Abstract
Objective
The existing prediction models for metastasis in pheochromocytomas/paragangliomas (PPGLs) showed high heterogeneity in different centers. Therefore, this study aimed to establish new prediction models integrating multiple variables based on different algorithms.
Design and methods
Data of patients with PPGLs undergoing surgical resection at the Peking Union Medical College Hospital from 2007 to 2022 were collected retrospectively. Patients were randomly divided into the training and testing sets in a ratio of 7:3. Subsequently, decision trees, random forest, and logistic models were constructed for metastasis prediction with the training set and Cox models for metastasis-free survival (MFS) prediction with the total population. Additionally, Ki-67 index and tumor size were transformed into categorical variables for adjusting models. The testing set was used to assess the discrimination and calibration of models and the optimal models were visualized as nomograms. Clinical characteristics and MFS were compared between patients with and without risk factors.
Results
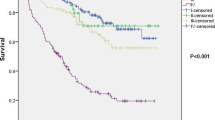
A total of 198 patients with 59 cases of metastasis were included and classified into the training set (n = 138) and testing set (n = 60). Among all models, the logistic regression model showed the best discrimination for metastasis prediction with an AUC of 0.891 (95% CI, 0.793–0.990), integrating SDHB germline mutations [OR: 96.72 (95% CI, 16.61–940.79)], S-100 (-) [OR: 11.22 (95% CI, 3.04–58.51)], ATRX (-) [OR: 8.42 (95% CI, 2.73–29.24)] and Ki-67 ≥ 3% [OR: 7.98 (95% CI, 2.27–32.24)] evaluated through immunohistochemistry (IHC), and tumor size ≥ 5 cm [OR: 4.59 (95% CI, 1.34–19.13)]. The multivariate Cox model including the above risk factors also showed a high C-index of 0.860 (95% CI, 0.810–0.911) in predicting MFS after surgery. Furthermore, patients with the above risk factors showed a significantly poorer MFS (P ≤ 0.001).
Conclusions
Models established in this study provided alternative and reliable tools for clinicians to predict PPGLs patients’ metastasis and MFS. More importantly, this study revealed for the first time that IHC of ATRX could act as an independent predictor of metastasis in PPGLs.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Beard CM, Sheps SG, Kurland LT, Carney JA, Lie JT (1983) Occurrence of pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin Proc 58(12):802–804
Lenders JW, Duh QY, Eisenhofer G et al (2014) Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(6):1915–1942. https://doi.org/10.1210/jc.2014-1498
Lam AK (2017) Update on adrenal tumours in 2017 world health organization (WHO) of endocrine tumours. Endocr Pathol 28(3):213–227. https://doi.org/10.1007/s12022-017-9484-5
Eisenhofer G, Bornstein SR, Brouwers FM et al (2004) Malignant pheochromocytoma: current status and initiatives for future progress. Endocr Relat Cancer 11(3):423–436. https://doi.org/10.1677/erc.1.00829
Hescot S, Leboulleux S, Amar L et al (2013) One-year progression-free survival of therapy-naive patients with malignant pheochromocytoma and paraganglioma. J Clin Endocrinol Metab 98(10):4006–4012. https://doi.org/10.1210/jc.2013-1907
Turkova H, Prodanov T, Maly M et al (2016) Characteristics and outcomes of metastatic sdhb and sporadic pheochromocytoma/paraganglioma: an national institutes of health study. Endocr Pract 22(3):302–314. https://doi.org/10.4158/ep15725.Or
Gimenez-Roqueplo AP, Favier J, Rustin P et al (2003) Mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res 63(17):5615–5621
King KS, Prodanov T, Kantorovich V et al (2011) Metastatic pheochromocytoma/paraganglioma related to primary tumor development in childhood or adolescence: significant link to SDHB mutations. J Clin Oncol 29(31):4137–4142. https://doi.org/10.1200/jco.2011.34.6353
Schovanek J, Martucci V, Wesley R et al (2014) The size of the primary tumor and age at initial diagnosis are independent predictors of the metastatic behavior and survival of patients with SDHB-related pheochromocytoma and paraganglioma: a retrospective cohort study. BMC Cancer 14:523. https://doi.org/10.1186/1471-2407-14-523
