Abstract
Purpose
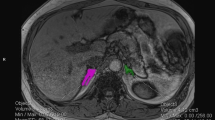
The role of computed tomography (CT) in the diagnosis of primary aldosteronism (PA) warrants attention, since the success application of adrenal venous sampling (AVS) remains limited. We aimed to investigate the value of CT-based volumetric indicators, including left-versus-right-adrenal-volume ratio (L/Rv) and left-subtract-right-adrenal-volume difference (L − Rv), in the diagnosis of unilateral primary aldosteronism (UPA).
Methods
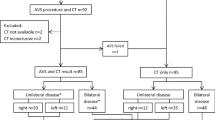
A retrospective case–control study included 153 patients with PA and 1272 controls. AVS was used to classify patients into bilateral disease, left-sided disease, and right-sided disease groups.
Results
Adrenal gland volume on both sides of PA patients was significantly larger than controls. The optimal cutoff values of L/Rv and L − Rv were 1.417 [area under the curve (AUC) 0.864] and 1.185 (AUC 0.827), respectively, for the diagnosis of left-sided PA, and 1.030 (AUC 0.767) and 0.220 (AUC 0.769), respectively, for the diagnosis of right-sided PA. The mean AUC for subsequent cross-validation ranged from 0.77 ± 0.03 to 0.86 ± 0.02. Based on the optimal cutoff values, the combination of L/Rv and L − Rv detected 69.6% of patients with left-sided PA and 74.3% of patients with right-sided PA, with a specificity of 93.5% and 89.0%, respectively. For a better clinical application, we reported the sub-optimal cutoffs corresponding to a specificity of 95%. A L/Rv higher than 1.431 and a L − Rv higher than 3.185 as sub-optimal cutoff values was detected in 26.1% of patients with left-sided PA (specificity: 97.2%). A L/Rv smaller than 0.892 and a L − Rv smaller than −0.640 could detect 48.6% of patients with right-sided PA (specificity: 97.5%).
Conclusions
CT-based L/Rv and L − Rv performed well in predicting UPA. The combination of L/Rv and L − Rv may serve as a potential indicator for guiding surgical decision making in centers without AVS programs.


Similar content being viewed by others
Availability of data and materials
Data are available upon motivated requests.
References
Käyser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, Hermus AR, Lenders JW, Deinum J (2016) Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab 101:2826–2835. https://doi.org/10.1210/jc.2016-1472
Mulatero P, Monticone S, Deinum J, Amar L, Prejbisz A, Zennaro M-C, Beuschlein F, Rossi GP, Nishikawa T, Morganti A et al (2020) Genetics, prevalence, screening and confirmation of primary aldosteronism: a position statement and consensus of the working group on endocrine hypertension of the European society of hypertension. J Hypertens 38:1919–1928. https://doi.org/10.1097/HJH.0000000000002510
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, Mulatero P (2018) Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 6:41–50. https://doi.org/10.1016/S2213-8587(17)30319-4
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, Stowasser M, Young WF (2016) The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101:1889–1916. https://doi.org/10.1210/jc.2015-4061
Monticone S, Viola A, Rossato D, Veglio F, Reincke M, Gomez-Sanchez C, Mulatero P (2015) Adrenal vein sampling in primary aldosteronism: towards a standardised protocol. Lancet Diabetes Endocrinol 3:296–303. https://doi.org/10.1016/S2213-8587(14)70069-5
Buffolo F, Monticone S, Williams TA, Rossato D, Burrello J, Tetti M, Veglio F, Mulatero P (2017) Subtype diagnosis of primary aldosteronism: is adrenal vein sampling always necessary? Int J Mol Sci. https://doi.org/10.3390/ijms18040848
Pasternak JD, Epelboym I, Seiser N, Wingo M, Herman M, Cowan V, Gosnell JE, Shen WT, Kerlan RK Jr, Lee JA et al (2016) Diagnostic utility of data from adrenal venous sampling for primary aldosteronism despite failed cannulation of the right adrenal vein. Surgery 159:267–273. https://doi.org/10.1016/j.surg.2015.06.048
Strajina V, Al-Hilli Z, Andrews JC, Bancos I, Thompson GB, Farley DR, Lyden ML, Dy BM, Young WF, McKenzie TJ (2018) Primary aldosteronism: making sense of partial data sets from failed adrenal venous sampling-suppression of adrenal aldosterone production can be used in clinical decision making. Surgery 163:801–806. https://doi.org/10.1016/j.surg.2017.10.012
