Abstract
Objectives
To study the aggregation of multiple comorbidities in people with gout and explore differences in prognosis of gout flares among different subgroups.
Methods
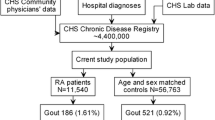
Hierarchical clustering was performed to identify homogeneous subgroups among 2639 people with gout using eight comorbidities. A one-year follow-up of acute gout flares in 463 of these people was conducted; the incidence and the timing of gout flares in each cluster were assessed to explore prognosis of gout flares. Binary logistic regression was applied to assess factors associated with gout flares.
Results
In baseline study, we identified five subgroups (C1–C5). C1 (n = 671, 25%) was characterized by isolated gout with few comorbidities. C2 (n = 258, 10%) were all obese. Almost all people in C3 (n = 335, 13%) had diabetes (99.7%). All people in C4 (n = 938, 36%) had dyslipidemia. C5 (n = 437, 17%) had the highest proportion of cardiovascular disease (CVD, 53%), chronic kidney disease (CKD, 56%), and cancer (7%). In follow-up study, C5 had the highest incidence (71.9%) and earliest onset (median 3 months) of gout flares. C2 had the lowest incidence (52.1%) and the latest onset (median 10 months) of gout flares. The highest relative risk for gout recurrent was seen for C5 (OR = 2.09). Other factors associated with the risk of gout flares were age at diagnosis of gout, duration of gout, presence of tophi, and smoking ≥ 20 cigarettes/day.
Conclusions
We clustered people with gout into five groups with varying comorbidities. People with CVD, CKD, and cancer had the highest risk of gout flares and should receive comprehensive care.




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kluck V, Jansen T, Janssen M, Comarniceanu A, Efde M, Tengesdal IW et al (2020) Dapansutrile, an oral selective NLRP3 inflammasome inhibitor, for treatment of gout flares: an open-label, dose-adaptive, proof-of-concept, phase 2a trial. Lancet Rheumatol 2(5):e270–e280. https://doi.org/10.1016/s2665-9913(20)30065-5
Bardin T, Richette P (2017) Impact of comorbidities on gout and hyperuricaemia: an update on prevalence and treatment options. BMC Med 15(1):123. https://doi.org/10.1186/s12916-017-0890-9
Rashid N, Levy GD, Wu YL, Zheng C, Koblick R, Cheetham TC (2015) Patient and clinical characteristics associated with gout flares in an integrated healthcare system. Rheumatol Int 35(11):1799–1807. https://doi.org/10.1007/s00296-015-3284-3
Rothenbacher D, Primatesta P, Ferreira A, Cea-Soriano L, Rodriguez LA (2011) Frequency and risk factors of gout flares in a large population-based cohort of incident gout. Rheumatology (Oxford) 50(5):973–981. https://doi.org/10.1093/rheumatology/keq363
Primatesta P, Plana E, Rothenbacher D (2011) Gout treatment and comorbidities: a retrospective cohort study in a large US managed care population. BMC Musculoskel Disord 12:103. https://doi.org/10.1186/1471-2474-12-103
Koto R, Nakajima A, Horiuchi H, Yamanaka H (2021) Serum uric acid control for prevention of gout flare in patients with asymptomatic hyperuricaemia: a retrospective cohort study of health insurance claims and medical check-up data in Japan. Ann Rheum Dis 80(11):1483–1490. https://doi.org/10.1136/annrheumdis-2021-220439
Richette P, Clerson P, Perissin L, Flipo RM, Bardin T (2015) Revisiting comorbidities in gout: a cluster analysis. Ann Rheum Dis 74(1):142–147. https://doi.org/10.1136/annrheumdis-2013-203779
Huang CF, Liu JC, Huang HC, Chuang SY, Chen CI, Lin KC (2017) Longitudinal transition trajectory of gouty arthritis and its comorbidities: a population-based study. Rheumatol Int 37(2):313–322. https://doi.org/10.1007/s00296-016-3634-9
Fatima T, Nilsson PM, Turesson C, Dehlin M, Dalbeth N, Jacobsson LTH et al (2020) The absolute risk of gout by clusters of gout-associated comorbidities and lifestyle factors-30 years follow-up of the Malmo Preventive Project. Arthrit Res Ther 22(1):244. https://doi.org/10.1186/s13075-020-02339-0
Bevis M, Blagojevic-Bucknall M, Mallen C, Hider S, Roddy E (2018) Comorbidity clusters in people with gout: an observational cohort study with linked medical record review. Rheumatology (Oxford) 57(8):1358–1363. https://doi.org/10.1093/rheumatology/key096
Bajpai R, Muller S, Mallen C, Watson L, Richette P, Hider SL et al (2021) Onset of comorbidities and flare patterns within pre-existing morbidity clusters in people with gout: 5-year primary care cohort study. Rheumatology (Oxford) 61(1):407–412. https://doi.org/10.1093/rheumatology/keab283
