Abstract
Purpose
There is little information on factors that influence the glycemic variability (GV) during the nocturnal and diurnal periods. We aimed to examine the relationship between clinical factors and GV during these two periods.
Methods
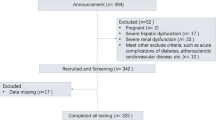
This cross-sectional study included 134 patients with type 2 diabetes. 24-h changes in blood glucose were recorded by a continuous glucose monitoring system. Nocturnal and diurnal GV were assessed by standard deviation of blood glucose (SDBG), coefficient of variation (CV), and mean amplitude of glycemic excursions (MAGE), respectively. Robust regression analyses were performed to identify the factors associated with GV. Restricted cubic splines were used to determine dose–response relationship.
Results
During the nocturnal period, age and glycemic level at 12:00 A.M. were positively associated with GV, whereas alanine aminotransferase was negatively associated with GV. During the diurnal period, homeostatic model assessment 2-insulin sensitivity (HOMA2-S) was positively associated with GV, whereas insulin secretion-sensitivity index-2 (ISSI2) was negatively associated with GV. Additionally, we found a J-shape association between the glycemic level at 12:00 A.M. and MAGE, with 9.0 mmol/L blood glucose level as a cutoff point. Similar nonlinear associations were found between ISSI2 and SDBG, and between ISSI2 and MAGE, with ISSI2 value of 175 as a cutoff point.
Conclusion
Factors associated with GV were different between nocturnal and diurnal periods. The cutoff points we found in this study may provide the therapeutic targets for beta-cell function and pre-sleep glycemic level in clinical practice.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
American Diabetes Association (2021) 6. Glycemic targets: standards of medical care in diabetes-2021. Diabetes Care 44:S73–S84
Martinez M, Santamarina J, Pavesi A et al (2021) Glycemic variability and cardiovascular disease in patients with type 2 diabetes. BMJ Open Diabetes Res Care 9:e002032
Huang Y, Heng C, Wei J et al (2017) Influencing factors of glycemic variability in hospitalized type 2 diabetes patients with insulin therapy: a strobe-compliant article. Medicine (Baltimore) 96:e8021
Brownlee M, Hirsch IB (2006) Glycemic variability: a hemoglobin A1c-independent risk factor for diabetic complications. JAMA 295:1707–1708
Sun B, Luo Z, Zhou J (2021) Comprehensive elaboration of glycemic variability in diabetic macrovascular and microvascular complications. Cardiovasc Diabetol 20:9
Monnier L, Colette C (2008) Glycemic variability: should we and can we prevent it? Diabetes Care 31:S150–S154
Jin SM, Kim TH, Bae JC et al (2014) Clinical factors associated with absolute and relative measures of glycemic variability determined by continuous glucose monitoring: an analysis of 480 subjects. Diabetes Res Clin Pract 104:266–272
Tanaka C, Saisho Y, Tanaka K et al (2013) Factors associated with glycemic variability in Japanese patients with diabetes. Diabetol Int 5:36–42
Chinese Diabetes Society (2021) Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes Mellitus 13:332–335
National Institute of Diabetes and Digestive and Kidney Diseases (2021) CKD-EPI calculator for adults (SI Units). https://www.niddk.nih.gov/health-26information/professionals/clinical-tools-patient-management/kidneydisease/laboratory-evaluation/glomerular-filtration-rate-calculators/ckd-epiadults-si-units. Accessed 12 Nov 2021
Kramer CK, Choi H, Zinman B, Retnakaran R (2014) Glycemic variability in patients with early type 2 diabetes: the impact of improvement in β-cell function. Diabetes Care 37:1116–1123
Diabetes Trials Unit (2021) A software implimentation of the HOMA2 model. http://www.dtu.ox.ac.uk/homa. Accessed 13 Oct 2021
