Abstract
Influenza is a commonly encountered and serious pathogen. Patients with end-stage renal disease are more susceptible to serious morbidity and mortality associated with influenza infection. Proper management of patients includes: vaccination, monitoring for symptoms and isolation of potentially infected patients as well as appropriate antiviral therapies. In some cases of exposure, chemoprophylaxis is warranted. Vaccination and appropriate therapies are associated with improved outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Influenza is a major human pathogen. Seasonal influenza is responsible for thousands of deaths in the United States every year and global pandemics have mortality totals in the millions [1, 2]. Patients with kidney disease, especially end stage renal disease (ESRD), are among the high risk populations for contracting influenza with resulting increased mortality rates [3]. Thus, the ESRD population represents a high priority for influenza vaccination and treatment. This paper will explore rates of influenza, clinical manifestations, vaccination practices and pitfalls and the use of antivirals in the ESRD population.
Influenza: background
Influenza is an eight segment ribonucleic acid virus and the most important member of the orthomyxoviridae family. Flu is classified into A, B, and C subtypes with A and B the primary cause of human seasonal influenza [4]. The major proteins present on the surface of influenza are hemagglutinin (HA), neuraminidase (NA) and the M2 hydrogen ion channel. Each protein has a specialized function. Hemagglutinin mediates cellular entry by binding to human epithelial cell sialic acid receptors. The virus is then endocytosed and the endosome is acidified via proton entry mediated by the M2 channel. This acidification leads to fusion of the endosome with the cytoplasm and uncoating of the virus with release of the RNA into the cytoplasm. Once in the cytoplasm, the RNA molecules translocate to the cell nucleus leading to production of new viral proteins and RNA. Viral proteins are then packaged and bud from the cell. This process is mediated by neuraminidase with resulting release of the virion into circulation [5].
Influenza has tropism for the columnar epithelial cells of the upper respiratory tract [4]. Viral replication occurs within 4–6 h of infection, incubation is 18–72 h followed by symptoms consisting of the typical fever, malaise, cough, pharyngitis and myalgias. Viral shedding has been estimated to occur for 2–5 days following onset of symptoms, though more severe infections may increase this time period [6].
The immune response to flu is both humoral and cell mediated. Development of antibodies to hemagglutinin protects from infection and is the mechanism of protection for all flu vaccines. In the case of infection, antibodies develop to both the M2 channel and neuraminidase. This prevents virus budding from infected cells. Viral protein is presented by infected cells on MHC class 1 molecules and this leads to targeting by Cd8+ cytotoxic T-cells with eventual lysis of the infected cell and clearance of viremia [7].
Differences in hemagglutinin and neuraminidase confer the familiar numbers seen in flu strains such as “H1N1” or “H3N2”. Minor variation in one of these two antigens leads to seasonal flu changes “drift”; whereas major variation “shift” is responsible for pandemic influenza strains [4]. Reassortment is a major cause of antigenic shift. This occurs when different flu strains co-infect a host cell and “re-assort”, combining elements of different strains. This is thought to have occurred in the 2009 H1N1 “pandemic” influenza (H1N1pdm) which had elements of avian, human and swine influenza viruses [8].
In terms of epidemiology, Centers for Disease Control and Prevention (CDC) estimates vary on the mortality of seasonal influenza. In the US, annual estimates range from a few thousand to tens of thousands of deaths from influenza. (1) Pandemic influenzas can range from 1 to 4 million deaths globally. The highest mortality estimates are from the 1918 pandemic influenza at 50–100 million deaths globally—2–3% of the world population at the time. (2) Mortality disproportionately affects the elderly and those with underlying cardiac and pulmonary conditions. Differences in pre-existing immunity can shift this curve, as in the 2009 H1N1pdm where mortality rates were 8 and 12 times higher in children and adults <65 years old, respectively, compared to seasonal influenzas [9].
