Abstract
Background
The effect of sodium–glucose cotransporter 2 (SGLT2) inhibitors on cancer has yet to be fully elucidated.
Objective
This systematic review and meta-analysis investigated the effects of SGLT2 inhibitors on cancer.
Methods
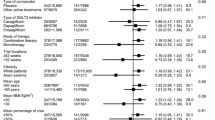
We searched the PubMed and ClinicalTrials.gov databases up to July 15, 2023, to identify eligible randomized, double-blind, placebo-controlled trials that lasted at least ≥24 weeks. The primary outcome was the overall cancer incidence, and the secondary outcomes were the incidences of various types of cancer. We used the Mantel–Haenszel method, fixed effects model, risk ratio (RR) and 95% confidence interval (CI) to analyze dichotomous variables. Subgroup analysis was performed based on the SGLT2 inhibitor type, baseline conditions, and follow-up duration. All meta-analyses were performed using RevMan5.4.1 and Stata MP 16.0.
Results
A total of 58 publications (59 trials) were included, comprising 113,909 participants with type 2 diabetes mellitus and/or chronic kidney disease and/or high cardiovascular risk and/or heart failure (SGLT2 inhibitor group, 63864; placebo group, 50045). Compared to the placebo SGLT2 inhibitors did not significantly increase the overall incidence of cancer (RR 1.01; 95% CI 0.94–1.08; p = 0.82). However, ertugliflozin did significantly increase the overall incidence of cancer (RR 1.29; 95% CI 1.01–1.64; p = 0.04). SGLT2 inhibitors did not increase the risks of bladder or breast cancer. However, dapagliflozin did significantly reduce the risk of bladder cancer by 47% (RR 0.53; 95% CI 0.35–0.81; p = 0.003). SGLT2 inhibitors had no significant effect on the risks of gastrointestinal, thyroid, skin, respiratory, prostate, uterine/endometrial, hepatic and pancreatic cancers. Dapagliflozin reduced the risk of respiratory cancer by 26% (RR 0.74; 95% CI 0.55–1.00; p = 0.05). SGLT2 inhibitors (particularly mediated by dapagliflozin and ertugliflozin but not statistically significant) were associated with a greater risk of renal cancer than the placebo (RR 1.39; 95% CI 1.04–1.87; p = 0.03).
Conclusion
SGLT2 inhibitors did not significantly increase the overall risk of cancer or the risks of bladder and breast cancers. However, the higher risk of renal cancer associated with SGLT2 inhibitors warrants concern.




Similar content being viewed by others
Availability of data and materials
If you have a reasonable request for relevant data, please send an email to the corresponding author.
Abbreviations
- T2DM:
-
Type 2 diabetes mellitus
- SGLT2:
-
Sodium-glucose cotransporter 2
- RR:
-
Risk ratio
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Pearson-Stuttard J, Papadimitriou N, Markozannes G et al (2021) Type 2 diabetes and cancer: an umbrella review of observational and mendelian randomization studies. Cancer Epidemiol Biomark Prev 30(6):1218–1228
Shlomai G, Neel B, LeRoith D, Gallagher EJ (2016) Type 2 diabetes mellitus and cancer: the role of pharmacotherapy. J Clin Oncol 34(35):4261–4269
Brown E, Heerspink HJL, Cuthbertson DJ, Wilding JPH (2021) SGLT2 inhibitors and GLP-1 receptor agonists: established and emerging indications. Lancet 398(10296):262–276
Zelniker TA, Wiviott SD, Raz I et al (2019) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 393(10166):31–39
Koepsell H (2017) The Na+-d-glucose cotransporters SGLT1 and SGLT2 are targets for the treatment of diabetes and cancer. Pharmacol Ther 170:148–165
Scafoglio C, Hirayama BA, Kepe V et al (2015) Functional expression of sodium-glucose transporters in cancer. Proc Natl Acad Sci USA 112(30):E4111–E4119
Burki TK (2012) FDA rejects novel diabetes drug over safety fears. Lancet 379(9815):507
Benedetti R, Benincasa G, Glass K et al (2022) Effects of novel SGLT2 inhibitors on cancer incidence in hyperglycemic patients: a meta-analysis of randomized clinical trials. Pharmacol Res 175:106039
Spiazzi BF, Naibo RA, Wayerbacher LF et al (2023) Sodium-glucose cotransporter-2 inhibitors and cancer outcomes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 198:110621
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors) (2019) Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane. www.training.cochrane.org/handbook
Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–926
Neal B, Perkovic V, Mahaffey KW et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657
Efficacy and safety of sotagliflozin versus placebo and empagliflozin in participants with type 2 diabetes mellitus who have inadequate glycemic control while taking a DPP4 inhibitor alone or with metformin (SOTA-EMPA). ClinicalTrials.gov. https://classic.clinicaltrials.gov/ct2/show/results/NCT03351478.
Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF (2013) Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med 11:43
Cherney DZI, Ferrannini E, Umpierrez GE et al (2021) Efficacy and safety of sotagliflozin in patients with type 2 diabetes and severe renal impairment. Diabetes Obes Metab 23(12):2632–2642
Ferdinand KC, Izzo JL, Lee J et al (2019) Antihyperglycemic and blood pressure effects of empagliflozin in black patients with type 2 diabetes mellitus and hypertension. Circulation 139(18):2098–2109
Forst T, Guthrie R, Goldenberg R et al (2014) Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes on background metformin and pioglitazone. Diabetes Obes Metab 16(5):467–477
Wilding JP, Charpentier G, Hollander P et al (2013) Efficacy and safety of canagliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sulphonylurea: a randomised trial. Int J Clin Pract 67(12):1267–1282
Kohan DE, Fioretto P, Tang W, List JF (2014) Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int 85(4):962–971
Yale JF, Bakris G, Cariou B et al (2014) Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes mellitus and chronic kidney disease. Diabetes Obes Metab 16(10):1016–1027
Efficacy and Safety of Sotagliflozin Versus Placebo in Patients With Type 2 Diabetes Mellitus on Background of Metformin. ClinicalTrials.gov. https://classic.clinicaltrials.gov/ct2/show/results/NCT02926950
Efficacy and safety of sotagliflozin versus glimepiride and placebo in participants with type 2 diabetes mellitus that are taking metformin monotherapy (SOTA-GLIM). ClinicalTrials.gov. https://classic.clinicaltrials.gov/ct2/show/NCT03332771
Bhatt DL, Szarek M, Pitt B et al (2021) Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med 384(2):129–139
Perkovic V, Jardine MJ, Neal B et al (2019) Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380(24):2295–2306
Heerspink HJL, Stefánsson BV, Correa-Rotter R et al (2020) Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383(15):1436–1446
Efficacy and Bone Safety of Sotagliflozin 400 and 200 mg Versus Placebo in Participants With Type 2 Diabetes Mellitus Who Have Inadequate Glycemic Control (SOTA-BONE). ClinicalTrials.gov. https://classic.clinicaltrials.gov/ct2/show/NCT03386344
Rosenstock J, Frias J, Páll D et al (2018) Effect of ertugliflozin on glucose control, body weight, blood pressure and bone density in type 2 diabetes mellitus inadequately controlled on metformin monotherapy (VERTIS MET). Diabetes Obes Metab 20(3):520–529
Tang H, Dai Q, Shi W, Zhai S, Song Y, Han J (2017) SGLT2 inhibitors and risk of cancer in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Diabetologia 60(10):1862–1872
Ueda P, Svanström H, Hviid A et al (2022) Sodium-glucose cotransporter 2 inhibitors and risk of bladder and renal cancer: scandinavian cohort study. Diabetes Care 45(5):e93–e96
Chung CT, Lakhani I, Chou OHI et al (2023) Sodium-glucose cotransporter 2 inhibitors versus dipeptidyl peptidase 4 inhibitors on new-onset overall cancer in type 2 diabetes mellitus: a population-based study. Cancer Med 12(11):12299–12315
Wu W, Wang Y, Xie J, Fan S (2023) Empagliflozin: a potential anticancer drug. Discov Oncol 14(1):127
Wang Y, Yang L, Mao L et al (2022) SGLT2 inhibition restrains thyroid cancer growth via G1/S phase transition arrest and apoptosis mediated by DNA damage response signaling pathways. Cancer Cell Int 22(1):74
Ali A, Mekhaeil B, Biziotis OD et al (2023) The SGLT2 inhibitor canagliflozin suppresses growth and enhances prostate cancer response to radiotherapy. Commun Biol 6(1):919
