Abstract
Purpose
Information on the general health of transgender and gender diverse (TGD) individuals continues to be lacking. To bridge this gap, the National Institute of Health in Italy together with the National Office against Racial Discriminations, clinical centres, and TGD organizations carried out a cross-sectional study to define the sociodemographic profile, health-related behaviours, and experiences of healthcare access in Italian TGD adult population.
Methods
A national survey was conducted by Computer-Assisted Web Interviewing (CAWI) technique. Collected data were compared within the TGD subgroups and between TGD people and the Italian general population (IGP).
Results
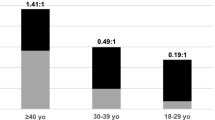
TGD respondents were 959: 65% assigned female at birth (AFAB) and 35% assigned male at birth (AMAB). 91.8% and 8.2% were binary and non-binary TGD respondents, respectively. More than 20% of the TGD population reported to be unemployed with the highest rate detectable in AMAB and non-binary people. Cigarette smoking and binge drinking were higher in the TGD population compared with IGP (p < 0.05), affecting TGD subgroups differently. A significant lower percentage of AFAB TGD people reported having had screening for cervical and breast cancer in comparison with AFAB IGP (p < 0.0001, in both cases). Over 40% was the percentage of AFAB and non-binary TGD people accessing healthcare who felt discriminated against because of their gender identity.
Conclusions
Our results are a first step towards a better understanding of the health needs of TGD people in Italy in order to plan the best policy choices for a more inclusive public health.
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this publication article and its supplementary information file.
Abbreviations
- AFAB:
-
Assigned female at birth
- AMAB:
-
Assigned male at birth
- Cis:
-
Confidence intervals
- GPs:
-
General practitioners
- IGP:
-
Italian general population
- ISS:
-
Istituto superiore di sanità-National institute of health in Italy
- ISTAT:
-
Istituto nazionale di statistica-National institute of statistics
- NB:
-
Non-binary
- PASSI:
-
Progressi delle aziende sanitarie per la salute in Italia-Italian Behavioural risk factor surveillance system
- POR:
-
Prevalence odds ratio
- TGD:
-
Transgender and gender diverse
- UNAR:
-
Ufficio nazionale antidiscriminazioni razziali-National office against racial discriminations
References
Coleman E, Radix AE, Bouman WP et al (2022) Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgend Health 23(Suppl 1):S1–S259. https://doi.org/10.1080/26895269.2022.2100644
Zhang Q, Goodman M, Adams N et al (2020) Epidemiological considerations in transgender health: a systematic review with focus on higher quality data. Int J Transgend Health 21(2):125–137. https://doi.org/10.1080/26895269.2020.1753136
Fisher A, Marconi M, Castellini G et al (2024) Estimate and needs of the transgender adult population in Italy: the spot study. J Endocrinol Invest. https://doi.org/10.1007/s40618-023-02251-9
Wiepjes CM, Nota NM, de Blok CJM et al (2018) The amsterdam cohort of gender dysphoria study (1972–2015): trends in prevalence, treatment, and regrets. J Sex Med 15(4):582–590. https://doi.org/10.1016/j.jsxm.2018.01.016
Leinung MC, Joseph J (2020) Changing demographics in transgender individuals seeking hormonal therapy: are trans women more common than trans men? Transgend Health 5(4):241–245. https://doi.org/10.1089/trgh.2019.0070
Reisner SL, Poteat T, Keatley J et al (2016) Global health burden and needs of transgender populations: a review. Lancet 388(10042):412–436. https://doi.org/10.1016/S0140-6736(16)00684-X
Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, Wylie K (2016) Transgender people: health at the margins of society. Lancet 388(10042):390–400. https://doi.org/10.1016/S0140-6736(16)00683-8
EU Agency for Fundamental Rights (2020) A long way to go for LGBTI equality: technical report. Luxembourg. https://fra.europa.eu/sites/default/files/fra_uploads/fra-2020-lgbti-equality-technical-report_en.pdf. Accessed 7 Dec 2022
Reisner SL, Deutsch MB, Bhasin S et al (2016) Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes 23(2):198–207. https://doi.org/10.1097/MED.0000000000000229
ISTAT, Istituto Nazionale di Statistica (2017) Forme, livelli e dinamiche dell’urbanizzazione in Italia. https://www.istat.it/it/files/2017/05/Urbanizzazione.pdf. Accessed 7 Dec 2022
National health service: essential levels of assistance. Preventive healthcare measures. https://www.salute.gov.it/portale/lea/dettaglioContenutiLea.jsp?lingua=english&id=5442&area=Lea&menu=prevLea. Accessed 7 Dec 2022