Influenza vaccination in the ESRD population
Typical influenza vaccines consist of 15 micrograms of inactivated injectable influenza protein—hemagglutinin. Current available vaccines are generally trivalent or quadrivalent—conferring protection against three to four potential seasonal strains of influenza. In addition, there is a “high-dose” trivalent vaccine available containing 60 µg of HA and an adjuvant vaccine. Both are approved for patients 65 and older. Live attenuated vaccine via intranasal spray (Flu-Mist) is no longer recommended due to poor response rates. (3) Most studies on vaccine efficacy consider a fourfold increase in hemagluttinin antibody response protective from infection. In the US, guidelines on vaccination administration are set by the Advisory Committee for Immunization Practices (ACIP) of the CDC. No specific recommendations are made in terms of which vaccine is preferential in ESRD patients, aside from noting that kidney disease patients are among the vulnerable patient populations that should be prioritized. Recommendations from the European Centre for Disease Prevention and Control are similar. Current vaccination rates in the dialysis population are about 70%, based on the 2013–2014 flu season and have improved markedly over the last 10 years [10].
Data on the immune response to vaccination in dialysis patients has been conflicting; however, the prevailing belief remains that dialysis patients have an impaired response. ESRD patients have a multitude of immune system defects that have been well described. Briefly, decreased monocyte/macrophage chemotaxis and phagocytosis, B-cell lymphopenia and depressed CD4+ and CD8+ T-cells have been described, among other changes [11,12,13]. Delayed/depressed antibody response and/or early waning of immunity occur in other vaccines such as hepatitis B. This has prompted antibody surveillance and booster protocols [14]. Early studies on influenza showed a promising response in ESRD patients. Jordan and colleagues showed similar rates of protective antibody generation in dialysis patients versus healthy controls in the early 1970s [15, 16]. Studies by Antonen and colleagues of inactivated trivalent vaccine linked a normal immune protection response in ESRD with calcitriol administration, a finding that has yet to be revisited [17, 18]. Overall; however, the balance of studies show a decreased response to influenza vaccines [19]. This has prompted some to advocate for the use of high-dose influenza vaccines in the ESRD population [20]. Unfortunately, neither high-dose influenza vaccine nor the currently available adjuvant vaccine, both approved for use in the elderly, has been tested in ESRD. A smaller study of a monovalent adjuvant vaccine for H1N1pdm influenza showed somewhat disappointing results with only 64% of HD patients seroconverting versus 94% in controls [21]. Therefore, the presumed benefit of high dose and adjuvant vaccines remains speculative.
The effect of vaccination on outcomes in the ESRD population remains unclear. Simply obtaining rates of influenza vaccination in dialysis units was historically difficult and relied on billing data, which may have led to under-reporting of vaccine recipients in large epidemiology studies. Also, the degree of vaccine match to a prevailing influenza strain significantly impacts the assessment of vaccine efficacy in any given year. Despite this, several studies have attempted to evaluate efficacy in ESRD patients. Gilbertson and colleagues used United Stated Renal Data System (USRDS) data to assess the effect of seasonal vaccination in dialysis patients in two flu seasons (1997–1998 and 1998–1999). They found vaccination was associated with lower mortality for both hemodialysis and peritoneal dialysis (PD) patients in both seasons [22]. A 2012 paper by Bond and colleagues reviewed combined data of three US ESRD networks including nearly 40,000 patients [23]. After excluding patients with less than 1 year on dialysis and those whose vaccination status was unknown, the relative risk of all-cause mortality was reduced ~30% in those receiving the flu vaccination and nearly 40% in those receiving both influenza and pneumococcal vaccines. This conclusion stands in contrast to another paper the same year by McGrath and colleagues using a different seasonal comparison methodology. McGrath’s analysis of a large dialysis cohort found minimal effect on all-cause mortality [24]. Specific to the PD population, Wang and colleagues evaluated the effect of seasonal vaccine in over 2000 incident PD patients versus an unvaccinated propensity matched cohort. The adjusted hazard ratio for overall mortality was 0.66 in the vaccine group [25]. Hospitalizations for cardiovascular disease, sepsis, ICU admission were all significantly lower in the vaccinated group. Data from the PEER Kidney Initiative, a research collaboration of the 13 largest US dialysis providers, has shown that hospitalizations for pneumonia and influenza have remained fairly stable, despite increases in vaccination rates over the last decade [26]. The largest systematic review of the effect of vaccination in ESRD found the body of literature to be of limited quality overall with most studies susceptible to confounding. Despite this, given the high mortality of ESRD patients as whole, the authors felt annual vaccination remained a reasonable policy [27]. This tepid endorsement of vaccination overall speaks to the need for larger studies of vaccine response and effectiveness in the ESRD population.
