Abstract
Background
Kidney transplantation—associated mineral and bone disorder (KT-MBD) still represents a black box on the long-term due to scarce available data. We aimed to investigate the impact of non-classical bone regulating factors (body composition, adipokines, inflammatory markers, fibroblast growth factor 23—FGF23 and α-Klotho) in long-standing kidney transplant (KT) recipients compared to the general population.
Methods
Our cross-sectional study, enrolling 59 KT patients and age, sex and body mass index—matched healthy general population volunteers, assessed the predictive role of the body composition, serum adipokines (leptin, adiponectin, resistin), inflammatory markers (erythrocyte sedimentation rate, C-reactive protein) and parathyroid hormone (PTH)—FGF23/α-Klotho axis upon bone mineral density (BMD) and osteocalcin, using correlation and linear multiple regression.
Results
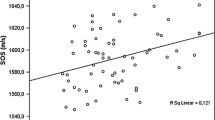
The 59 KT recipients (mean transplantation span of 57.7 ± 7.2 months) had similar body composition but significantly lower BMD (p < 0.01) compared to the general population group. Total lean mass was independently associated with BMD in both groups. In KT patients, age, time spent on dialysis and PTH were the main negative independent predictors of BMD, after adjusting for possible confounders. Resistin and α-Klotho also negatively predicted lumbar bone density (p < 0.001), while adiponectin and α-Klotho positively predicted osteocalcin levels (p < 0.001) in KT recipients, independently of inflammatory markers. No significant associations were found between FGF23 and bone parameters in any of the groups.
Conclusions
Age, PTH, time on dialysis and lean mass are among the main bone density predictors in long-standing KT patients. The bone impact of adipokine dysregulation and of α-Klotho merits further investigations in KT-MBD. Preserving lean mass for improved bone outcomes should be part of KT-MBD management on the long-term.
Graphic abstract



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Delos Santos R, Rossi A, Coyne D, Maw TT (2019) Management of post-transplant hyperparathyroidism and bone disease. Drugs 79:501–513. https://doi.org/10.1007/s40265-019-01074-4
Altman AM, Sprague SM (2018) Mineral and bone disease in kidney transplant recipients. Curr Osteoporos Rep 16:703–711. https://doi.org/10.1007/s11914-018-0490-4
Natacha R, Filipe R, Alice S, Pedro N (2019) The bone in renal transplant recipients-a nephrological and orthopedic review. Int J Transplant Res Med 5:045. https://doi.org/10.23937/2572-4045.1510045
Fattahi MR, Niknam R, Shams M et al (2019) The association between prolonged proton pump inhibitors use and bone mineral density. Risk Manag Healthc Policy 12:349–355. https://doi.org/10.2147/RMHP.S223118
Castiglioni S, Cazzaniga A, Albisetti W, Maier JAM (2013) Magnesium and osteoporosis: Current state of knowledge and future research directions. Nutrients 5:3022–3033
Giannini S, D’Angelo A, Carraro G et al (2001) Persistently increased bone turnover and low bone density in long-term survivors to kidney transplantation. Clin Nephrol 56:353–363
dos Santos VR, Christofaro DGD, Gomes IC et al (2018) Relationship between obesity, sarcopenia, sarcopenic obesity, and bone mineral density in elderly subjects aged 80 years and over. Rev Bras Ortop English Ed 53:300–305. https://doi.org/10.1016/j.rboe.2017.09.002
Johansen KL, Lee C (2015) Body composition in chronic kidney disease. Curr Opin Nephrol Hypertens 24:268–275. https://doi.org/10.1097/MNH.0000000000000120
Schütz T, Hudjetz H, Roske AE et al (2012) Weight gain in long-term survivors of kidney or liver transplantation-Another paradigm of sarcopenic obesity? Nutrition 28:378–383. https://doi.org/10.1016/j.nut.2011.07.019
Bilha SC, Branisteanu D, Buzduga C et al (2018) Modifications in the spectrum of bone mass predictive factors with menopausal status. Endocr Res 43:176–185. https://doi.org/10.1080/07435800.2018.1448991