Hamidi O, Young WF Jr, Iñiguez-Ariza NM et al (2017) Malignant pheochromocytoma and paraganglioma: 272 patients over 55 years. J Clin Endocrinol Metab 102(9):3296–3305. https://doi.org/10.1210/jc.2017-00992
Ayala-Ramirez M, Feng L, Johnson MM et al (2011) Clinical risk factors for malignancy and overall survival in patients with pheochromocytomas and sympathetic paragangliomas: primary tumor size and primary tumor location as prognostic indicators. J Clin Endocrinol Metab 96(3):717–725. https://doi.org/10.1210/jc.2010-1946
Zelinka T, Musil Z, Dušková J et al (2011) Metastatic pheochromocytoma: does the size and age matter? Eur J Clin Invest 41(10):1121–1128. https://doi.org/10.1111/j.1365-2362.2011.02518.x
Cho YY, Kwak MK, Lee SE et al (2018) A clinical prediction model to estimate the metastatic potential of pheochromocytoma/paraganglioma: ASES score. Surgery 164(3):511–517. https://doi.org/10.1016/j.surg.2018.05.001
Strong VE, Kennedy T, Al-Ahmadie H et al (2008) Prognostic indicators of malignancy in adrenal pheochromocytomas: clinical, histopathologic, and cell cycle/apoptosis gene expression analysis. Surgery 143(6):759–768. https://doi.org/10.1016/j.surg.2008.02.007
Salmenkivi K, Heikkilä P, Haglund C, Louhimo J, Arola J (2003) Lack of histologically suspicious features, proliferative activity, and p53 expression suggests benign diagnosis in phaeochromocytomas. Histopathology 43(1):62–71. https://doi.org/10.1046/j.1365-2559.2003.01645.x
Feng F, Zhu Y, Wang X et al (2011) Predictive factors for malignant pheochromocytoma: analysis of 136 patients. J Urol 185(5):1583–1590. https://doi.org/10.1016/j.juro.2010.12.050
Eisenhofer G, Lenders JW, Siegert G et al (2012) Plasma methoxytyramine: a novel biomarker of metastatic pheochromocytoma and paraganglioma in relation to established risk factors of tumour size, location and SDHB mutation status. Eur J Cancer 48(11):1739–1749. https://doi.org/10.1016/j.ejca.2011.07.016
Crona J, Lamarca A, Ghosal S, Welin S, Skogseid B, Pacak K (2019) Genotype-phenotype correlations in pheochromocytoma and paraganglioma: a systematic review and individual patient meta-analysis. Endocr Relat Cancer 26(5):539–550. https://doi.org/10.1530/erc-19-0024
Thompson LD (2002) Pheochromocytoma of the adrenal gland scaled score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol 26(5):551–566. https://doi.org/10.1097/00000478-200205000-00002
Kimura N, Takayanagi R, Takizawa N et al (2014) Pathological grading for predicting metastasis in phaeochromocytoma and paraganglioma. Endocr Relat Cancer 21(3):405–414. https://doi.org/10.1530/erc-13-0494
Koh JM, Ahn SH, Kim H et al (2017) Validation of pathological grading systems for predicting metastatic potential in pheochromocytoma and paraganglioma. PLoS ONE 12(11):e0187398. https://doi.org/10.1371/journal.pone.0187398
Pierre C, Agopiantz M, Brunaud L et al (2019) COPPS, a composite score integrating pathological features, PS100 and SDHB losses, predicts the risk of metastasis and progression-free survival in pheochromocytomas/paragangliomas. Virchows Arch 474(6):721–734. https://doi.org/10.1007/s00428-019-02553-5
van Nederveen FH, Gaal J, Favier J et al (2009) An immunohistochemical procedure to detect patients with paraganglioma and phaeochromocytoma with germline SDHB, SDHC, or SDHD gene mutations: a retrospective and prospective analysis. Lancet Oncol 10(8):764–771. https://doi.org/10.1016/s1470-2045(09)70164-0
Lee H, Jeong S, Yu Y et al (2020) Risk of metastatic pheochromocytoma and paraganglioma in SDHx mutation carriers: a systematic review and updated meta-analysis. J Med Genet 57(4):217–225. https://doi.org/10.1136/jmedgenet-2019-106324
Zhang X, Lian P, Su M et al (2021) Single-cell transcriptome analysis identifies a unique tumor cell type producing multiple hormones in ectopic ACTH and CRH secreting pheochromocytoma. Elife. https://doi.org/10.7554/eLife.68436
