Abstract
Purpose
We aimed to identify whether hypothalamic–pituitary–adrenal (HPA) axis dysfunction is related to deterioration in a percentage of patients who progress to severe COVID-19.
Methods
In this cohort observational study, we evaluated HPA axis activation by measuring cortisol, adrenocorticotropic hormone (ACTH), dehydroepiandrosterone sulfate (DHEA-S) levels, whole blood expression levels of the key glucocorticoid receptor, GCR-α, and the glucocorticoid-induced leucine zipper (GILZ), and cytokines, as markers of the inflammatory phase, in 149 patients with respiratory infection admitted in the ward, without known adrenal disease and/or confounding medications (glucocorticoids). One hundred and four (104) patients were SARS-CoV-2 positive (C +) and controls consisted of 45 SARS-CoV-2-negative patients (NC).
Results
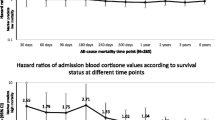
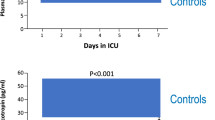
No differences in cortisol levels were observed between the C + and the NC patients. Cortisol levels correlated with ACTH (r = 0.284, p = 0.001) and IL-6 (r = 0.289, p = 0.04). In C + patients, cortisol levels mainly correlated with IL-6 levels (r = 0.28; p = 0.017). GCR-α expression was significantly higher in C + patients compared to NC. Patients with higher cortisol levels were more likely to progress to respiratory function deterioration or die. Both GCR-α and GILZ expression were significantly higher in C + non-survivors.
Conclusion
Our findings indicate that cortisol serves as an indicator of disease severity. GILZ expression appears to be a more effective marker of mortality prediction in moderate COVID-19 cases. However, routine measurement of GILZ levels is currently unavailable. Elevated levels of cortisol may be indicative of patients with moderate COVID-19 who are at a higher risk of deterioration. This information can aid in identifying individuals who require early medical attention.
Similar content being viewed by others
Data availability
Data are available upon reasonable request.
References
Wong CKH, Wong JYH, Tang EHM, Au CH, Wai AKC (2020) Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis. Sci Rep 10:19765
Ramasamy S, Subbian S (2021) Critical Determinants of Cytokine Storm and Type I Interferon Response in COVID-19 Pathogenesis. Clinical microbiology reviews 34.
Thakur M, Datusalia AK, Kumar A (2022) Use of steroids in COVID-19 patients: a meta-analysis. Eur J Pharmacol 914:174579
Boonen E, Bornstein SR, Van den Berghe G (2015) New insights into the controversy of adrenal function during critical illness. Lancet Diabetes Endocrinol 3:805–815
Kanczkowski W, Evert K, Stadtmüller M, Haberecker M, Laks L, Chen LS, Frontzek K, Pablik J, Hantel C, Beuschlein F, Kurth T, Gruber S, Aguzzi A, Varga Z, Bornstein SR (2022) COVID-19 targets human adrenal glands. Lancet Diabetes Endocrinol 10:13–16
Quatrini L, Ugolini S (2021) New insights into the cell- and tissue-specificity of glucocorticoid actions. Cell Mol Immunol 18:269–278
Vassiliou AG, Athanasiou N, Keskinidou C, Jahaj E, Tsipilis S, Zacharis A, Botoula E, Diamantopoulos A, Ilias I, Vassiliadi DA, Tsagarakis S, Kotanidou A, Dimopoulou I (2019) Increased Glucocorticoid Receptor Alpha Expression and Signaling in Critically Ill Coronavirus Disease 2019 Patients. Crit Care Med 49(2021):2131–2136
Kanczkowski W, Gaba WH, Krone N, Varga Z, Beuschlein F, Hantel C, Andoniadou C, Bornstein SR (2022) Adrenal gland function and dysfunction during COVID-19. Hormone Metabolic Res 54:532–539
Marik PE, Pastores SM, Annane D, Meduri GU, Sprung CL, Arlt W, Keh D, Briegel J, Beishuizen A, Dimopoulou I, Tsagarakis S, Singer M, Chrousos GP, Zaloga G, Bokhari F, Vogeser M, M American College of Critical Care (2008) Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med 36:1937–49
Tan T, Khoo B, Mills EG, Phylactou M, Patel B, Eng PC, Thurston L, Muzi B, Meeran K, Prevost AT, Comninos AN, Abbara A, Dhillo WS (2020) Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol 8:659–660
Das L, Dutta P, Walia R, Mukherjee S, Suri V, Puri GD, Mahajan V, Malhotra P, Chaudhary S, Gupta R, Jayant SS, Agrawal K, Kumar V, Sachdeva N, Rastogi A, Bhadada SK, Ram S, Bhansali A (2021) Spectrum of endocrine dysfunction and association with disease severity in patients with COVID-19: insights from a cross-sectional, observational study. Front Endocrinol 12:645787
Güven M, Gültekin H (2021) Could serum total cortisol level at admission predict mortality due to coronavirus disease 2019 in the intensive care unit? a prospective study. Sao Paulo Med J 139:398–404
Bornstein SR, Engeland WC, Ehrhart-Bornstein M, Herman JP (2008) Dissociation of ACTH and glucocorticoids. Trends Endocrinol Metab 19:175–180
Alzahrani AS, Mukhtar N, Aljomaiah A, Aljamei H, Bakhsh A, Alsudani N, Elsayed T, Alrashidi N, Fadel R, Alqahtani E, Raef H, Butt MI, Sulaiman O (2021) The Impact of COVID-19 Viral Infection on the Hypothalamic-Pituitary-Adrenal Axis. Endocrine practice 27:83–89
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Athanasiou, N., Diamantopoulos, A., Keskinidou, C. et al. Adrenal function in relation to cytokines and outcome in non-critically ill patients with COVID-19. J Endocrinol Invest 47, 721–728 (2024). https://doi.org/10.1007/s40618-023-02189-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02189-y