Abstract
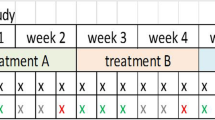
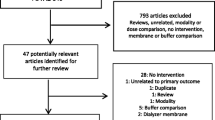
Dialysate cooling, either individualized based upon patient body temperature, or to a standardized temperature below 37 °C, has been proposed to minimize hemodynamic insults and improve outcomes among hemodialysis patients. However, low dialysate temperatures (35–35.5 °C) are associated with patient discomfort, and individualized dialysate cooling is difficult to operationalize. Here, we tested whether a standardized dialysate temperature of 36 °C (dT36) was associated with improved clinical outcomes compared to the default temperature of 37 °C (dT37). Because patients with known hemodynamic instability may be selectively prescribed dT36, we minimized selection bias by considering only incident adult in-center hemodialysis patients who, between Jan 2011 and Dec 2013 received their first-ever hemodialysis treatment at a large dialysis organization. Exposure status was based on the treatment order for this first-ever treatment. 313 dT36 patients were identified and propensity-score matched (1:5) to 1565 dT37 controls. Death, hospitalization, and missed hemodialysis treatments were considered from the date of first-ever hemodialysis treatment until the earliest of death, loss to follow-up, crossover (month in which prescribed dialysate temperature was consistent with patient’s exposure group for <80% of treatments), or study end (June 2015). During follow-up, rates of death, hospitalization and missed hemodialysis treatments did not differ between the two groups. This study therefor showed no benefit of dT36 vs. dT37 with respect to these clinical outcomes. Our results do not favor conversion to a default dialysate temperature of 36 °C. Individualized dialysate cooling may provide a more reliable approach to achieve the hemodynamic benefits associated with reduced dialysate temperature.

Similar content being viewed by others
References
US Renal Data System (2015) USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD
McIntyre CW (2010) Recurrent circulatory stress: the dark side of dialysis. Semin Dial 23(5):449–451
Maggiore Q, Pizzarelli F, Zoccali C, Sisca S, Nicolo F, Parlongo S (1981) Effect of extracorporeal blood cooling on dialytic arterial hypotension. Proc Eur Dial Transplant Assoc 18:597–602
Mustafa RA, Bdair F, Akl EA, Garg AX, Thiessen-Philbrook H, Salameh H, Kisra S, Nesrallah G, Al-Jaishi A, Patel P et al (2016) Effect of lowering the dialysate temperature in chronic hemodialysis: a systematic review and meta-analysis. Clin J Am Soc Nephrol 11(3):442–457
Eldehni MT, Odudu A, McIntyre CW (2015) Randomized clinical trial of dialysate cooling and effects on brain white matter. J Am Soc Nephrol 26(4):957–965
Odudu A, Eldehni MT, McCann GP, McIntyre CW (2015) Randomized controlled trial of individualized dialysate cooling for cardiac protection in hemodialysis patients. Clin J Am Soc Nephrol 10(8):1408–1417
Odudu A, Eldehni MT, Fakis A, McIntyre CW (2012) Rationale and design of a multi-centre randomised controlled trial of individualised cooled dialysate to prevent left ventricular systolic dysfunction in haemodialysis patients. BMC Nephrol 13:45
Brunelli SM, Sibbel S, Do TP, Cooper K, Bradbury BD (2015) Facility dialysate calcium practices and clinical outcomes among patients receiving hemodialysis: a retrospective observational study. Am J Kidney Dis 66(4):655–665
Selby NM, McIntyre CW (2006) A systematic review of the clinical effects of reducing dialysate fluid temperature. Nephrol Dial Transplant 21(7):1883–1898
Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM (2015) Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol 26(3):724–734
Fine A, Penner B (1996) The protective effect of cool dialysate is dependent on patients’ predialysis temperature. Am J Kidney Dis 28(2):262–265
Pizzarelli F (2007) From cold dialysis to isothermic dialysis: a twenty-five year voyage. Nephrol Dial Transplant 22(4):1007–1012
Usvyat LA, Raimann JG, Carter M, van der Sande FM, Kooman JP, Kotanko P, Levin NW (2012) Relation between trends in body temperature and outcome in incident hemodialysis patients. Nephrol Dial Transplant 27(8):3255–3263
Kuipers J, Oosterhuis JK, Krijnen WP, Dasselaar JJ, Gaillard CA, Westerhuis R, Franssen CF (2016) Prevalence of intradialytic hypotension, clinical symptoms and nursing interventions: a three-months, prospective study of 3818 haemodialysis sessions. BMC Nephrol 17(1):21
Stefansson BV, Brunelli SM, Cabrera C, Rosenbaum D, Anum E, Ramakrishnan K, Jensen DE, Stalhammar NO (2014) Intradialytic hypotension and risk of cardiovascular disease. Clin J Am Soc Nephrol 9(12):2124–2132
McIntyre CW, Harrison LE, Eldehni MT, Jefferies HJ, Szeto CC, John SG, Sigrist MK, Burton JO, Hothi D, Korsheed S et al (2011) Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol 6(1):133–141
Kooman J, Basci A, Pizzarelli F, Canaud B, Haage P, Fouque D, Konner K, Martin-Malo A, Pedrini L, Tattersall J et al (2007) EBPG guideline on haemodynamic instability. Nephrol Dial Transplant 22(Suppl 2):ii22–i44
Usvyat LA, Kotanko P, van der Sande FM, Kooman JP, Carter M, Leunissen KM, Levin NW (2012) Circadian variations in body temperature during dialysis. Nephrol Dial Transplant 27(3):1139–1144
Acknowledgements
The authors wish to acknowledge all members of the Healthcare Analytics and Insights team for their assistance and helpful discussions. This study was funded by DaVita Inc. Data from this study was presented in abstract and poster form at ASN Kidney Week 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by DaVita, Inc. KSG, DEC, and SMB are employees thereof. DaVita, Inc had no role in study design; collection, analysis, and interpretation of data; nor writing the report. DaVita, Inc was involved in the decision to submit the report for publication and was provided a draft of the manuscript for review prior to submission. None of the authors have any financial disclosures. SMB’s spouse is an employee of AstraZeneca.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gray, K.S., Cohen, D.E. & Brunelli, S.M. Dialysate temperature of 36 °C: association with clinical outcomes. J Nephrol 31, 129–136 (2018). https://doi.org/10.1007/s40620-016-0369-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-016-0369-3