Abstract
Purpose
While it is common for menstrual cycles to cease within the initial 6 months of treatment, there are instances where some transgender men may not experience this cessation. We analyzed transgender men undergoing gender-affirming hormone therapy (GAHT) with testosterone who experienced breakthrough bleeding in order to identify the factors associated with this condition.
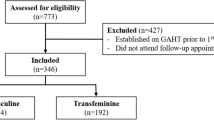
Methods
In this case–control study, 24 transgender men in the case group and 48 in the control group were assessed for clinical, sociodemographic, hormonal, and body composition variables using dual-energy X-ray absorptiometry. All participants had been on GATH for at least 6 months.
Results
A few transgender men experienced persistent breakthrough bleeding, which was associated with decreased testosterone levels and free androgen index (FAI) compared with controls (p = 0.002 and p = 0.008, respectively). Among individuals with breakthrough bleeding, 50% had testosterone levels below the lowest tertile calculated for the sample, compared with 18.8% on controls (p = 0.007). After therapy adjustment, testosterone levels increased compared with the values obtained in the initial bleeding episode (p = 0.031). Eight transgender men required the addition of an oral progestogen to achieve amenorrhea, and these individuals had higher BMI than those in whom the adjustment of the parenteral testosterone dose was adequate (p = 0.026). A univariate prevalence ratio analysis revealed a negative association of persistent bleeding with testosterone levels (p = 0.028) and FAI levels (p = 0.019).
Conclusion
Higher BMI and lower levels of testosterone and FAI were the main factors associated with breakthrough bleeding in transgender men.

Similar content being viewed by others
Data availability
Data are available after request directly to the authors.
References
Coleman E, Radix AE, Bouman WP et al (2022) Standards of care for the health of transgender and gender diverse people, Version 8. Int J Transgend Health. 23(1):S1-s259. https://doi.org/10.1080/26895269.2022.2100644
Hembree WC, Cohen-Kettenis PT, Gooren L et al (2017) Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab 102(11):3869–3903. https://doi.org/10.1210/jc.2017-01658
Silva DC, Salati LR, Fontanari AMV et al (2021) Prevalence of gender dysphoria in southern brazil: a retrospective study. Arch Sex Behav 50:3517–3526. https://doi.org/10.1007/s10508-021-02036-2
Klaver M, Dekker M, de Mutsert R, Twisk JWR, den Heijer M (2017) Cross-sex hormone therapy in transgender persons affects total body weight, body fat and lean body mass: a meta-analysis. Andrologia. https://doi.org/10.1111/and.12660
T’Sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V (2018) Endocrinology of transgender medicine. Endocr Rev 40(1):97–117. https://doi.org/10.1210/er.2018-00011
Wierckx K, Van Caenegem E, Schreiner T et al (2014) Cross-sex hormone therapy in trans persons is safe and effective at short-time follow-up: results from the European network for the investigation of gender incongruence. J Sex Med 11(8):1999–2011. https://doi.org/10.1111/jsm.12571
Costa R, Colizzi M (2016) The effect of cross-sex hormonal treatment on gender dysphoria individuals’ mental health: a systematic review. Neuropsychiatr Dis Treat 12:1953–1966. https://doi.org/10.2147/NDT.S95310
Silva ED, Fighera TM, Allgayer RM, Lobato MIR, Spritzer PM (2021) Physical and sociodemographic features associated with quality of life among transgender women and men using gender-affirming hormone therapy. Front Psychiatry 12:621075. https://doi.org/10.3389/fpsyt.2021.621075
Armuand G, Dhejne C, Olofsson JI, Rodriguez-Wallberg KA (2017) Transgender men’s experiences of fertility preservation: a qualitative study. Hum Reprod 32(2):383–390. https://doi.org/10.1093/humrep/dew323