Distante V, Ciatto S, Frigerio A et al (2007) Recommendations of a national Italian consensus conference on the opportunity of extending screening service by mammography to 40–49 and 70–74 years of age women. Epidemiol Prev 31(1):15–22
ISTAT, Istituto Nazionale di Statistica. Resident population on 1st January 2021. https://esploradati.istat.it/databrowser/#/it/dw/categories/IT1,POP,1.0/POP_POPULATION/DCIS_POPRES1/IT1,22_289_DF_DCIS_POPRES1_1,1.0. Accessed 7 Dec 2022
Fisher AD, Bandini E, Casale H et al (2013) Sociodemographic and clinical features of gender identity disorder: an Italian multicentric evaluation. J Sex Med 10(2):408–419. https://doi.org/10.1111/j.1743-6109.2012.03006.x
Baldissera S, Ferrante G, Quarchioni E et al (2014) Field substitution of nonresponders can maintain sample size and structure without altering survey estimates-the experience of the Italian behavioral risk factors surveillance system (PASSI). Ann Epidemiol 24(4):241–245. https://doi.org/10.1016/j.annepidem.2013.12.003
Baldissera S, Campostrini S, Binkin N et al (2011) Features and initial assessment of the Italian behavioral risk factor surveillance system (PASSI), 2007–2008. Prev Chronic Dis 8(1):A24
Romani A, Mazzoli F, Ristori J et al (2021) Psychological wellbeing and perceived social acceptance in gender diverse individuals. J Sex Med 18(11):1933–1944. https://doi.org/10.1016/j.jsxm.2021.08.012
Leppel K (2021) Transgender men and women in 2015: employed, unemployed, or not in the labor force. J Homosex 68(2):203–229. https://doi.org/10.1080/00918369.2019.1648081
Aparicio-García ME, Díaz-Ramiro EM, Rubio-Valdehita S, López-Núñez MI, García-Nieto I (2018) Health and well-being of cisgender transgender and non-binary young people. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph15102133
Azagba S, Latham K, Shan L (2019) Cigarette, smokeless tobacco, and alcohol use among transgender adults in the United States. Int J Drug Policy 73:163–169. https://doi.org/10.1016/j.drugpo.2019.07.024
Buchting FO, Emory KT, Scout KY, Fagan P, Vera LE, Emery S (2017) Transgender use of cigarettes, cigars, and E-cigarettes in a national study. Am J Prev Med 53(1):e1–e7. https://doi.org/10.1016/j.amepre.2016.11.022
Tamí-Maury I, Sharma A, Chen M, Blalock J, Ortiz J, Weaver L, Shete S (2020) Comparing smoking behavior between female-to-male and male-to-female transgender adults. Tob Prev Cessat. https://doi.org/10.18332/tpc/114513
Hughto JMW, Quinn EK, Dunbar MS, Rose AJ, Shireman TI, Jasuja GK (2021) Prevalence and co-occurrence of alcohol, nicotine, and other substance use disorder diagnoses among US transgender and cisgender adults. JAMA Netw Open 4(2):e2036512. https://doi.org/10.1001/jamanetworkopen.2020.36512
Kittaneh AA, Patel S, Sidhu NK, Lechner WV, Kenne DR (2021) Tobacco use status as a function of transgender identity: the mediating role of psychological distress. Tob Use Insights 14:1179173X211004267. https://doi.org/10.1177/1179173X211004267
Downing JM, Przedworski JM (2018) Health of transgender adults in the U.S., 2014–2016. Am J Prev Med 55(3):336–344. https://doi.org/10.1016/j.amepre.2018.04.045
Sawyer AN, Bono RS, Kaplan B, Breland AB (2022) Nicotine/tobacco use disparities among transgender and gender diverse adults: findings from wave 4 PATH data. Drug Alcohol Depend 232:109268. https://doi.org/10.1016/j.drugalcdep.2022.109268
Mahalik JR, Burns SM, Syzdek M (2007) Masculinity and perceived normative health behaviors as predictors of men’s health behaviors. Soc Sci Med 64(11):2201–2209. https://doi.org/10.1016/j.socscimed.2007.02.035
Wheldon CW, Watson RJ, Fish JN, Gamarel K (2019) Cigarette smoking among youth at the intersection of sexual orientation and gender identity. LGBT Health 6(5):235–241. https://doi.org/10.1089/lgbt.2019.0005
Coulter RW, Blosnich JR, Bukowski LA, Herrick AL, Siconolfi DE, Stall RD (2015) Differences in alcohol use and alcohol-related problems between transgender- and nontransgender-identified young adults. Drug Alcohol Depend 154:251–259. https://doi.org/10.1016/j.drugalcdep.2015.07.006
Day JK, Fish JN, Perez-Brumer A, Hatzenbuehler ML, Russell ST (2017) Transgender youth substance use disparities: results from a population-based sample. J Adolesc Health 61(6):729–735. https://doi.org/10.1016/j.jadohealth.2017.06.024
Reisner SL, Greytak EA, Parsons JT, Ybarra ML (2015) Gender minority social stress in adolescence: disparities in adolescent bullying and substance use by gender identity. J Sex Res 52(3):243–256. https://doi.org/10.1080/00224499.2014.886321
