Abstract
Introduction
Since inflammation alters vascular permeability, including vascular permeability in the lung, we hypothesized that it can be an amplifier of lung congestion in a category of patients at high risk for pulmonary oedema like end stage kidney disease (ESKD) patients.
Objective and methods
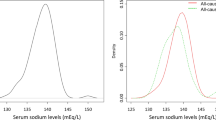
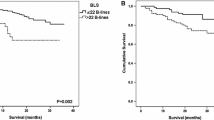
We investigated the effect modification by systemic inflammation (serum CRP) on the relationship between a surrogate of the filling pressure of the LV [left atrial volume indexed to the body surface area (LAVI)] and lung water in a series of 220 ESKD patients. Lung water was quantified by the number of ultrasound B lines (US-B) on lung US. Six-hundred and three recordings were performed during a 2-year follow up. Longitudinal data analysis was made by the Mixed Linear Model.
Results
At baseline, 88 had absent, 101 had mild to moderate lung congestion and 31 severe congestion. The number of US B lines associated with LAVI (r = 0.23, P < 0.001) and serum CRP was a robust modifier of this relationship (P < 0.001). Similarly, in fully adjusted longitudinal analyses US-B lines associated with simultaneous estimates of LAVI (P = 0.002) and again CRP was a strong modifier of this relationship in adjusted analyses (P ≤ 0.01). Overall, at comparable LAVI levels, lung congestion was more pronounced in inflamed than in non-inflamed patients.
Conclusion
In ESKD systemic inflammation is a modifier of the relationship between LAVI, an integrate measure of LV filling pressure, and lung water. For any given pressure, lung water is increased with higher CRP levels, likely reflecting a higher permeability of the alveolar-capillary barrier.


Similar content being viewed by others
References
Noble VE, Murray AF, Capp R et al (2009) Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest 135:1433–1439. https://doi.org/10.1378/chest.08-1811
Mallamaci F, Benedetto FA, Tripepi R et al (2010) Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging 3:586–594. https://doi.org/10.1016/j.jcmg.2010.02.005
Zoccali C, Tripepi R, Torino C et al (2014) Lung congestion as a risk factor in end-stage renal disease. Blood Purif 36:184–191. https://doi.org/10.1159/000356085
Enia G, Torino C, Panuccio V et al (2013) Asymptomatic pulmonary congestion and physical functioning in hemodialysis patients. Clin J Am Soc Nephrol 8:1343–1348. https://doi.org/10.2215/CJN.11111012
Zoccali C, Puntorieri E, Mallamaci F (2013) Lung congestion as a hidden threat in end-stage kidney disease: a call to action. Nephrol Dial Transplant 28:2657–2660. https://doi.org/10.1093/ndt/gft425
Covic A, Siriopol D, Voroneanu L (2018) Use of lung ultrasound for the assessment of volume status in CKD. Am J Kidney Dis 71:412–422. https://doi.org/10.1053/j.ajkd.2017.10.009
Siriopol D, Hogas S, Voroneanu L et al (2013) Predicting mortality in haemodialysis patients: a comparison between lung ultrasonography, bioimpedance data and echocardiography parameters. Nephrol Dial Transplant 28:2851–2859. https://doi.org/10.1093/ndt/gft260
Zoccali C, Mallamaci F (2018) Mapping progress in reducing cardiovascular risk with kidney disease managing volume overload. Clin J Am Soc Nephrol 13:1432–1434
Zoccali C, Moissl U, Chazot C, Mallamaci F, Tripepi G, Arkossy O, Wabel P (2017) Chronic fluid overload and mortality in end stage kidney disease. J Am Soc Nephrol (in press)
Grootendorst DC, de Jager DJ, Brandenburg VM et al (2007) Excellent agreement between C-reactive protein measurement methods in end-stage renal disease patients no additional power for mortality prediction with high-sensitivity CRP. Nephrol Dial Transplant 22:3277–3284. https://doi.org/10.1093/ndt/gfm381
Stenvinkel P, Wanner C, Metzger T et al (2002) Inflammation and outcome in end-stage renal failure: does female gender constitute a survival advantage? Kidney Int 62:1791–1798. https://doi.org/10.1046/j.1523-1755.2002.00637.x
