Abstract
Aim
To evaluate sleep architecture of patients with Cushing’s disease (CD) and to explore whether agouti-related peptide (AgRP) and/or leptin play a permissive role in sleep alterations in patients with active CD.
Methods
We performed polysomnography on 26 patients with active CD and age 26 age- and sex-matched control subjects. Blood samples were obtained from all participants for the analyzes of AgRP and leptin. The laboratory and sleep-related parameters were compared.
Results
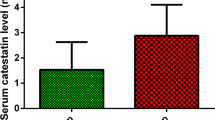
The groups were similar in age, gender, and body mass index. The CD group had reduced sleep efficiency (71.6 ± 12.1% vs. 78.8 ± 12.6%, p = 0.042) and increased wake after sleep onset (WASO%) (24.7 ± 13.1% vs. 17.4 ± 11.6%, p = 0.040) as compared to control group. Seventeen patients with CD (65.4%) and 18 control subjects (69.2%) had obstructive sleep apnea. Serum AgRP (13.2 ± 7.4 pg/ml vs. 9 ± 3.1, p = 0.029), leptin (59.5 mcg/l, [IQR] 32.6–94.6 vs. 25.3 mcg/l, [IQR] 12.9–57.5, p = 0.007) were higher in CD group. AgRP and leptin correlated negatively with total sleep time, sleep efficiency, stage N2 sleep (%), and positively with WASO%. In multiple regression analyses, serum cortisol (ß = − 0.359, p = 0.042) and AgRP (ß = − 0.481, p = 0.01) were significant predictor of sleep efficiency. AgRP was also significant predictor of WASO% (ß = 0.452 and p < 0.05).
Conclusions
Active CD carries an increased risk of impaired sleep efficiency and continuity which may worsen health-related quality of life. Elevated circulating AgRP and, to a lesser extent, leptin may be associated with decreased sleep efficiency and continuity in patients with CD. Patients with CD who have subjective sleep symptoms should be screened with polysomnography.



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article [and/or] its tables. The data repository can be provided upon request. Further inquiries can be directed to the corresponding author.
References
Starkman MN, Schteingart DE, Schork MA (1981) Depressed mood and other psychiatric manifestations of Cushing’s syndrome: relationship to hormone levels. Psychosom Med 43:3–18
Shipley JE, Schteingart DE, Tandon R et al (1992) Sleep architecture and sleep apnea in patients with Cushing’s disease. Sleep 15:514–518
Starkman MN, Schteingart DE (1981) Neuropsychiatric manifestations of patients with Cushing’s syndrome: relationship to cortisol and adrenocorticotropic hormone levels. Arch Intern Med 141:215–219
Ismailogullari S, Karaca Z, Firat ST et al (2021) Cushing syndrome is associated with increased stage N2 sleep and decreased SWS partially reversible after treatment. Horm Metab Res 53:608–615
Friedman TC, García-Borreguero D, Hardwick D et al (1994) Decreased delta-sleep and plasma delta-sleep-inducing peptide in patients with Cushing syndrome. Neuroendocrinology 60:626–634
Mazziotti G, Giustina A (2013) Glucocorticoids and the regulation of growth hormone secretion. Nat Rev Endocrinol 9:265–276
Buckley TM, Schatzberg AF (2005) On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab 90:3106–3114
Steiger A (2002) Sleep and the hypothalamo–pituitary–adrenocortical system. Sleep Med Rev 6:125–138
Bottini P, Tantucci C (2003) Sleep apnea syndrome in endocrine diseases. Respiration 70:320–327
Danguir J, Nicolaïdis S, Gerard H (1979) Relations between feeding and sleep patterns in the rat. J Comp Physiol Psychol 93:820
Garcı́a-Garcı́a F, Drucker-Colı́n R (1999) Endogenous and exogenous factors on sleep–wake cycle regulation. Progr Neurobiol 58:297–314
Richter C, Woods IG, Schier AF (2014) Neuropeptidergic control of sleep and wakefulness. Annu Rev Neurosci 37:503–531
Ollmann MM, Wilson BD, Yang Y-K et al (1997) Antagonism of central melanocortin receptors in vitro and in vivo by agouti-related protein. Science 278:135–138
Park H-K, Ahima RS (2015) Physiology of leptin: energy homeostasis, neuroendocrine function and metabolism. Metabolism 64:24–34
Cedernaes J, Huang W, Ramsey KM et al (2019) Transcriptional basis for rhythmic control of hunger and metabolism within the AgRP neuron. Cell Metab 29:1078-1091.e1075