Clinical characteristics of influenza in the ESRD population
Despite the strong recommendations for vaccination in the ESRD population, little has been written about the clinical presentation of influenza in the dialysis population and how this may differ from the general population. The 2009 H1N1 pandemic flu provided an opportunity to describe the disease from the ESRD perspective and multiple case reports and series were published. The first ESRD case of H1N1pdm in the literature was reported from Manitoba, Canada [28]. There, a 32 year old male presented with shortness of breath, myalgias, malaise and productive cough. Importantly, the patient was afebrile. Despite 11 l of ultrafiltration and antibiotics, the patient remained hypoxic and polymerase chain reaction (PCR) testing demonstrated H1N1 virus. The patient remained afebrile throughout the course of admission and survived to discharge.
Fresenius medical care (FMC) provided the first clinical overview of a larger population of H1N1 pandemic influenza infected ESRD patients [29]. Pooling data from over 80 clinics in South America, Europe and Africa, FMC reported data on over 300 reported cases. Diagnosis was made by clinical characteristics (typical influenza-like illness), rapid flu testing, and rarely PCR. Most cases of influenza were in the younger 20–64 year old cohort. Fever, cough and myalgias were the most frequently cited symptoms. High rates of pneumonia were seen; 22.5% in these ESRD patients. Hospitalization rates were much higher in the diagnosed ESRD cohort—38% versus an estimated 6–7% in the general populations. Mortality was also much higher in the dialysis group at approximately 5 versus 0.4% in the general population.
In China, a smaller cohort of 15 patients was published by Li [30]. This patient group had the advantage of PCR diagnosis confirmation, increasing diagnostic confidence. Contrasting with the prior study, only one of the 15 patients presented with fever or a classic influenza-like illness. All patients experienced dyspnea and cough with high rates of bacterial nosocomial pneumonia following influenza infection. Six of the 15 patients required mechanical ventilation at one point. Length of stay was prolonged at an average of 14 days. All patients survived to discharge. Real time PCR performed throughout showed evidence of viral shedding for an average of 12 days; roughly double that described in the general population. How to reconcile the atypical pattern of the Chinese study with more typical influenza picture of the FMC cohort? The difference may be in the inclusion criteria—the FMC study used clinician description of influenza like illness with a high index of suspicion to diagnose many cases whereas the Chinese study used real time PCR. This may have left the FMC study susceptible to inclusion of febrile non H1N1 afflicted patients.
The question of susceptibility to influenza by modality also remains difficult to assess. In a 2011 paper, Cho et al. reported rates of H1N1 hospitalization in three hospitals in Korea during the 2009 pandemic. Rates of diagnosed influenza were more than four times lower in the PD population but the number of total patients infected was low [31]. Also, PD patients were younger with fewer co-morbidities. Despite controlling for differences in baseline characteristics, it is difficult to draw any firm conclusions about the course of the disease in PD versus HD.
Mortality of ESRD patients in the US due to influenza is difficult to assess as neither CMS nor CDC requires reporting of influenza deaths. Currently, CMS requires only vaccination rate reporting in ESRD units though the National Healthcare Safety Network (NHSN). The United States Renal Data System captures infections leading to hospitalization and mortality but breakouts for influenza alone are not available while data from the PEER initiative combines pneumonia and influenza diagnoses. Interestingly, data from the PEER Initiative has shown a seasonal pattern of admissions for influenza and pneumonia with associated peaks in cardiovascular-related admission such as myocardial infarction and heart failure [32]. This suggests a possible association of influenza and subsequent cardiac related hospitalization. Head to head comparison of infectious disease related mortality between ESRD patients and the general population was performed by a Japanese group for the 2008–2009 flu season. In that comparison, influenza mortality rates were three times higher in the ESRD patients than the general population [33]. Overall, infectious disease related mortality was seven times higher.
Treatment of influenza in dialysis patients
The Advisory Committee on Immunization Practices recommends treatment with antivirals for influenza infection in patients at high risk of complications—this includes patients with kidney disease/ESRD [34]. This recommendation holds for even those with mild infection that does not require hospitalization. Several antivirals are available for treatment of influenza. Currently, the most effective are the neuraminidase inhibitors. The amantadine class of antiviral has seen widespread resistance among currently circulating flu strains and are no longer recommended therapy. The neuraminidase inhibitors all work generally by blocking virion release from the host cell leading to eventual viremia clearance [5]. The main members of this class are oral oseltamivir (Tamiflu) and inhaled zanamivir (Relenza). In 2014, a new intravenous NA inhibitor was FDA approved, peramivir (Rapivab), though the drug was used on an emergency use authorization during the height of the 2009 pandemic influenza period [35]. Only oseltamivir and peramivir are approved NA inhibitors for use in dialysis patients [34].