Danne T, Nimri R, Battelino T et al (2017) International consensus on use of continuous glucose monitoring. Diabetes Care 40:1631–1640
Kovatchev BP (2017) Metrics for glycaemic control - from HbA1c to continuous glucose monitoring. Nat Rev Endocrinol 13:425–436
Nuffield Department of Primary Care Health Sciences Medical Sciences Division, University of Oxford (2021) EasyGV. https://www.phc.ox.ac.uk/research/resources/easygv. Accessed 10 Oct 2021
Gallieni M, De Salvo C, Lunati ME et al (2021) Continuous glucose monitoring in patients with type 2 diabetes on hemodialysis. Acta Diabetol 58:975–981
Pinckney A, Rigby MR, Keyes-Elstein L, Soppe CL, Nepom GT, Ehlers MR (2016) Correlation among hypoglycemia, glycemic variability, and C-peptide preservation after Alefacept therapy in patients with type 1 diabetes mellitus: analysis of data from the Immune Tolerance Network T1DAL Trial. Clin Ther 38:1327–1339
Lunati ME, Fiorina P (2022) Antigen-based immunotherapy improves glycemic metrics and beta-cell function. J Clin Endocrinol Metab 107:e4250–e4251
Bolla AM, Montefusco L, Pastore I, Lunati ME, Ben Nasr M, Fiorina P (2022) Benefits and hurdles of pancreatic beta-cell replacement. Stem Cells Transl Med 11:1029–1039
ElSayed NA, Aleppo G, Aroda VR et al (2023) 13. Older adults: standards of care in diabetes-2023. Diabetes Care 46:S216–S229
Mathieu C, Martens PJ, Vangoitsenhoven R (2021) One hundred years of insulin therapy. Nat Rev Endocrinol 17:715–725
Uemura F, Okada Y, Torimoto K, Tanaka Y (2018) Relation between hypoglycemia and glycemic variability in type 2 diabetes patients with insulin therapy: a study based on continuous glucose monitoring. Diabetes Technol Ther 20:140–146
Pathak RD, Schroeder EB, Seaquist ER et al (2016) Severe hypoglycemia requiring medical intervention in a large cohort of adults with diabetes receiving care in US integrated health care delivery systems: 2005–2011. Diabetes Care 39:363–370
Birkenfeld AL, Shulman GI (2014) Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology 59:713–723
Meshkani R, Adeli K (2009) Hepatic insulin resistance, metabolic syndrome and cardiovascular disease. Clin Biochem 42:1331–1346
Bonnet F, Ducluzeau PH, Gastaldelli A et al (2011) Liver enzymes are associated with hepatic insulin resistance, insulin secretion, and glucagon concentration in healthy men and women. Diabetes 60:1660–1667
Funding
This work was supported by National Natural Science Foundation of China [82073648], Shandong Research Hospital Association [2022023], Shandong Provincial Natural Science Foundation [ZR2021QH135], Doctoral Fund of Jining NO.1 People’s Hospital [2022-BS-008], and Traditional Chinese Medicine Science and Technology Development Plan of Shandong Province [Q-2022026]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: JJ, ZX, YH. Methodology: ZX, DZ, YZ, YH. Acquisition of data: JJ, FL, WW, SD, JZ, JS. Formal analysis: ZX. Interpretation of data: JJ, ZX, YL, YH, JS. Writing—original draft preparation: ZX. Writing—review and editing: JJ, DZ, YL, XS, QZ, YZ, YZ, HYG, YH, JS. Funding acquisition: JJ, YH. Supervision: JJ, YH. Final approval of the manuscript: All authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Medical Ethics Committee of Shandong First Medical University (No. JNMC-2022-YX-019).
Informed consent
The requirement for informed consent was waived because we used deidentified retrospective data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, J., Xia, Z., Zheng, D. et al. Factors associated with nocturnal and diurnal glycemic variability in patients with type 2 diabetes: a cross-sectional study. J Endocrinol Invest 47, 245–253 (2024). https://doi.org/10.1007/s40618-023-02142-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02142-z