Goldstein N, Levine BJ, Loy KA et al (2018) Hypothalamic neurons that regulate feeding can influence sleep/wake states based on homeostatic need. Curr Biol 28(3736–3747):e3733
Koo M, Lai N-S, Chiang J-K (2013) Short duration of sleep is associated with hyperleptinemia in Taiwanese adults. J Clin Sleep Med 9:1049–1055
Olson CA, Hamilton NA, Somers VK (2016) Percentage of REM sleep is associated with overnight change in leptin. J Sleep Res 25:419–425
Sinton CM, Fitch TE, Gershenfeld HK (1999) The effects of leptin on REM sleep and slow wave deltain rats are reversed by food deprivation. J Sleep Res 8:197–203
Laposky AD, Shelton J, Bass J et al (2006) Altered sleep regulation in leptin-deficient mice. Am J Physiol-Regul, Integr Comp Physiol 290:R894–R903
Laposky AD, Bradley MA, Williams DL et al (2008) Sleep-wake regulation is altered in leptin-resistant (db/db) genetically obese and diabetic mice. Am J Physiol-Regul, Integr Comp Physiol 295:R2059–R2066
Page-Wilson G, Freda PU, Jacobs TP et al (2014) Clinical utility of plasma POMC and AgRP measurements in the differential diagnosis of ACTH-dependent Cushing’s syndrome. J Clin Endocrinol Metab 99:E1838-1845
Page-Wilson G, Peters JB, Panigrahi SK et al (2019) Plasma agouti-related protein and cortisol levels in cushing disease: evidence for the regulation of agouti-related protein by glucocorticoids in humans. J Clin Endocrinol Metab 104:961–969
Veldman RG, Frolich M, Pincus SM et al (2001) Hyperleptinemia in women with Cushing’s disease is driven by high-amplitude pulsatile, but orderly and eurhythmic, leptin secretion. Eur J Endocrinol 144:21–27
Schafroth U, Godang K, Ueland T et al (2000) Leptin levels in relation to body composition and insulin concentration in patients with endogenous Cushing’s syndrome compared to controls matched for body mass index. J Endocrinol Invest 23:349–355
Nieman LK, Biller BMK, Findling JW et al (2008) The diagnosis of Cushing’s syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 93:1526–1540
Association AD (2020) 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care 43:S66–S76
James PA, Oparil S, Carter BL et al (2014) 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA 311:507–520
Berry RB, Brooks R, Gamaldo CE et al (2012) The AASM manual for the scoring of sleep and associated events. Rules Terminol Tech Specific Darien Illinois Am Acad Sleep Med 176:2012
Medicine AAoS International Classification of Sleep Disorders 2014 3rd ed Darien. IL American Academy of Sleep Medicine. pp 246–253
Johns MW (2000) Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res 9:5–11
Buysse DJ, Reynolds CF III, Monk TH et al (1991) Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 14:331–338
Bertagna X, Guignat L (2013) Approach to the Cushing’s disease patient with persistent/recurrent hypercortisolism after pituitary surgery. J Clin Endocrinol Metab 98:1307–1318
D’Angelo V, Beccuti G, Berardelli R et al (2015) Cushing’s syndrome is associated with sleep alterations detected by wrist actigraphy. Pituitary 18:893–897
Romijn JA (2016) Pituitary diseases and sleep disorders. Curr Opin Endocrinol Diabetes Obes 23:345–351
Krieger D (1975) Sleep EEG stages and growth hormone levels in endogenous and exogenous hyper-cortisolemia or ACTH elevation. Prog Brain Res 42:121
Krieger DT, Glick SM (1974) Sleep EEG stages and plasma growth hormone concentration in states of endogenous and exogenous hypercortisolemia or ACTH elevation. J Clin Endocrinol Metab 39:986–1000
Zakrzewska KE, Cusin I, Stricker-Krongrad A et al (1999) Induction of obesity and hyperleptinemia by central glucocorticoid infusion in the rat. Diabetes 48:365–370
Panigrahi SK, Toedesbusch CD, McLeland JS et al (2020) Diurnal patterns for cortisol, cortisone and agouti-related protein in human cerebrospinal fluid and blood. J Clin Endocrinol Metab 105:e1584-1592
Padilla SL, Qiu J, Soden ME et al (2016) Agouti-related peptide neural circuits mediate adaptive behaviors in the starved state. Nat Neurosci 19:734–741
Shibata M, Banno R, Sugiyama M et al (2016) AgRP neuron-specific deletion of glucocorticoid receptor leads to increased energy expenditure and decreased body weight in female mice on a high-fat diet. Endocrinology 157:1457–1466