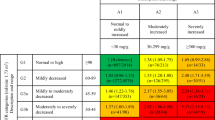
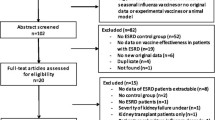
Dosing recommendations generally describe treatment dosing as well as chemoprophylaxis. Data in ESRD is limited, and there are differences between modalities; please see Table 1. Oseltamivir is rapidly converted to oseltamivir carboxylate, the active metabolite. It is 3% protein bound with a volume of distribution of 23 l. Dosing mostly relies on a 2006 study of chemoprophylaxis in hemodialysis and peritoneal dialysis patients [36]. In that study, hemodialysis patients received a 30 mg dose of oseltamivir 1 h following their dialysis session for a period of 6 weeks. Peak plasma concentrations reached protective levels from a chemoprophylaxis standpoint and also were considered high enough for treatment. In that same study, patients on continuous ambulatory peritoneal dialysis (CAPD) were also evaluated. Plasma protective levels were obtained with a single weekly dose of 30 mg. Continuous cycler-assisted PD (CCPD) patients were compared to CAPD patients in a small 2014 study [37]. CCPD patients were found to clear the drug roughly twice as fast and a single dose of 75 mg was recommended by the authors.
Dosing for continuous renal therapies remains uncertain and trials are few with small participants. A 2012 study of osteltamivir on continuous veno-venous hemodialysis used dosing of 150 mg twice daily for 5 days—a higher dose often recommended in critically ill patients. In that study, there was wide variation in peak plasma concentrations—up to 14-fold difference between patients and overall concentrations much higher than in those with normal renal function [38]. The same dose was used in a 2008 case series of patients with seasonal influenza, critical illness and on high dose (45 ml/kg/h) continuous veno-venous hemofiltration. The number of patients was only three, but again, peak concentrations of oseltamivir carboxylate varied five to sixfold between the patients and were considerably higher than expected in patients with normal renal function [39]. Lastly, another small case series of three patients reported pharmacokinetics on continuous veno-venous hemodiafiltration (CVVHDF) and extracorporeal membrane oxygenation (ECMO) with variable dosing schemes. Results were similar—much higher concentrations even on CVVHDF and the authors concluded dose reduction should be used [40].
Peramivir is an intravenous formulation that is typically administered as a one time 600 mg infusion administered over 15–30 min. Dosing recommendations provided by the manufacturer provide adjustments by creatinine clearance only. There are no specific recommendations for dialysis patients aside from a single dose administered “after dialysis” at a dose “reduced for Creatinine Clearance” [41]. In some publications, the FDA recommended a single 100 mg dose after hemodialysis on day 1, then additional 100 mg doses 2 h after subsequent hemodialysis sessions, though that is not found on the manufacturers prescribing information [42]. Data on PD patients is not available. Dosing information on continuous therapies is limited with a single case report for a patient on slow low efficiency dialysis (SLED) and four other patients on CVVHDF, CVVHD and CVVHF [35, 43,44,45]. The authors of the SLED paper suggested dosing at the standard single 600 mg infusion citing a clearance of >60 ml/min of drug while on SLED [35]. Another case report detailed a 29 year old on CVVHD receiving 600 mg IV with followup daily doses of 480 mg IV during the 2009 pandemic season. The authors used maintenance dosing after the initial bolus due to fears of high clearance as protein binding is low at <30%. In the three other patients, standard dosing of 600 mg IV once was used. All found the dose effective at achieving target peak plasma concentrations, but effect on clinical outcomes was unclear. In all cases, the drug was used under an emergency authorization.
Special considerations: unit chemoprophylaxis
Free standing dialysis units provide several elements needed for pathogen transmission—a vulnerable population with multiple chronic health conditions in close proximity for an extended period of time. The Infectious Disease Society of America (IDSA) has provided recommendations regarding use of chemoprophylaxis in health care settings such as skilled nursing facilities [46]. There are no specific guidelines for dialysis units; however, the CDC and IDSA suggest chemoprophylaxis in institutions where two or more individuals are diagnosed within 72 h, at least one with confirmed influenza. Chemoprophylaxis dosing should be given for a minimum of 2 weeks and through 1 week after the last confirmed case. All patients, including those vaccinated, should receive chemoprophylaxis.