Unger P, Hoffman K, Pertsemlidis D, Thung S, Wolfe D, Kaneko M (1991) S100 protein-positive sustentacular cells in malignant and locally aggressive adrenal pheochromocytomas. Arch Pathol Lab Med 115(5):484–487
Kumaki N, Kajiwara H, Kameyama K et al (2002) Prediction of malignant behavior of pheochromocytomas and paragangliomas using immunohistochemical techniques. Endocr Pathol Summer 13(2):149–156. https://doi.org/10.1385/ep:13:2:149
Job S, Draskovic I, Burnichon N et al (2019) Telomerase activation and ATRX mutations are independent risk factors for metastatic pheochromocytoma and paraganglioma. Clin Cancer Res 25(2):760–770. https://doi.org/10.1158/1078-0432.Ccr-18-0139
Singhi AD, Liu TC, Roncaioli JL et al (2017) Alternative lengthening of telomeres and loss of DAXX/ATRX expression predicts metastatic disease and poor survival in patients with pancreatic neuroendocrine tumors. Clin Cancer Res 23(2):600–609. https://doi.org/10.1158/1078-0432.Ccr-16-1113
Hsu YR, Torres-Mora J, Kipp BR et al (2019) Clinicopathological, immunophenotypic and genetic studies of mediastinal paragangliomas†. Eur J Cardiothorac Surg 56(5):867–875. https://doi.org/10.1093/ejcts/ezz115
Liau JY, Tsai JH, Jeng YM, Lee JC, Hsu HH, Yang CY (2015) Leiomyosarcoma with alternative lengthening of telomeres is associated with aggressive histologic features, loss of ATRX expression, and poor clinical outcome. Am J Surg Pathol 39(2):236–244. https://doi.org/10.1097/pas.0000000000000324
Liau JY, Tsai JH, Yang CY et al (2015) Alternative lengthening of telomeres phenotype in malignant vascular tumors is highly associated with loss of ATRX expression and is frequently observed in hepatic angiosarcomas. Hum Pathol 46(9):1360–1366. https://doi.org/10.1016/j.humpath.2015.05.019
Zhou Y 2023 Data from: Novel alternative tools for metastatic pheochromocytomas/paragangliomas prediction. https://doi.org/10.7910/DVN/HWBD74
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American college of medical genetics and genomics and the association for molecular pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Nölting S, Bechmann N, Taieb D et al (2022) Personalized management of pheochromocytoma and paraganglioma. Endocr Rev 43(2):199–239. https://doi.org/10.1210/endrev/bnab019
Cui Y, Ma X, Gao Y et al (2021) Local-regional recurrence of pheochromocytoma/paraganglioma: characteristics, risk factors and outcomes. Front Endocrinol (Lausanne) 12:762548. https://doi.org/10.3389/fendo.2021.762548
Dyer MA, Qadeer ZA, Valle-Garcia D, Bernstein E (2017) ATRX and DAXX: Mechanisms and mutations. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a026567
Yang CY, Liau JY, Huang WJ et al (2015) Targeted next-generation sequencing of cancer genes identified frequent TP53 and ATRX mutations in leiomyosarcoma. Am J Transl Res 7(10):2072–2081
Fishbein L, Khare S, Wubbenhorst B et al (2015) Whole-exome sequencing identifies somatic ATRX mutations in pheochromocytomas and paragangliomas. Nat Commun 6:6140. https://doi.org/10.1038/ncomms7140
Heaphy CM, de Wilde RF, Jiao Y et al (2011) Altered telomeres in tumors with ATRX and DAXX mutations. Science 333(6041):425. https://doi.org/10.1126/science.1207313
Pacurari M, Addison JB, Bondalapati N et al (2013) The microRNA-200 family targets multiple non-small cell lung cancer prognostic markers in H1299 cells and BEAS-2B cells. Int J Oncol 43(2):548–560. https://doi.org/10.3892/ijo.2013.1963
Acknowledgements
This research was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS) (grant number 2021-I2M-C&T-B-002), and the National High Level Hospital Clinical Research Funding (grant number 2022-PUMCH-C-028).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest, we do not have any possible conflicts of interest.
Ethical approval
This study was approved by the ethics committees of Peking Union Medical College Hospital (JS-3535).
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cui, Y., Zhou, Y., Gao, Y. et al. Novel alternative tools for metastatic pheochromocytomas/paragangliomas prediction. J Endocrinol Invest 47, 1191–1203 (2024). https://doi.org/10.1007/s40618-023-02239-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02239-5