Mansell H, Rosaasen N, Dean J, Shoker A (2013) Evidence of enhanced systemic inflammation in stable kidney transplant recipients with low Framingham risk scores. Clin Transplant 27:E391–E399. https://doi.org/10.1111/ctr.12159
Kirk B, Feehan J, Lombardi G, Duque G (2020) Muscle and bone (a bonetto and m brotto, section editors) muscle, bone, and fat crosstalk: the biological role of myokines, osteokines, and adipokines. Curr Osteoporos Rep 18:388–400
Kanaan N, Claes K, Devogelaer JP et al (2010) Fibroblast growth factor-23 and parathyroid hormone are associated with post-transplant bone mineral density loss. Clin J Am Soc Nephrol 5:1887–1892. https://doi.org/10.2215/CJN.00950110
Ozdem S, Yilmaz VT, Ozdem SS et al (2015) Is Klotho F352V polymorphism the missing piece of the bone loss puzzle in renal transplant recipients? Pharmacology 95:271–278. https://doi.org/10.1159/000398812
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Hansen D, Rasmussen K, Danielsen H et al (2011) No difference between alfacalcidol and paricalcitol in the treatment of secondary hyperparathyroidism in hemodialysis patients: a randomized crossover trial. Kidney Int 80:841–850. https://doi.org/10.1038/ki.2011.226
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on Bone Densitometry. J Clin Densitom 16:455–466. https://doi.org/10.1016/j.jocd.2013.08.004
Chumlea WC, Cesari M, Evans WJ et al (2011) International working group on Sarcopenia. J Nutr Heal Aging 15:450–455. https://doi.org/10.1007/s12603-011-0092-7
Yanishi M, Kinoshita H, Tsukaguchi H et al (2018) Factors related to osteosarcopenia in kidney transplant recipients. Transplant Proc 50:3371–3375. https://doi.org/10.1016/j.transproceed.2018.04.032
Ho-Pham LT, Nguyen UD, Nguyen TV (2014) Association between lean mass, fat mass, and bone mineral density: a meta-analysis. J Clin Endocrinol Metab 99:30–38. https://doi.org/10.1210/jc.2013-319010.1210/jc.2014-v99i12-30A
Žofková I (2008) Hormonal aspects of the muscle-bone unit. Physiol Res 57(Suppl. 1):S159–S169
Zhu Q, Scherer PE (2018) Immunologic and endocrine functions of adipose tissue: implications for kidney disease. Nat Rev Nephrol 14:105–120. https://doi.org/10.1038/nrneph.2017.157
Van Atteveld VA, Van Ancum JM, Reijnierse EM et al (2019) Erythrocyte sedimentation rate and albumin as markers of inflammation are associated with measures of sarcopenia: a cross-sectional study. BMC Geriatr 19:233. https://doi.org/10.1186/s12877-019-1253-5
Singh M, Arora S, Kaur A et al (2018) Patterns of age- and sex-related variations in bone mineral density of lumbar spine and total femur: a retrospective diagnostic laboratory-based study. J Midlife Health 9:155–161. https://doi.org/10.4103/jmh.JMH_95_18
Adami G, Saag KG (2019) Glucocorticoid-induced osteoporosis: 2019 concise clinical review. Osteoporos Int 30:1145–1156
Iyer SP, Nikkel LE, Nishiyama KK et al (2014) Kidney transplantation with early corticosteroid withdrawal: paradoxical effects at the central and peripheral skeleton. J Am Soc Nephrol 25:1331–1341. https://doi.org/10.1681/ASN.2013080851
Liu J, Li X, Fan L et al (2019) Proton pump inhibitors therapy and risk of bone diseases: an update meta-analysis. Life Sci 218:213–223. https://doi.org/10.1016/j.lfs.2018.12.058
Carrillo-López N, Panizo S, Alonso-Montes C et al (2016) Direct inhibition of osteoblastic Wnt pathway by fibroblast growth factor 23 contributes to bone loss in chronic kidney disease. Kidney Int 90:77–89. https://doi.org/10.1016/j.kint.2016.01.024
Erben RG, Andrukhova O (2017) FGF23-Klotho signaling axis in the kidney. Bone 100:62–68
Komaba H, Kaludjerovic J, Hu DZ et al (2017) Klotho expression in osteocytes regulates bone metabolism and controls bone formation. Kidney Int 92:599–611. https://doi.org/10.1016/j.kint.2017.02.014
Haussler MR, Whitfield GK, Kaneko I et al (2012) The role of vitamin D in the FGF23, klotho, and phosphate bone-kidney endocrine axis. Rev Endocr Metab Disord 13:57–69
Nagaraju SP, Rhee CM, Mathe Z, Molnar MZ (2016) Adipocytokines in renal transplant recipients Kristof Nagy1. Clin Kidney J 9:359–373. https://doi.org/10.1093/ckj/sfv156