In one of the authors’ affiliated academic units, a case cluster of H1N1pdm influenza occurred in the 2013–2014 season resulting in three ICU admissions and several hospital visits within 4–5 days. PCR testing of all symptomatic patients in the unit, even those with mild cough or cold, was instituted and yielded a 26% rate of influenza infection, despite a 96% vaccination rate. Chemoprophylaxis was instituted based on the above guidelines with standard 30 mg post dialysis dosing until 1 week after the final confirmed cases. Thus, we strongly recommend dialysis units develop influenza action plans that emphasize vaccination first but also address the procedures for an outbreak in the unit.
References
Thompson MG et al (2010) Estimates of deaths associated with seasonal influenza—United States 1976–2007. MMWR 59:1057–1062
World Health Organization (2009) Pandemic influenza preparedness and response: a WHO guidance document. WHO, Geneva
Prevention and Control of Seasonal Influenza with Vaccines (2016) Recommendations of the advisory committee on immunization practices—United States, 2016–2017 influenza season. MMWR 65:1–52
Treanor J (2015) In: Bennett JE (ed) Influenza principles and practice of infectious diseases, 8th edn. Elsevier, Philadelphia
De Clerq E (2007) Avian influenza A (H5N1) infection: targets and strategies for chemotherapeutic intervention. Trends Pharm Sci 28(6):280–285
Cohen YZ, Dolin R (2015) Influenza. In: Kasper D et al (eds) Harrison’s principles of internal medicine, 19th Edn. McGraw-Hill Education, USA
Subbarao K, Joseph T (2007) Scientific barriers to developing vaccines against avian influneza viruses. Nat Rev Immunol 7:267–278
York I, Donis RO (2012) The 2009 pandemic influenza virus: where did it come from, where is it now, and where is it going? CRRN Top Mirc Immun 370:241–257
Shrestha S et al (2011) Estimating the burden of 2009 pandemic influneza A (H1N1) in the United States (April 2009–April 2010). Clin Infect Dis 52(Supplement):S75–S82
United States Renal Data System (2016) 2016 USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda
Betjes MG (2013) Immune cell dysfunction and inflammation in end-stage renal disease. Nat Rev Nephrol 9:255–265
Eleftheriadis T et al (2007) Disturbances in acquired immunity in hemodialysis patients. Semin Dial 20:440–451
Hauser AB et al (2007) Characteristics and causes of immune dysfunction related to uremia and dialysis. Perit Dial Int 28(Supplement 3):S183–S187
Soni R, Horowitz B, Unruh M (2013) Immunization in end-stage renal disease: opportunity to improved outcomes. Semin Dial 26:416–426
Jordan MC et al (1973) Immunogenicity of inactivated influenza virus vaccine in chronic renal failure. Ann Intern Med 79:790–794
Ortbals DW (1978) Influenza immunization in patients with chronic renal disease. JAMA 239:2562–2565
Antonen JA et al (2000) Adequate seroresponse to influenza vaccination in dialysis patients. Nephron 86:56–61
Antonen JA et al (2003) Influenza vaccination of dialysis patients: cross-reactivity of induced haemagglutination-inhibiting antibodies to H3N2 subtype antigenic variants is comparable with the response of naturally infected young healthy adults. Nephrol Dial Transplant 18:777–781
Dinits-Pensy M et al (2005) The use of vaccines in adult patients with renal disease. AJKD 46:997–1011
Peer Kidney Care Initiative. Peer Report: Dialysis Care and Outcomes in the United States, 2016. http://www.peerkidney.org/wp-content/uploads/2016/11/Chapter-2-Hospitalizations.pdf. Accessed 9 Feb 2017
Labriola L et al (2011) Immunocgenicity of an adjuvanted 2009 pandemic influenza A (H1N1) vaccine in heamodialysed patients. NDT 26:1424–1428
Gilbertson DT et al (2003) Influenza vaccine delivery and effectiveness in end-stage renal disease. Kidney Int 63:738–743
Bond TC, Spaulding AC, Krisher J, McClellan W (2012) Mortality of dialysis patients according to influenza and pneumococcal vaccination status. Am J Kidney Dis 60:959–965
McGrath LJ et al (2012) Influenza vaccine effectiveness in patients on hemodialysis: an analysis of a natural experiment. Arch Intern Med 172:548–554