Wu W, Zhang Z, Jing D et al (2022) SGLT2 inhibitor activates the STING/IRF3/IFN-β pathway and induces immune infiltration in osteosarcoma. Cell Death Dis 13(6):523
Qiang W, Lei Y, Yuan L et al (2022) SGLT-2 as a potential target in pancreatic cancer: the preliminary clue from The Cancer Genome Atlas data. J Gastrointest Oncol 13(5):2539–2552
Kaji K, Nishimura N, Seki K et al (2018) Sodium glucose cotransporter 2 inhibitor canagliflozin attenuates liver cancer cell growth and angiogenic activity by inhibiting glucose uptake. Int J Cancer 142(8):1712–1722
Nalla LV, Khairnar A (2023) Empagliflozin mediated miR-128-3p upregulation promotes differentiation of hypoxic cancer stem-like cells in breast cancer. Eur J Pharmacol 943:175565
Grempler R, Thomas L, Eckhardt M et al (2012) Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors. Diabetes Obes Metab. 14(1):83–90
Kuang H, Liao L, Chen H, Kang Q, Shu X, Wang Y (2017) Therapeutic effect of sodium glucose co-transporter 2 inhibitor dapagliflozin on renal cell carcinoma. Med Sci Monit 23:3737–3745
Reilly TP, Graziano MJ, Janovitz EB et al (2014) Carcinogenicity risk assessment supports the chronic safety of dapagliflozin, an inhibitor of sodium-glucose co-transporter 2, in the treatment of type 2 diabetes mellitus. Diabetes Ther 5(1):73–96
Billger M, Kirk J, Chang J et al (2019) A study in a rat initiation-promotion bladder tumour model demonstrated no promoter/progressor potential of dapagliflozin. Regul Toxicol Pharmacol 103:166–173
Cahn A, Raz I, Bonaca M et al (2020) Safety of dapagliflozin in a broad population of patients with type 2 diabetes: analyses from the DECLARE-TIMI 58 study. Diabetes Obes Metab 22(8):1357–1368
Funding
This study was supported by the NSFC (82003872), Natural Science Foundation of Hunan Province (2022JJ50163, 2023JJ20034), Scientific Research Fund Project of Hunan Provincial Health Commission (20201973), Central government funds for guiding local scientific and Technological Development (2021QZY016), Hunan Province Clinical Medical Technology Innovation Guidance Project (2020SK51823, 2021SK51828, 2021SK51823), Hunan Provincial Clinical Medical Research Center for Drug Evaluation of major chronic diseases (2023SK4040). The science and technology innovation Program of Hunan Province (2023RC3173).
Author information
Authors and Affiliations
Contributions
Bo Xu and Jiecan Zhou provided topics and methods, while Bo Xu and Bo Kang completed literature search and data extraction. Bo Xu, Shaoqian Li, Shangzhi Fan completed the study selection. Bo Xu and Jiecan Zhou identified the outcome of interest. Bo Xu, Bo Kang, and Jiecan Zhou jointly completed the methodological quality assessment. Bo Xu is responsible for data analysis of the entire manuscript, providing tables and figures, and writing the article. All authors have undergone manuscript review. All authors have finally approved the manuscript and submitted it.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethics approval and consent to participate
Not applicable.
Code availability
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Research involving human participants and animals
No animals or humans were recruited for this study.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, B., Kang, B., Li, S. et al. Sodium-glucose cotransporter 2 inhibitors and cancer: a systematic review and meta-analysis. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-024-02351-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-024-02351-0