Carswell JM, Roberts SA (2017) Induction and maintenance of amenorrhea in transmasculine and nonbinary adolescents. Transgender Health 2(1):195–201. https://doi.org/10.1089/trgh.2017.0021
Nakamura A, Watanabe M, Sugimoto M et al (2013) Dose-response analysis of testosterone replacement therapy in patients with female to male gender identity disorder. Endocr J 60(3):275–281. https://doi.org/10.1507/endocrj.EJ12-0319
Pradhan S, Gomez-Lobo V (2019) Hormonal contraceptives, intrauterine devices, gonadotropin-releasing hormone analogues and testosterone: menstrual suppression in special adolescent populations. J Pediatr Adolesc Gynecol 32(5):23–29. https://doi.org/10.1016/j.jpag.2019.04.007
Ahmad S, Leinung M (2017) The response of the menstrual cycle to initiation of hormonal therapy in transgender men. Transgender Health 2(1):176–179. https://doi.org/10.1089/trgh.2017.0023
Grimstad, Kremen J, Shim J, Charlton BM, Boskey ER (2021) Breakthrough bleeding in transgender and gender diverse adolescents and young adults on long-term testosterone. J Pediatr Adolesc Gynecol 34(5):706–716. https://doi.org/10.1016/j.jpag.2021.04.004
Grimstad, Fowler KG, New EP et al (2019) Uterine pathology in transmasculine persons on testosterone: a retrospective multicenter case series. Am J Obstet Gynecol 220(3):257.e251-257.e257. https://doi.org/10.1016/j.ajog.2018.12.021
Taub RL, Ellis SA, Neal-Perry G, Magaret AS, Prager SW, Micks EA (2020) The effect of testosterone on ovulatory function in transmasculine individuals. Am J Obstet Gynecol 223(2):229.e221-229.e228. https://doi.org/10.1016/j.ajog.2020.01.059
Perrone AM, Cerpolini S, Maria Salfi NC et al (2009) Effect of long-term testosterone administration on the endometrium of female-to-male (FtM) transsexuals. J Sex Med 6(11):3193–3200. https://doi.org/10.1111/j.1743-6109.2009.01380.x
Tuckerman EM, Okon MA, Li T-C, Laird SM (2000) Do androgens have a direct effect on endometrial function? an in vitro study. Fertil Steril 74(4):771–779. https://doi.org/10.1016/S0015-0282(00)00711-1
Trum HW, Hoebeke P, Gooren LJ (2015) Sex reassignment of transsexual people from a gynecologist’s and urologist’s perspective. Acta Obstet Gynecol Scand 94(6):563–567. https://doi.org/10.1111/aogs.12618
Zang H, Sahlin L, Masironi B, Eriksson E, Lindén HA (2007) Effects of testosterone treatment on endometrial proliferation in postmenopausal women. J Clin Endocrinol Metab 92(6):2169–2175. https://doi.org/10.1210/jc.2006-2171
Loverro G, Resta L, Dellino M, Cascarano MA, Loverro M, Mastrolia SA (2016) Uterine and ovarian changes during testosterone administration in young female-to-male transsexuals. Taiwan J Obstet Gynecol 55(5):686–691. https://doi.org/10.1016/j.tjog.2016.03.004
Khalifa MA, Toyama A, Klein ME, Santiago V (2019) Histologic features of hysterectomy specimens from female-male transgender individuals. Int J Gynecol Pathol. https://doi.org/10.1097/PGP.0000000000000548
Hawkins M, Deutsch MB, Obedin-Maliver J et al (2021) Endometrial findings among transgender and gender nonbinary people using testosterone at the time of gender-affirming hysterectomy. Fertil Steril 115(5):1312–1317. https://doi.org/10.1016/j.fertnstert.2020.11.008
Klaver M, van Velzen D, de Blok C et al (2022) Change in visceral fat and total body fat and the effect on cardiometabolic risk factors during transgender hormone therapy. J Clin Endocrinol Metab 107(1):e153–e164. https://doi.org/10.1210/clinem/dgab616
Kyinn M, Banks K, Leemaqz SY, Sarkodie E, Goldstein D, Irwig MS (2021) Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy. Int J Obes 45(12):2562–2569. https://doi.org/10.1038/s41366-021-00935-x