Wang I et al (2016) Seasonal influenza vaccination is associated with reduced morbidity and mortality in peritoneal dialysis patients. NDT 31:269–274
Wetmore JB, PEER Kidney Care Initiative Investigators (2016) Trends in infection in dialysis patients. AJKD 67:A13
Remschmidt C, Wichmann O, Harder T (2014) Influenza vaccination in patients with end-stage renal disease: systematic review and assessment of quality of evidence related to vaccine efficacy, effectiveness, and safety. BMC Med 12:1–14
Wiebe C et al (2009) Atypical clinical presentation of H1N1 influenza in a dialysis patient. Lancet 374:1300
Marcelli D, Marelli C, Richards N (2009) Influenza A(H1N1)v pandemic in the dialysis population: first wave results from an international survey. Nephrol Dial Transplant 24:3566–3572
Li H, Wang SX (2010) Clinical features of 2009 pandemic influenza A (H1N1) virus infection in chronic hemodialysis patients. Blood Purif 30:172–177
Cho JH et al (2011) Impact of dialysis modality on the incidence of 2009 pandemic H1N1 influenza in end-stage renal disease patients. Perit Dial Int 31:347–350
Peer Kidney Care Initiative (2015) Seasonality of hospitalization for pneumonia, influenza, and dialysis access infection. AJKD 65:A67
Wakasugi M (2012) High mortality rate of infectious diseases in dialysis patients: a comparison with the general population in Japan. Ther Apher Dial 16:226–231
ACIP (2011) Antiviral agents for the treatment and chemoprophylaxis of influenza. MMWR 60(1):1–24
Thomas B, Hollister AS, Muczynski KA (2010) Peramivir clearance in continuous renal replacement therapy. Hemodial Int 14:339–340
Robson R et al (2006) The pharmacokinetics and tolerability of oseltamivir suspension in patients on haemodialysis and continuous ambulatory peritoneal dialysis. Nephol Dial Transplant 21:2556–2562
Patel K et al (2014) Pharmacokinetics and safety of oseltamivir in patients with end-stage renal disease treated with automated peritoneal dialysis. Br J Clin Pharmacol 79:624–635
Eyler RF, Heung M, Pleva M (2012) Pharmacokinetics of oseltamivir and oseltamivir carboxylate in critically ill patients receiving continuous venovenous hemodialysis and/or extracorporeal membrane oxygenation. Pharmacotherapy 32:1061–1069
Taylor WR, Thinh BN, Anh GT (2008) Oseltamivir is adequately absorbed following nasogastric administration to adult patients with severe H5N1 influenza. PLoS One 3:e3410
Flannery AH, Thomson B ML (2014) Oseltamivir dosing in critically Ill patients with severe influenza. Ann Pharamcotherapy 48:1011–1018
Rapivab Highlights of Prescribing Information. Rapivab.com. http://labeling.cslbehring.com/PI/US/Rapivab/EN/Rapivab-Prescribing-Information.pdf. Accessed 9 Feb 2017
Questions and Answers for Health Care Providers: Renal Dosing and Administration Recommendations for Peramivir IV. FDA.gov. http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM190601.pdf. Accessed 9 Feb 2017
Bazan JA et al (2010) Peramivir pharmacokinetics in two critically ill adult patients with 2009 H1N1 influenza A concurrently receiving continuous renal replacement therapy. Pharmacotherapy 10:1016–1020
Bentley ML et al (2014) Peramivir pharmacokinetics in a patient receiving continuous veno-venous hemodiafiltration during the 2009 H1N1 influenza A pandemic. Int J Clin Pharmacol Ther 52:1105–1111
Scheetz MH et al (2011) Pharmacokinetic assessment of peramivir in a hospitalized adult undergoing continuous venovenous hemofiltration. Ann Pharmacother 45(12):E64
Harper SA et al (2008) Seasonal influenza in adults and children—diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the infectious disease society of America. Clin Infect Dis 48:1003–1032
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Human and animal rights
The articles does not contain any studies with any human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Bowman, B.T., Rosner, M.H. Influenza and the patient with end-stage renal disease. J Nephrol 31, 225–230 (2018). https://doi.org/10.1007/s40620-017-0407-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-017-0407-9