Parasiliti-Caprino M, Bioletto F, Ceccato F, Lopez C, Bollati M, Di Carlo MC, Voltan G, Rossato D, Giraudo G, Scaroni C et al (2022) The accuracy of simple and adjusted aldosterone indices for assessing selectivity and lateralization of adrenal vein sampling in the diagnosis of primary aldosteronism subtypes. Front Endocrinol (Lausanne) 13:801529. https://doi.org/10.3389/fendo.2022.801529
Parasiliti-Caprino M, Bioletto F, Ceccato F, Lopez C, Bollati M, Voltan G, Rossato D, Giraudo G, Scaroni C, Ghigo E et al (2021) The diagnostic accuracy of adjusted unconventional indices for adrenal vein sampling in the diagnosis of primary aldosteronism subtypes. J Hypertens 39:1025–1033. https://doi.org/10.1097/HJH.0000000000002700
Burrello J, Burrello A, Pieroni J, Sconfienza E, Forestiero V, Amongero M, Rossato D, Veglio F, Williams TA, Monticone S et al (2020) Prediction of hyperaldosteronism subtypes when adrenal vein sampling is unilaterally successful. Eur J Endocrinol 183:657–667. https://doi.org/10.1530/EJE-20-0656
Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, Ichijo T, Wada N, Yoshimoto T, Ogawa Y et al (2018) Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab 103:900–908. https://doi.org/10.1210/jc.2017-01774
Kobayashi H, Abe M, Soma M, Takeda Y, Kurihara I, Itoh H, Umakoshi H, Tsuiki M, Katabami T, Ichijo T et al (2018) Development and validation of subtype prediction scores for the workup of primary aldosteronism. J Hypertens 36:2269–2276. https://doi.org/10.1097/HJH.0000000000001855
Kamemura K, Wada N, Ichijo T, Matsuda Y, Fujii Y, Kai T, Fukuoka T, Sakamoto R, Ogo A, Suzuki T et al (2017) Significance of adrenal computed tomography in predicting laterality and indicating adrenal vein sampling in primary aldosteronism. J Hum Hypertens 31:195–199. https://doi.org/10.1038/jhh.2016.61
Riester A, Fischer E, Degenhart C, Reiser MF, Bidlingmaier M, Beuschlein F, Reincke M, Quinkler M (2014) Age below 40 or a recently proposed clinical prediction score cannot bypass adrenal venous sampling in primary aldosteronism. J Clin Endocrinol Metab 99:E1035–E1039. https://doi.org/10.1210/jc.2013-3789
Burrello J, Burrello A, Pieroni J, Sconfienza E, Forestiero V, Rabbia P, Adolf C, Reincke M, Veglio F, Williams TA et al (2020) Development and validation of prediction models for subtype diagnosis of patients with primary aldosteronism. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgaa379
Carsin-Vu A, Oubaya N, Mulé S, Janvier A, Delemer B, Soyer P, Hoeffel C (2016) MDCT linear and volumetric analysis of adrenal glands: normative data and multiparametric assessment. Eur Radiol 26:2494–2501. https://doi.org/10.1007/s00330-015-4063-y
Wang X, Jin Z-Y, Xue H-D, Liu W, Sun H, Chen Y, Xu K (2013) Evaluation of normal adrenal gland volume by 64-slice CT. Chin Med Sci J 27:220–224
Degenhart C, Schneller J, Osswald A, Pallauf A, Riester A, Reiser MF, Reincke M, Beuschlein F (2017) Volumetric and densitometric evaluation of the adrenal glands in patients with primary aldosteronism. Clin Endocrinol (Oxf) 86:325–331. https://doi.org/10.1111/cen.13258
Velema MS, Canu L, Dekkers T, Hermus A, Timmers H, Schultze Kool LJ, Groenewoud H, Jacobs C, Deinum J, Investigators S (2021) Volumetric evaluation of CT images of adrenal glands in primary aldosteronism. J Endocrinol Invest 44:2359–2366. https://doi.org/10.1007/s40618-021-01540-5
Tang YZ, Bharwani N, Micco M, Akker S, Rockall AG, Sahdev A (2014) The prevalence of incidentally detected adrenal enlargement on CT. Clin Radiol 69:e37–e42. https://doi.org/10.1016/j.crad.2013.08.017
Arnaldi G, Angeli A, Atkinson AB, Bertagna X, Cavagnini F, Chrousos GP, Fava GA, Findling JW, Gaillard RC, Grossman AB et al (2003) Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab 88:5593–5602. https://doi.org/10.1210/jc.2003-030871
Inoue K, Kitamoto T, Tsurutani Y, Saito J, Omura M, Nishikawa T (2021) Cortisol co-secretion and clinical usefulness of acth stimulation test in primary aldosteronism: a systematic review and biases in epidemiological studies. Front Endocrinol (Lausanne) 12:645488. https://doi.org/10.3389/fendo.2021.645488
Chen C, Lu FC, and Department of Disease Control Ministry of Health PRC (2004) The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci 17(Suppl):1–36
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, Satoh F, Amar L, Quinkler M, Deinum J et al (2017) Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol 5:689–699. https://doi.org/10.1016/S2213-8587(17)30135-3