Zhang W, He J, Zhang F et al (2013) Prognostic role of C-reactive protein and Interleukin-6 in dialysis patients: a systematic review and meta-analysis. J Nephrol 26:243–253. https://doi.org/10.5301/jn.5000169
Dai L, Mukai H, Lindholm B et al (2017) Clinical global assessment of nutritional status as predictor of mortality in chronic kidney disease patients. PLoS One 12:e0186659. https://doi.org/10.1371/journal.pone.0186659
Mehta D, Ravindran K, Kuebler WM (2014) Novel regulators of endothelial barrier function. Am J Physiol Cell Mol Physiol 307:L924–L935. https://doi.org/10.1152/ajplung.00318.2014
Douglas PS (2003) The left atrium: a biomarker of chronic diastolic dysfunction and cardiovascular disease risk. J Am Coll Cardiol 42:1206–1207
Picano E, Scali MC, Ciampi Q, Lichtenstein D (2018) Lung ultrasound for the cardiologist. JACC Cardiovasc Imaging 11:1692–1705. https://doi.org/10.1016/j.jcmg.2018.06.023
Jambrik Z, Monti S, Coppola V et al (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 93:1265–1270. https://doi.org/10.1016/j.amjcard.2004.02.012
Agricola E, Bove T, Oppizzi M et al (2005) “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127:1690–1695. https://doi.org/10.1378/chest.127.5.1690
Frassi F, Gargani L, Gligorova S et al (2007) Clinical and echocardiographic determinants of ultrasound lung comets. Eur J Echocardiogr 8:474–479. https://doi.org/10.1016/j.euje.2006.09.004
Frassi F, Gargani L, Tesorio P et al (2007) Prognostic value of extravascular lung water assessed with ultrasound lung comets by chest sonography in patients with dyspnea and/or chest pain. J Card Fail 13:830–835. https://doi.org/10.1016/j.cardfail.2007.07.003
Sicari R, Gargani L, Wiecek A et al (2013) The use of echocardiography in observational clinical trials: the EURECA-m registry. Nephrol Dial Transplant 28:19–23. https://doi.org/10.1093/ndt/gfs399
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Hear J Cardiovasc Imaging 16:233–271. https://doi.org/10.1093/ehjci/jev014
Parfrey PS, Harnett JD, Griffiths SM et al (1988) Congestive heart failure in dialysis patients. Arch Intern Med 148:1519–1525
Zoccali C (2007) How important is echocardiography for risk stratification in follow-up of patients with chronic kidney disease? Nat Clin Pract Nephrol 3:178–179. https://doi.org/10.1038/ncpneph0441
Zoccali C, Bolignano D, Mallamaci F (2015) Left ventricular hypertrophy in chronic kidney disease. In: Turner NN, Lameire N, Goldsmith DJ, Winearls CG, Himmelfarb J, Remuzzi G, Bennet WG, de Broe ME, Chapman JR, Adrian Covic VJ (eds) Oxord textbook of nephrology, 4th edn. Oxford University Press, Oxford, pp 837–852
Adamson PB, Magalski A, Braunschweig F et al (2003) Ongoing right ventricular hemodynamics in heart failure: clinical value of measurements derived from an implantable monitoring system. J Am Coll Cardiol 41:565–571
Picano E, Pellikka PA (2016) Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J 37:2097–2104. https://doi.org/10.1093/eurheartj/ehw164
Obi Y, Qader H, Kovesdy CP, Kalantar-Zadeh K (2015) Latest consensus and update on protein–energy wasting in chronic kidney disease. Curr Opin Clin Nutr Metab Care 18:254–262. https://doi.org/10.1097/MCO.0000000000000171
Benz K, Hilgers K-F, Daniel C, Amann K (2018) Vascular calcification in chronic kidney disease: the role of inflammation. Int J Nephrol 2018:1–7. https://doi.org/10.1155/2018/4310379
Avila-Díaz M, Ventura M-J, Valle D et al (2016) Inflammation and extracellular volume expansion are related to sodium and water removal in patients on peritoneal dialysis. Perit Dial Int 26:574–580
Rao AK, Djamali A, Korcarz CE et al (2008) Left atrial volume is associated with inflammation and atherosclerosis in patients with kidney disease. Echocardiography 25:264–269. https://doi.org/10.1111/j.1540-8175.2007.00589.x
