
Gritters M et al (2006) Citrate anticoagulation abolishes degranulation of polymorphonuclear cells and platelets and reduces oxidative stress during haemodialysis. Nephrol Dial Transplant 21(1):153–159
Finkel KW, Foringer JR (2005) Safety of regional citrate anticoagulation for continuous sustained low efficiency dialysis (C-SLED) in critically ill patients. Ren Fail 27(5):541–545
Doidge JC et al (2022) Regional citrate anticoagulation versus systemic heparin anticoagulation for continuous kidney replacement therapy in intensive care. J Crit Care 74:154218
Chadha V et al (2002) Citrate clearance in children receiving continuous venovenous renal replacement therapy. Pediatr Nephrol 17(10):819–824
Davenport A, Tolwani A (2009) Citrate anticoagulation for continuous renal replacement therapy (CRRT) in patients with acute kidney injury admitted to the intensive care unit. NDT Plus 2(6):439–447
Fiaccadori E et al (2013) Efficacy and safety of a citrate-based protocol for sustained low-efficiency dialysis in AKI using standard dialysis equipment. Clin J Am Soc Nephrol 8(10):1670–1678
Wen M et al (2018) A novel citrate-based protocol versus heparin anticoagulation for sustained low-efficiency dialysis in the ICU: safety, efficacy, and cost. BMC Nephrol 19(1):79
Makdisi G, Wang IW (2015) Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J Thorac Dis 7(7):E166–E176
Arnold F et al (2022) Integration of sustained low-efficiency dialysis into extracorporeal membrane oxygenation circuit in critically ill COVID-19 patients: a feasibility study. Artif Organs 46(9):1847–1855
Álvarez-Lerma F, Grau S (2012) Management of antimicrobial use in the intensive care unit. Drugs 72(4):447–470
Verbeeck RK, Musuamba FT (2009) Pharmacokinetics and dosage adjustment in patients with renal dysfunction. Eur J Clin Pharmacol 65(8):757–773
Thompson A, Li F, Gross AK (2017) Considerations for medication management and anticoagulation during continuous renal replacement therapy. AACN Adv Crit Care 28(1):51–63
Edrees F, Li T, Vijayan A (2016) Prolonged intermittent renal replacement therapy. Adv Chronic Kidney Dis 23(3):195–202
Pourcine F et al (2021) Sustained low-efficiency dialysis with regional citrate anticoagulation for patients with liver impairment in intensive care unit: a single-center experience. Ther Apher Dial 25(2):211–217
Mueller BA, Scoville BA (2012) Adding to the armamentarium: antibiotic dosing in extended dialysis. Clin J Am Soc Nephrol 7(3):373–375
Harvey AK et al (2021) Short-and long-term outcomes of sustained low efficiency dialysis vs continuous renal replacement therapy in critically ill patients with acute kidney injury. J Crit Care 62:76–81
Abe M et al (2010) Comparison of sustained hemodiafiltration with continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Artif Organs 34(4):331–338
Wu VC et al (2010) Sustained low-efficiency dialysis versus continuous veno-venous hemofiltration for postsurgical acute renal failure. Am J Surg 199(4):466–476
Abe M et al (2011) Comparison of sustained hemodiafiltration with acetate-free dialysate and continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Int J Nephrol 2011:432094
Chen X, Ma T (2014) Sustained low-efficiency daily diafiltration for diabetic nephropathy patients with acute kidney injury. Med Princ Pract 23(2):119–124
Sun Z et al (2014) Continuous venovenous hemofiltration versus extended daily hemofiltration in patients with septic acute kidney injury: a retrospective cohort study. Crit Care 18(2):R70
Badawy S, Hassan A, Samir E (2013) A prospective randomized comparative pilot trial on extended daily dialysis versus continuous venovenous hemodiafiltration in acute kidney injury after cardiac surgery. Egyptian J Cardiothorac Anesth 7(2):69–73
Alam MG, Marshall MR, Shaver MJ, Chatoth DK (2000) Cost comparison between sustained low efficiency hemodialysis (SLED) and continuous venovenous hemofiltration (CVVH) for ICU patients with ARF. Am J Kidney Dis 35(4):A9–A9
Monchi M et al (2004) Citrate vs heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med 30(2):260–265
Kutsogiannis DJ et al (2005) Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int 67(6):2361–2367
Keene AB et al (2021) Critical care surge during the COVID-19 pandemic: implementation and feedback from frontline providers. J Intensive Care Med 36(2):233–240
Helms J et al (2020) High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 46(6):1089–1098
Lee CY, Yeh HC, Lin CY (2012) Treatment of critically ill children with kidney injury by sustained low-efficiency daily diafiltration. Pediatr Nephrol 27(12):2301–2309
Di Mario F et al (2021) Sustained low-efficiency dialysis with regional citrate anticoagulation in critically ill patients with COVID-19 associated AKI: a pilot study. J Crit Care 63:22–25
Zhang L et al (2015) Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis 66(2):322–330
Moura EIM et al (2021) Efficacy and safety of regional anticoagulation with 4% trisodium citrate versus heparin in extended hemodialysis among critical patients with cancer and acute kidney injury. Blood Purif 50(1):50–56
Funding
There were no funding sources for this article.
Author information
Authors and Affiliations
Contributions
SKS and GM conceptualized the manuscript. SKS, GM, AS, ABM, RPF, AD, RS, RR wrote the manuscript. AD, SKS, and RR critically reviewed and edited the manuscript. RS created the graphical abstract.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sethi, S., Mangat, G., Soundararajan, A. et al. Archetypal sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring kidney replacement therapy: towards an adequate therapy. J Nephrol 36, 1789–1804 (2023). https://doi.org/10.1007/s40620-023-01665-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01665-1