Naot D, Musson DS, Cornish J (2017) The activity of adiponectin in bone. Calcif Tissue Int 100:486–499. https://doi.org/10.1007/s00223-016-0216-5
Bacchetta J, Boutroy S, Guebre-Egziabher F et al (2009) The relationship between adipokines, osteocalcin and bone quality in chronic kidney disease. Nephrol Dial Transplant 24:3120–3125. https://doi.org/10.1093/ndt/gfp262
Marchelek-Myśliwiec M, Dziedziejko V, Nowosiad-Magda M et al (2019) Bone metabolism parameters in hemodialysis patients with chronic kidney disease and in patients after kidney transplantation. Physiol Res 68:947–954. https://doi.org/10.33549/physiolres.934118
Wang Y, Zhang X, Shao J et al (2017) Adiponectin regulates BMSC osteogenic differentiation and osteogenesis through the Wnt/β-catenin pathway. Sci Rep 7:1–13. https://doi.org/10.1038/s41598-017-03899-z
Chen XX, Yang T (2015) Roles of leptin in bone metabolism and bone diseases. J Bone Miner Metab 33:474–485. https://doi.org/10.1007/s00774-014-0569-7
Ghorban-Sabbagh M, Nazemian F, Naghibi M et al (2016) Correlation between serum leptin and bone mineral density in hemodialysis patients. J Ren Inj Prev 5:112–117. https://doi.org/10.15171/jrip.2016.24
Malyszko J, Malyszko JS, Pawlak K, Mysliwiec M (2006) Resistin, a new adipokine, is related to inflammation and renal function in kidney allograft recipients. Transplant Proc 38:3434–3436. https://doi.org/10.1016/j.transproceed.2006.10.140
Oh KW, Lee WY, Rhee EJ et al (2005) The relationship between serum resistin, leptin, adiponectin, ghrelin levels and bone mineral density in middle-aged men. Clin Endocrinol (Oxf) 63:131–138. https://doi.org/10.1111/j.1365-2265.2005.02312.x
Mermerci Başkan B, Pekin Doğan Y, Sivas F et al (2010) The relation between osteoporosis and vitamin D levels and disease activity in ankylosing spondylitis. Rheumatol Int 30:375–381. https://doi.org/10.1007/s00296-009-0975-7
Siggelkow H, Cortis J, Claus C et al (2009) Erythrocyte sedimentation rate as an osteoporosis risk factor in patients with active Crohn’s disease. Osteologie 18:209–216. https://doi.org/10.1055/s-0037-1619894
Wang T, He C (2019) TNF-α and IL-6: the link between immune and bone system. Curr Drug Targets 21:213–227. https://doi.org/10.2174/1389450120666190821161259
Fargnoli JL, Sun Q, Olenczuk D et al (2010) Resistin is associated with biomarkers of inflammation while total and high-molecular weight adiponectin are associated with biomarkers of inflammation, insulin resistance, and endothelial function. Eur J Endocrinol 162:281–288. https://doi.org/10.1530/EJE-09-0555
Akaberi S, Simonsen O, Lindergård B, Nyberg G (2008) Can DXA predict fractures in renal transplant patients? Am J Transplant 8:2647–2651. https://doi.org/10.1111/j.1600-6143.2008.02423.x
Acknowledgements
We are grateful to Mr. Valentin Zaharia and Mr. Adrian Aancute for excellent technical assistance.
Funding
This work was financed by the “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania under an internal Grant [27494/20.12.2018].
Author information
Authors and Affiliations
Contributions
AM and SCB contributed to the research design and performance, data analysis and writing of the paper. DC and MPT performed laboratory determinations and data analysis. PC performed laboratory determinations and revised the paper. AC and DDB performed the research design, drafted and revised the paper. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study adhered to the Declaration of Helsinki and the Declaration of Istanbul. The institutional ethics committee approved the protocol (20.03.2019).
Consent to participate
All individual participants gave written informed consent before entering the study.
Consent for publication
All individual participants gave written informed consent regarding publishing their data before entering the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matei, A., Bilha, S.C., Constantinescu, D. et al. Body composition, adipokines, FGF23-Klotho and bone in kidney transplantation: Is there a link?. J Nephrol 35, 293–304 (2022). https://doi.org/10.1007/s40620-021-00972-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-021-00972-9