Abstract
Purpose
The function of B cells in papillary thyroid cancer (PTC) is controversial. The role of B-cell-related tertiary lymphoid structures (TLSs) is still unclear. Whether B cells exert their anti-tumor effect through forming TLS in PTC needs further investigation.
Methods
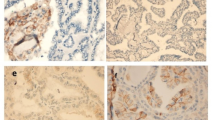
We detected the percentage of B cells in PTC tissues by multi-parameter flow cytometry. Paraffin-embedded tumor tissues of 125 PTC patients were collected and stained with Haematoxylin–Eosin (H&E) for inflammatory infiltration analysis in combination with clinical features. Multiplexed immunohistochemistry (mIHC) was performed to verify the TLSs in above inflammatory infiltration. Correlation of B cells and TLSs with prognosis was analyzed using the TCGA database.
Results
We observed that PTC patients with higher expression of B lineage cell genes had improved survival and the percentage of B cells in the PTC tumor tissues was variable. Moreover, PTC tumor tissues with more B cells were surrounded by immune cell aggregates of varying sizes. We furtherly confirmed the immune cell aggregates as TLSs with different maturation stages. By analyzing PTC data from TCGA database, we found the maturation stages of TLSs were associated with genders and clinical stages among PTC patients. Moreover, patients with high TLSs survived longer and had a better prognosis.
Conclusion
B cells are associated with the existence of TLSs which have different maturation stages in PTC. Both B cells and TLSs are associated with the survival rate of PTC. These observations indicate that the anti-tumor effects of B cells in PTC are associated with TLSs formation.





Similar content being viewed by others
Data availability
Authors declare that the raw data supporting the conclusions of this article will be made available upon request.
References
Cancer Genome Atlas Research Network (2014) Integrated genomic characterization of papillary thyroid carcinoma. Cell 159(3):676–690
Raman P, Koenig RJ (2014) Pax-8-PPAR-γ fusion protein in thyroid carcinoma. Nat Rev Endocrinol 10(10):616–623
Grogan RH et al (2013) A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery 154(6):1436–1447
Haugen BR et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc 26(1):1–133
Cunha LL et al (2012) Infiltration of a mixture of immune cells may be related to good prognosis in patients with differentiated thyroid carcinoma. Clin Endocrinol 77(6):918–925
Bychkov A, Jung CK (2018) Aberrant expression of CD20 in thyroid cancer and its clinicopathologic significance. Hum Pathol 71:74–83
Wang X et al (2019) IL-10-producing B cells in differentiated thyroid cancer suppress the effector function of T cells but improve their survival upon activation. Exp Cell Res 376(2):192–197
Binnewies M et al (2018) Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med 24(5):541–550
Sautès-Fridman C et al (2020) Tertiary lymphoid structures and B cells: clinical impact and therapeutic modulation in cancer. Semin Immunol 48:101406
Siliņa K et al (2018) Germinal centers determine the prognostic relevance of tertiary lymphoid structures and are impaired by corticosteroids in lung squamous cell carcinoma. Can Res 78(5):1308–1320
Calderaro J et al (2019) Intra-tumoral tertiary lymphoid structures are associated with a low risk of early recurrence of hepatocellular carcinoma. J Hepatol 70(1):58–65
Cabrita R et al (2020) Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature 577(7791):561–565
Petitprez F et al (2020) B cells are associated with survival and immunotherapy response in sarcoma. Nature 577(7791):556–560
Helmink BA et al (2020) B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577(7791):549–555
Koti M et al (2017) Tertiary lymphoid structures associate with tumour stage in urothelial bladder cancer. Bladder Cancer (Amsterdam, Netherlands) 3(4):259–267
Noël G et al (2021) Functional Th1-oriented T follicular helper cells that infiltrate human breast cancer promote effective adaptive immunity. J Clin Invest 131(19):e139905
Posch F et al (2018) Maturation of tertiary lymphoid structures and recurrence of stage II and III colorectal cancer. Oncoimmunology 7(2):e1378844
Wang S-S et al (2019) Tumor-infiltrating B cells: their role and application in anti-tumor immunity in lung cancer. Cell Mol Immunol 16(1):6–18
Sarvaria A, Madrigal JA, Saudemont A (2017) B cell regulation in cancer and anti-tumor immunity. Cell Mol Immunol 14(8):662–674
Schwartz M, Zhang Y, Rosenblatt JD (2016) B cell regulation of the anti-tumor response and role in carcinogenesis. J Immunother Cancer 4:40
Li Q et al (2011) Adoptive transfer of tumor reactive B cells confers host T-cell immunity and tumor regression. Clin Cancer Res Off J Am Assoc Cancer Res 17(15):4987–4995
Germain C et al (2014) Presence of B cells in tertiary lymphoid structures is associated with a protective immunity in patients with lung cancer. Am J Respir Crit Care Med 189(7):832–844