Gamarel KE, Mereish EH, Manning D, Iwamoto M, Operario D, Nemoto T (2016) Minority stress, smoking patterns, and cessation attempts: findings from a community-sample of transgender women in the san francisco bay area. Nicotine Tob Res 18(3):306–313. https://doi.org/10.1093/ntr/ntv066
Shires DA, Jaffee KD (2016) Structural discrimination is associated with smoking status among a national sample of transgender individuals. Nicotine Tob Res 18(6):1502–1508. https://doi.org/10.1093/ntr/ntv221
Hatzenbuehler ML, Phelan JC, Link BG (2013) Stigma as a fundamental cause of population health inequalities. Am J Public Health 103(5):813–821. https://doi.org/10.2105/AJPH.2012.301069
de Blok CJM, Dreijerink KMA, den Heijer M (2019) Cancer risk in transgender people. Endocrinol Metab Clin North Am 48(2):441–452. https://doi.org/10.1016/j.ecl.2019.02.005
Braun H, Nash R, Tangpricha V, Brockman J, Ward K, Goodman M (2017) Cancer in transgender people: evidence and methodological considerations. Epidemiol Rev 39(1):93–107. https://doi.org/10.1093/epirev/mxw003
Leone AG, Casolino R, Trapani D et al (2023) Position paper of the Italian association of medical oncology on health disparities among transgender and gender-diverse people: the assisi recommendations. EClinicalMedicine 65:102277. https://doi.org/10.1016/j.eclinm.2023.102277
Bazzi AR, Whorms DS, King DS, Potter J (2015) Adherence to mammography screening guidelines among transgender persons and sexual minority women. Am J Public Health 105(11):2356–2358. https://doi.org/10.2105/AJPH.2015.302851
Luehmann N, Ascha M, Chwa E et al (2022) A single-center study of adherence to breast cancer screening mammography guidelines by transgender and non-binary patients. Ann Surg Oncol 29(3):1707–1717. https://doi.org/10.1245/s10434-021-10932-z
Tabaac AR, Sutter ME, Wall CSJ, Baker KE (2018) Gender identity disparities in cancer screening behaviors. Am J Prev Med 54(3):385–393. https://doi.org/10.1016/j.amepre.2017.11.009
Kiran T, Davie S, Singh D, Hranilovic S, Pinto AD, Abramovich A, Lofters A (2019) Cancer screening rates among transgender adults: Cross-sectional analysis of primary care data. Can Fam Physician 65(1):e30–e37
Scheim A, Bauer G (2013) Breast and cervical cancer screening among trans Ontarians: a report prepared for the Screening Saves Lives Program of the Canadian Cancer Society. Trans PULSE Project. https://www.transpulseproject.ca. Accessed 7 Dec 2022
Heer E, Peters C, Knight R, Yang L, Heitman SJ (2023) Participation, barriers, and facilitators of cancer screening among LGBTQ+ populations: a review of the literature. Prev Med 170:107478. https://doi.org/10.1016/j.ypmed.2023.107478
Peitzmeier SM, Agénor M, Bernstein IM et al (2017) “It can promote an existential crisis”: Factors influencing pap test acceptability and utilization among transmasculine individuals. Qual Health Res 27(14):2138–2149. https://doi.org/10.1177/1049732317725513
Peitzmeier SM, Khullar K, Reisner SL, Potter J (2014) Pap test use is lower among female-to-male patients than non-transgender women. Am J Prev Med 47(6):808–812. https://doi.org/10.1016/j.amepre.2014.07.031
James SEHJ, Rankin S, Keisling M, Mottet LAA (2016) The report of the 2015 US Transgender Survey. https://www.ustranssurvey.org/reports. Accessed 7 Dec 2022
Agénor M, White Hughto JM, Peitzmeier SM, Potter J, Deutsch MB, Pardee DJ, Reisner SL (2018) Gender identity disparities in Pap test use in a sample of binary and non-binary transmasculine adults. J Gen Intern Med 33(7):1015–1017. https://doi.org/10.1007/s11606-018-4400-3
Carroll R, Tan KKH, Ker A, Byrne JL, Veale JF (2023) Uptake, experiences and barriers to cervical screening for trans and non-binary people in Aotearoa New Zealand. Aust N Z J Obstet Gynaecol 63(3):448–453. https://doi.org/10.1111/ajo.13674
Agénor M, Peitzmeier SM, Bernstein IM et al (2016) Perceptions of cervical cancer risk and screening among transmasculine individuals: patient and provider perspectives. Cult Health Sex 18(10):1192–1206. https://doi.org/10.1080/13691058.2016.1177203
Nicholls EJ, McGowan CR, Miles S et al (2023) Provision of cervical screening for transmasculine patients: a review of clinical and programmatic guidelines. BMJ Sex Reprod Health 49(2):118–128. https://doi.org/10.1136/bmjsrh-2022-201526
Roznovjak D, Petroll AE, Lakatos AEB, Narayan R, Cortina CS (2023) Perceptions of transgender and nonbinary persons toward breast and cervical cancer development, screening, and potential impact on gender-affirming hormone therapy. JCO Oncol Pract OP2200681. https://doi.org/10.1200/OP.22.00681