Robin ED, Thomas ED (1954) Some relations between pulmonary edema and pulmonary inflammation (pneumonia). Arch Intern Med 93:713. https://doi.org/10.1001/archinte.1954.00240290071008
Mann DL (2005) Targeted anticytokine therapy and the failing heart. Am J Cardiol 95:9–16. https://doi.org/10.1016/j.amjcard.2005.03.007
Rashid H, Hashmi SN, Hussain T (2005) Risk factors in high altitude pulmonary oedema. J Coll Phys Surg Pak 15:96–99
Scheel PJ, Liu M, Rabb H (2008) Uremic lung: new insights into a forgotten condition. Kidney Int 74:849–851. https://doi.org/10.1038/ki.2008.390
Mukai H, Ming P, Lindholm B et al (2018) Lung dysfunction and mortality in patients with chronic kidney disease. Kidney Blood Press Res 43:522–535. https://doi.org/10.1159/000488699
Yılmaz S, Yildirim Y, Yilmaz Z et al (2016) Pulmonary function in patients with end-stage renal disease: effects of hemodialysis and fluid overload. Med Sci Monit 22:2779–84. https://doi.org/10.12659/MSM.897480
Klein CL, Hoke TS, Fang W-F et al (2008) Interleukin-6 mediates lung injury following ischemic acute kidney injury or bilateral nephrectomy. Kidney Int 74:901–909. https://doi.org/10.1038/ki.2008.314
Black S, Kushner I, Samols D (2004) C-reactive Protein. J Biol Chem 279:48487–48490. https://doi.org/10.1074/jbc.R400025200
Grobbee DE, Hoes AW (2009) Modifiers and confounders. In: AW GD and H (ed) Clinical epidemiology : principles, methods, and applications for clinical research. Jones and Bartlett Publishers, pp 46–48
Fedak KM, Bernal A, Capshaw ZA, Gross S (2015) Applying the Bradford Hill criteria in the 21st century: how data integration has changed causal inference in molecular epidemiology. Emerg Themes Epidemiol 12:14. https://doi.org/10.1186/s12982-015-0037-4
Arneson TJ, Liu J, Qiu Y et al (2010) Hospital treatment for fluid overload in the medicare hemodialysis population. Clin J Am Soc Nephrol 5:1054–1063. https://doi.org/10.2215/CJN.00340110
Plantinga LC, King LM, Masud T et al (2018) Burden and correlates of readmissions related to pulmonary edema in US hemodialysis patients: a cohort study. Nephrol Dial Transplant 33:1215–1223. https://doi.org/10.1093/ndt/gfx335
Shah T, Newcombe P, Smeeth L et al (2010) Ancestry as a determinant of mean population C-reactive protein values: implications for cardiovascular risk prediction. Circ Cardiovasc Genet 3:436–444. https://doi.org/10.1161/CIRCGENETICS.110.957431
Acknowledgements
This study is part of the scientific activity of the EURECA-m (European Cardiovascular and Renal medicine) working group. The authors are grateful to Sarah Rocchi and Gennaro D’Angelo for their support during the LUST trial, and to Nancy CHRU University Hospital, France, which co-sponsored the trial in the French centres.
Funding
The LUST trial was funded by the European Renal Association-European Dialysis Transplantation Association (ERA-EDTA).
Author information
Authors and Affiliations
Contributions
CZ conceived the idea of the present analysis in the LUST database. CT, GD and GT performed the statistical analysis and CZ participated into the planning of the same analysis. CT and CZ prepared the first draft of the study which was critically read by all co-authors that eventually approved the final version of the manuscript prepared by CT and CZ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study fully complies with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The ethical committees of the Renal Units participating in the LUST trial approved the study protocol. All participants gave informed consent before enrolment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Torino, C., Gargani, L., Sicari, R. et al. Inflammation is an amplifier of lung congestion by high lv filling pressure in hemodialysis patients: a longitudinal study. J Nephrol 33, 583–590 (2020). https://doi.org/10.1007/s40620-019-00696-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-019-00696-x