Hagimoto S, Arima H, Adachi K et al (2013) Expression of neuropeptide Y and agouti-related protein mRNA stimulated by glucocorticoids is attenuated via NF-κB p65 under ER stress in mouse hypothalamic cultures. Neurosci Lett 553:165–169
Shimizu H, Arima H, Watanabe M et al (2008) Glucocorticoids increase neuropeptide Y and agouti-related peptide gene expression via adenosine monophosphate-activated protein kinase signaling in the arcuate nucleus of rats. Endocrinology 149:4544–4553
Szentirmai É (2012) Central but not systemic administration of ghrelin induces wakefulness in mice. PLoS ONE 7:e41172
Weber F, Dan Y (2016) Circuit-based interrogation of sleep control. Nature 538:51–59
Ramírez-Plascencia OD, Saderi N, Cárdenas-Romero S et al (2022) Leptin and adiponectin regulate the activity of nuclei involved in sleep-wake cycle in male rats. Front Neurosci. https://doi.org/10.3389/fnins.2022.907508
Megirian D, Dmochowski J, Farkas GA (1998) Mechanism controlling sleep organization of the obese Zucker rats. J Appl Physiol 84:253–256
Hirota T, Morioka T, Yoda K et al (2018) Positive association of plasma leptin with sleep quality in obese type 2 diabetes patients. J Diabetes Investig 9:1100–1105
Friess E, Wiedemann K, Steiger A et al (1995) The hypothalamic-pituitary-adrenocortical system and sleep in man. Adv Neuroimmunol 5:111–125
Leal-Cerro A, Soto A, Martínez MA et al (2001) Influence of cortisol status on leptin secretion. Pituitary 4:111–116
Pan W, Kastin AJ (2014) Leptin: a biomarker for sleep disorders? Sleep Med Rev 18:283–290
Knutson K, Galli G, Zhao X et al (2011) NIDDK sleep extension study. No association between leptin levels and sleep duration or quality in obese adults. Obesity 19:2433–2435
Capers PL, Fobian AD, Kaiser KA et al (2015) A systematic review and meta-analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obes Rev 16:771–782
Pattipati M, Gudavalli G (2022) Association between Cushing’s syndrome and sleep apnea: results from the national inpatient sample. Cureus 14:e22044
Gokosmanoğlu F, Güzel A, Kan EK et al (2017) Increased prevalence of obstructive sleep apnea in patients with Cushing’s syndrome compared with weight- and age-matched controls. Eur J Endocrinol 176:267–272
Buysse DJ, Reynolds CF 3rd, Monk TH et al (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Sagan KP, Andrysiak-Mamos E, Tyburski E et al (2021) Quality of life and sleep in patients with pituitary adenoma in relation to tumor type and compression of the optic chiasm. J Clin Med 10:1879
Chen DM, Taporoski TP, Alexandria SJ et al (2023) Altered sleep architecture in diabetes and prediabetes: findings from the Baependi Heart Study. medRxiv. 252:125
Yoda K, Inaba M, Hamamoto K et al (2015) Association between poor glycemic control, impaired sleep quality, and increased arterial thickening in type 2 diabetic patients. PLoS ONE 10:e0122521
Pallayova M, Donic V, Gresova S et al (2010) Do differences in sleep architecture exist between persons with type 2 diabetes and nondiabetic controls? J Diabetes Sci Technol 4:344–352
Kajbaf F, Fendri S, Basille-Fantinato A et al (2014) The relationship between metformin therapy and sleep quantity and quality in patients with Type 2 diabetes referred for potential sleep disorders. Diabet Med 31:577–580
Funding
The present study was funded by Scientific Research Projects Coordination Unit of Istanbul University-Cerrahpasa (Grant No: 2021–35750).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and design, and/or acquisition of data, and/or analysis and interpretation of data; participated in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The present study was approved by the Medical Research Ethics Committee of Cerrahpasa Medical School (01.14.2021-7774). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration.
Consent to participate
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sulu, C., Senel, G.B., Koca, O. et al. The relations of circulating agouti-related peptide and leptin with altered sleep architecture in patients with active Cushing’s disease: a pilot study. J Endocrinol Invest 47, 167–178 (2024). https://doi.org/10.1007/s40618-023-02133-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02133-0