Scheim AI, Perez-Brumer AG, Bauer GR (2020) Gender-concordant identity documents and mental health among transgender adults in the USA: a cross-sectional study. Lancet Public Health 5(4):e196–e203. https://doi.org/10.1016/S2468-2667(20)30032-3
Kattari SK, Call J, Holloway BT, Kattari L, Seelman KL (2021) Exploring the experiences of transgender and gender diverse adults in accessing a trans knowledgeable primary care physician. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph182413057
Drabish K, Theeke LA (2022) Health impact of stigma, discrimination, prejudice, and bias experienced by transgender people: a systematic review of quantitative studies. Issues Ment Health Nurs 43(2):111–118. https://doi.org/10.1080/01612840.2021.1961330
Jaffee KD, Shires DA, Stroumsa D (2016) Discrimination and delayed health care among transgender women and men: implications for improving medical education and health care delivery. Med Care 54(11):1010–1016. https://doi.org/10.1097/MLR.0000000000000583
de Vries E, Kathard H, Müller A (2020) Debate: Why should gender-affirming health care be included in health science curricula? BMC Med Educ 20(1):51. https://doi.org/10.1186/s12909-020-1963-6
Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, Sevelius J (2016) Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes 23(2):168–171. https://doi.org/10.1097/MED.0000000000000227
Feldman JL, Luhur WE, Herman JL, Poteat T, Meyer IH (2021) Health and health care access in the US transgender population health (TransPop) survey. Andrology 9(6):1707–1718. https://doi.org/10.1111/andr.13052
National Academies of Sciences, Engineering, and Medicine (2020) Understanding the Well-Being of LGBTQI+ Populations. The National Academies Press, Washington, DC. https://doi.org/10.17226/25877
Acknowledgements
The project was established with the co-funding of the European Union, National Operational Programme for social inclusion—European Social Fund 2014–2020. We are deeply grateful to all those who played a role in the success of this project. We wish to thank our study participants for sharing their voices and experiences. We also thank TGD organizations (ALA Milano; Associazione Consultorio Transgenere, Associazione Libellula Italia APS; Associazione Maurice GLBT, Spo.T Sportello Trans; Associazione Transessuale Napoli, ATN; Azione Trans; Boramosa, Centro Salute Trans e Gender Variant, CEST; Gruppo Ascolto Giovani Arcobaleno, G.A.G.A; Gay Center; Gender X; Gruppo Trans APS; I Ken; Intersexioni; Movimento Identità Trans, MIT; Sat Pink APS; Sunderam; T Genus: Magna Grecia) for their active contribution in planning the study and disseminating the questionnaire. We would like to thank the Osservatorio Nazionale sull'Identità di Genere (ONIG)—National Observatory on Gender Identity and “The Bridge” Foundation for their precious support, Anna Ferrigno for her technical management, Monica Brocco, and Isabel Torres-Carrilho for their linguistic revision of the text.
Author information
Authors and Affiliations
Contributions
M.M. and M.T.P made substantial contributions to the conception of the work, interpreted the results, wrote the initial version of the manuscript. J.R. made substantial contributions to the conception and design of the work. S.B., R.P., M.C.M., G.M., F.L., M.Mo., A.O. contributed to the design of the work, data collection and interpretation. C.C., A.R., S.F., L.B., N.V., A.L., C.M.C, L.M. contributed to data collection and interpretation; L.G., P.M., A.R., C.S. contributed to data interpretation, wrote the initial version of the manuscript; B.C., M. Ma., and V.M. contributed to data collection and interpretation. F.C. made statistical analyses; A.D.F. contributed to the conception and design of the work, data interpretation, manuscript revision; M.P. contributed to the conception and design of the work, data interpretation, manuscript revision, handling funding and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Research involving human participants and/or animals
The Ethics Committee of the Istituto Superiore di Sanità—National Institute of Health in Italy approved this study (AOO–ISS 01/07/2019 0020061).
Informed consent
A signed informed consent was not required from participants in this anonymous and voluntary questionnaire survey.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marconi, M., Pagano, M.T., Ristori, J. et al. Sociodemographic profile, health-related behaviours and experiences of healthcare access in Italian transgender and gender diverse adult population. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-024-02362-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-024-02362-x