Yang Z et al (2021) Diagnostic and prognostic value of tumor-infiltrating B cells in lymph node metastases of papillary thyroid carcinoma. Virchows Arch Int J Pathol 479(5):947–959
Crotty S (2014) T follicular helper cell differentiation, function, and roles in disease. Immunity 41(4):529–542
Cui C et al (2021) Neoantigen-driven B cell and CD4 T follicular helper cell collaboration promotes anti-tumor CD8 T cell responses. Cell 184(25):6101-6118.e13
Overacre-Delgoffe AE et al (2021) Microbiota-specific T follicular helper cells drive tertiary lymphoid structures and anti-tumor immunity against colorectal cancer. Immunity 54(12):2812-2824.e4
Kinoshita T et al (2016) Prognostic value of tumor-infiltrating lymphocytes differs depending on histological type and smoking habit in completely resected non-small-cell lung cancer. Ann Oncol 27(11):2117–2123
Schalper KA et al (2015) Objective measurement and clinical significance of TILs in non-small cell lung cancer. J Natl Cancer Inst 107(3):dju435
Shobab L, Burman KD, Wartofsky L (2022) Sex Differences in differentiated thyroid cancer. Thyroid 32(3):224–235
Cunha LL, Ward LS (2022) Translating the immune microenvironment of thyroid cancer into clinical practice. Endocr Relat Cancer 29(6):R67-r83
Haupt S et al (2021) Sex disparities matter in cancer development and therapy. Nat Rev Cancer 21(6):393–407
Zahedi A et al (2020) Risk for thyroid cancer recurrence is higher in men than in women independent of disease stage at presentation. Thyroid Off J Am Thyroid Assoc 30(6):871–877
de Carvalho AY et al (2021) Predictive factors for recurrence of papillary thyroid carcinoma: analysis of 4,085 patients. Acta Otorhinolaryngol Ital Organo Ufficiale Della Societa Italiana Di Otorinolaringologia E Chirurgia Cervico-facciale 41(3):236–242
Bortz MD et al (2021) Extrathyroidal extension predicts negative clinical outcomes in papillary thyroid cancer. Surgery 169(1):2–6
Mao J et al (2020) Risk factors for lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis. Front Endocrinol 11:265
Pitzalis C et al (2014) Ectopic lymphoid-like structures in infection, cancer and autoimmunity. Nat Rev Immunol 14(7):447–462
van Dijk N et al (2020) Preoperative ipilimumab plus nivolumab in locoregionally advanced urothelial cancer: the NABUCCO trial. Nat Med 26(12):1839–1844
Lynch KT et al (2021) Heterogeneity in tertiary lymphoid structure B-cells correlates with patient survival in metastatic melanoma. J Immunother Cancer 9(6):e002273
Gao J et al (2020) Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma. Nat Med 26(12):1845–1851
Dieu-Nosjean M-C et al (2016) Tertiary lymphoid structures, drivers of the anti-tumor responses in human cancers. Immunol Rev 271(1):260–275
Ruffin AT et al (2021) B cell signatures and tertiary lymphoid structures contribute to outcome in head and neck squamous cell carcinoma. Nat Commun 12(1):3349
Meylan M et al (2022) Tertiary lymphoid structures generate and propagate anti-tumor antibody-producing plasma cells in renal cell cancer. Immunity 55(3):527-541.e5
Ding G-Y et al (2022) Distribution and density of tertiary lymphoid structures predict clinical outcome in intrahepatic cholangiocarcinoma. J Hepatol 76(3):608–618
Gu-Trantien C et al (2013) CD4+ follicular helper T cell infiltration predicts breast cancer survival. J Clin Investig 123(7):2873–2892
Thommen DS et al (2018) A transcriptionally and functionally distinct PD-1 CD8 T cell pool with predictive potential in non-small-cell lung cancer treated with PD-1 blockade. Nat Med 24(7):994–1004
Figenschau SL et al (2015) Tertiary lymphoid structures are associated with higher tumor grade in primary operable breast cancer patients. BMC Cancer 15:101
Funding
This work was supported by the Guangzhou Science and Technology Plan Project (202102080170 to B.X.), Project of Guangzhou Science and Technology Bureau (2023A03J0967 and 2023A03J0477), and the Program for Guangdong Introducing Innovative and Entrepreneurial Teams (2017ZT07S054).
Author information
Authors and Affiliations
Contributions
Y-YL, S-JL and ZC: performed the experiments. Y-YL and S-JL: analyzed the data and plotted tables. FS: collected samples. M-CL: checked the data. LL, Q-ZL, BX and Z-XL: designed the work. BX: provided the funding of the project. YYL: wrote the manuscript. M-CL, LL, Q-ZL, BX and Z-XL: revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This study was approved by the Medical Ethics Committee of the Second Affiliated Hospital of South China University of Technology (K-2019-185). Written informed consent was obtained from all patients.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, YY., Li, SJ., Liu, MC. et al. B cells and tertiary lymphoid structures are associated with survival in papillary thyroid cancer. J Endocrinol Invest 46, 2247–2256 (2023). https://doi.org/10.1007/s40618-023-02072-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02072-w