Velho I, Fighera TM, Ziegelmann PK, Spritzer PM (2017) Effects of testosterone therapy on BMI, blood pressure, and laboratory profile of transgender men: a systematic review. Andrology 5(5):881–888. https://doi.org/10.1111/andr.12382
American Psychiatric Association (2014) DSM-5: Manual diagnóstico e estatístico de transtornos mentais: Artmed Editora
Maeda SS, Peters BSE, Martini LA et al (2022) Official position of the Brazilian Association of Bone Assessment and Metabolism (ABRASSO) on the evaluation of body composition by densitometry: part I (technical aspects) general concepts, indications, acquisition, and analysis. Adv Rheumatol 62(1):7. https://doi.org/10.1186/s42358-022-00240-9
Pappas II, Craig WY, Spratt LV, Spratt DI (2020) Efficacy of sex steroid therapy without progestin or GnRH agonist for gonadal suppression in adult transgender patients. J Clin Endocrinol Metab 106(3):e1290–e1300. https://doi.org/10.1210/clinem/dgaa884
Defreyne J, Vanwonterghem Y, Collet S et al (2020) Vaginal bleeding and spotting in transgender men after initiation of testosterone therapy: a prospective cohort study (ENIGI). Int J Transgend Health 21(2):163–175. https://doi.org/10.1080/26895269.2020.1719951
Grynberg M, Fanchin R, Dubost G et al (2010) Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod BioMed Online 20(4):553–558. https://doi.org/10.1016/j.rbmo.2009.12.021
Stenzel AE et al (2020) Clinical needs for transgender men in the gynecologic oncology setting. Gynecol Oncol 159(3):899–905. https://doi.org/10.1016/j.ygyno.2020.09.038
Hetemäki N, Mikkola TS, Tikkanen MJ et al (2021) Adipose tissue estrogen production and metabolism in premenopausal women. J Steroid Biochem Mol Biol 209:105849. https://doi.org/10.1016/j.jsbmb.2021.105849
Ohlsson C, Nilsson ME, Tivesten Å et al (2013) Comparisons of immunoassay and mass spectrometry measurements of serum estradiol levels and their influence on clinical association studies in men. J Clin Endocrinol Metab 98(6):E1097–E1102. https://doi.org/10.1210/jc.2012-3861
Kumari P, Gaikwad HS, Nath B (2022) Endometrial cut off thickness as predictor of endometrial pathology in perimenopausal women with abnormal uterine bleeding: a cross-sectional study. Obstet Gynecol Int 2022:5073944. https://doi.org/10.1155/2022/5073944
Simpson AN, Lennox G (2021) Highlighting obesity as a risk factor for endometrial cancer. CMAJ 193(2):E58. https://doi.org/10.1503/cmaj.77367
Funding
This work was funded by the National Council for Scientific and Technological Development (grant number INCT/CNPq 465482/2014-7) and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (grant INCT/FAPERGS: 17/2551-0000519-8). The funding source had no role in the collection, analysis, interpretation of data and in the writing of the report or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
EDS contributed to study design, acquisition of data, analysis and interpretation of data, drafting the manuscript, and final review. TMF and PMS contributed to conception and study design, acquisition of data, analysis and interpretation of data, and final review of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Research involving human participants and/or animals
This study was approved by the Ethics Committee of Hospital de Clínicas de Porto Alegre, project number 2014-0608, and all participants signed an informed consent form and complies with the guidelines of the Declaration of Helsinki.
Informed consent
All patients have provided their written informed consent to participate to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
da Silva, E.D., Spritzer, P.M. & Fighera, T.M. Persistent vaginal bleeding during gender-affirming hormone therapy in transgender men. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-023-02296-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-023-02296-w