Alduraibi FK, Saleem M, Ricart K, Patel RP, Szalai AJ, Singh JA (2022) Clustering patients with gout based on comorbidities and biomarkers: a cross-sectional study. J Rheumatol. https://doi.org/10.3899/jrheum.220635
Choi HK, Ford ES, Li C, Curhan G (2007) Prevalence of the metabolic syndrome in patients with gout: the third national health and nutrition examination survey. Arthritis Rheum 57(1):109–115. https://doi.org/10.1002/art.22466
Berenson CS, Lashner B, Korman L, Hohmann E, Deshpande A, Louie TJ et al (2023) Prevalence of comorbid factors in patients with recurrent Clostridioides difficile infection in ECOSPOR III, a randomized trial of an oral microbiota-based therapeutic. Clin Infect Dis. https://doi.org/10.1093/cid/ciad448
Bluher M (2019) Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol 15(5):288–298. https://doi.org/10.1038/s41574-019-0176-8
Pillinger MH, Klein AB, Baumgartner S, Morlock R (2017) Cardiovascular disease and gout: real-world experience evaluating patient characteristics, treatment patterns, and health care utilization. J Manag Care Spec Pharm 23(6):677–683. https://doi.org/10.18553/jmcp.2017.23.6.677
Cipolletta E, Tata LJ, Nakafero G, Avery AJ, Mamas MA, Abhishek A (2022) Association between gout flare and subsequent cardiovascular events among patients with gout. JAMA 328(5):440–450. https://doi.org/10.1001/jama.2022.11390
Latourte A, Bardin T, Clerson P, Ea HK, Flipo RM, Richette P (2018) Dyslipidemia, alcohol consumption, and obesity as main factors associated with poor control of urate levels in patients receiving urate-lowering therapy. Arthritis Care Res (Hoboken) 70(6):918–924. https://doi.org/10.1002/acr.23347
Tsushima Y, Nishizawa H, Tochino Y, Nakatsuji H, Sekimoto R, Nagao H et al (2013) Uric acid secretion from adipose tissue and its increase in obesity. J Biol Chem 288(38):27138–27149. https://doi.org/10.1074/jbc.M113.485094
Zhang X, Zhu C, Gao J, Mei F, Yin J, Bu L et al (2018) Gender difference in the relationship between serum uric acid reduction and improvement in body fat distribution after laparoscopic sleeve gastrectomy in Chinese obese patients: a 6-month follow-up. Lipids Health Dis 17(1):288. https://doi.org/10.1186/s12944-018-0934-y
Kim JW, Choe JY, Park SH (2022) Metformin and its therapeutic applications in autoimmune inflammatory rheumatic disease. Korean J Intern Med 37(1):13–26. https://doi.org/10.3904/kjim.2021.363
Ji L, Jiang H, An P, Deng H, Liu M, Li L, Feng L, Song B, Han-Zhang H, Ma Q, Qian L (2021) IBI362 (LY3305677), a weekly-dose GLP-1 and glucagon receptor dual agonist, in Chinese adults with overweight or obesity: a randomised, placebo-controlled, multiple ascending dose phase 1b study. EClinicalMedicine. https://doi.org/10.1016/j.eclinm.2021.101088
Pei L, Xie L, Wu J, Zhang H, Zhang X (2020) Study on the relationship between FFA and gout flare. Clin Rheumatol 39(4):1251–1255. https://doi.org/10.1007/s10067-019-04903-9
Acknowledgements
We thank the trial staff as well as all people with gout who agreed to participate in this study.
Funding
This study was supported by the National Key R&D Programme of China (2019YFA0904500, 2022YFC2503300), the National Natural Science Foundation of China (81870616, 82170904), the Clinical Trial Programme of Shanghai Municipal Health Commission (202240130), the Clinical Trial Programme of Shanghai No.10 Hospital (YNCR2A009), and Medical enterprise integration Innovation achievement transformation Programme of Shanghai Shen-kang Hospital Development Centre (SHDC2022CRD042) to HC.
Author information
Authors and Affiliations
Contributions
SL: designed the study, analyzed and interpreted the data, and wrote the paper. HS: participated in the conception of the study. SY, NL and YG: participated in the collection of trial data. SQ and HC made critical revisions to the original manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of Shanghai Tenth People’s Hospital. It was conducted in accordance with the Declaration of Helsinki and the Guidelines for Good Clinical Practice.
Informed consent
All participants gave written informed consent before taking part in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Sun, H., Yang, S. et al. Clustering of gout-related comorbidities and their relationship with gout flares: a data-driven cluster analysis of eight comorbidities. J Endocrinol Invest 47, 1119–1128 (2024). https://doi.org/10.1007/s40618-023-02224-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02224-y