Dekkers T, Prejbisz A, Kool LJS, Groenewoud H, Velema M, Spiering W, Kołodziejczyk-Kruk S, Arntz M, Kądziela J, Langenhuijsen JF et al (2016) Adrenal vein sampling versus CT scan to determine treatment in primary aldosteronism: an outcome-based randomised diagnostic trial. Lancet Diabetes Endocrinol 4:739–746. https://doi.org/10.1016/s2213-8587(16)30100-0
Serifoglu I, Oz II, Bilici M (2016) The adrenal gland volume measurements in manifestation of the metabolic status in type-2 diabetes mellitus patients. Int J Endocrinol 2016:7195849. https://doi.org/10.1155/2016/7195849
Schneller J, Reiser M, Beuschlein F, Osswald A, Pallauf A, Riester A, Tietze JK, Reincke M, Degenhart C (2014) Linear and volumetric evaluation of the adrenal gland–MDCT-based measurements of the adrenals. Acad Radiol 21:1465–1474. https://doi.org/10.1016/j.acra.2014.06.008
Liu F, Chen Y, Xie W, Liu C, Zhu Y, Tian H, Ren Y, Chen T (2020) Obesity might persistently increase adrenal gland volume: a preliminary study. Obes Surg 30:3503–3507. https://doi.org/10.1007/s11695-020-04593-2
Geraghty EM, Boone JM, McGahan JP, Jain K (2004) Normal organ volume assessment from abdominal CT. Abdom Imaging 29:482–490
Rubin RT, Phillips JJ (1991) Adrenal gland volume determination by computed tomography and magnetic resonance imaging in normal subjects. Invest Radiol 26:465–469
Boulkroun S, Samson-Couterie B, Dzib J-FG, Lefebvre H, Louiset E, Amar L, Plouin P-F, Lalli E, Jeunemaitre X, Benecke A et al (2010) Adrenal cortex remodeling and functional zona glomerulosa hyperplasia in primary aldosteronism. Hypertension 56:885–892. https://doi.org/10.1161/HYPERTENSIONAHA.110.158543
Li S, Sun H, Ma L, Zhu Y, Xie W, Sun J, Zhao L, Qing B, Ren Y, Tian H et al (2020) Left-versus-right-adrenal-volume ratio as a screening index before adrenal venous sampling to identify unilateral primary aldosteronism patients. J Hypertens 38:347–353. https://doi.org/10.1097/HJH.0000000000002271
Lim V, Guo Q, Grant CS, Thompson GB, Richards ML, Farley DR, Young WF (2014) Accuracy of adrenal imaging and adrenal venous sampling in predicting surgical cure of primary aldosteronism. J Clin Endocrinol Metab 99:2712–2719. https://doi.org/10.1210/jc.2013-4146
Ladurner R, Sommerey S, Buechner S, Dietz A, Degenhart C, Hallfeldt K, Gallwas J (2017) Accuracy of adrenal imaging and adrenal venous sampling in diagnosing unilateral primary aldosteronism. Eur J Clin Invest 47:372–377. https://doi.org/10.1111/eci.12746
Zhou Y, Wang D, Jiang L, Ran F, Chen S, Zhou P, Wang P (2020) Diagnostic accuracy of adrenal imaging for subtype diagnosis in primary aldosteronism: systematic review and meta-analysis. BMJ Open 10:e038489. https://doi.org/10.1136/bmjopen-2020-038489
Acknowledgements
The authors gratefully acknowledge the participation of all patients and the grant of the National Nature Science Foundation of China.
Funding
This study was supported by the National Nature Science Foundation of China under Grant (number 81770812 and 81974110).
Author information
Authors and Affiliations
Contributions
G-JQ, WZ, JW and M-WS were involved in the development and implementation of the study design and methods and drafting of the paper, revising it critically for intellectual content. All the authors were involved with manuscript preparation, multiple draft revisions, conception of tables, analysis and interpretation of the data and have reviewed and approved the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All the procedures involving human participants were performed in accordance with the ethical standard of the Institutional Ethics Committee with which the studies were conducted. This paper does not contain any studies with animals performed by any of the authors.
Informed consent
The Ethics Committee judged that written informed consent for participation was not required given the non-intrusive and non-experimental character of this study in accordance with the national legislation and the institutional requirements.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, W., Wang, J., Shao, M. et al. The performance of left/right adrenal volume ratio and volume difference in predicting unilateral primary aldosteronism. J Endocrinol Invest 46, 687–698 (2023). https://doi.org/10.1007/s40618-022-01912-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01912-5