Abstract
Aim
The aim was to assess perceived psychological stress, emotional state, and quality of life (QoL) in men and women with congenital adrenal hyperplasia (CAH) in comparison to age- and sex-matched control individuals.
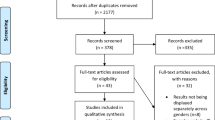
Methods
Participants: 26 patients with CAH (11 men, 15 women, age 14–48 years) and 26 age- and sex-matched control individuals without CAH. Psychological assessment: Perceived Stress Scale, Profile of Mood States2, and WHO Brief Quality of Life Questionnaire.
Results
There were no significant differences in perceived stress, emotional state and QoL scores between men with CAH and control men. Perceived distress (median 14.0 score vs. 10.0 score, p = 0.020), tension-anxiety (median 9.0 score vs. 3.5 score, p = 0.026), depression-dejection (median 12.0 score vs. 5.0 score, p = 0.040), fatigue-inertia (median 13.0 score vs. 7.5 score, p = 0.007) were higher and environmental domain of QoL (median 16.0 score vs. 17.0 score, p = 0.001) was lower in women with CAH than in control women.
Conclusion
Women with congenital adrenal hyperplasia have higher perceived distress, tension-anxiety, depression dejection, fatigue-inertia, and worse environmental aspect of quality of life than age-matched control women, while perceived psychological stress, emotional state and quality of life in men with congenital adrenal hyperplasia do not differ from that of age-matched control men.
Similar content being viewed by others
References
Pignatelli D, Carvalho BL, Palmeiro A, Barros A, Guerreiro SG, Macut D (2019) The complexities in genotyping of congenital adrenal hyperplasia: 21-hydroxylase deficiency. Front Endocrinol 10:432. https://doi.org/10.3389/fendo.2019.00432.79
Claahsen-van der Grinten HL, Speiser PW, Ahmed SF, Arlt W, Auchus RJ, Falhammar H, Flück CE, Guasti L, Huebner A, Kortmann BBM et al (2021) Congenital adrenal hyperplasia—current insights in pathophysiology, diagnostics and management. Endocr Re 7:16
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American college of medical genetics and genomics and the association for molecular pathology. Genet Med 17:405–423
Navardauskaitė R, Banevičiūtė K, Songailienė J, Grigalionienė K, Čereškevičius D, Šukys M, Mockevicienė G, Smirnova M, Utkus A, Verkauskienė R (2021) Impact of newborn screening on clinical presentation of congenital adrenal hyperplasia. Medicina 57(10):1035. https://doi.org/10.3390/medicina57101035
Nordenström A, Falhammar H (2019) Diagnosis and management of the patient with non-classic CAH due to 21-hydroxylase deficiency. Eur J Endocrinol 180:R127–R145
Zainuddin AA, Grover SR, Shamsuddin K, Mahdy ZA (2013) Research on quality of life in female patients with congenital adrenal hyperplasia and issues in developing nations. J Pediatr Adolesc Gynecol 26:296–304
Carroll L, Graff C, Wicks M, Thomas AD (2020) Living with an invisible illness: a qualitative study exploring the lived experiences of female children with congenital adrenal hyperplasia. Qual Life Res 29:673–681
Strandqvist A, Falhammar H, Lichtenstein P, Hirschberg AL, Wedell A, Norrby C, Nordenskjöld A, Frisén L, Nordenström A (2014) Suboptimal psychosocial outcomes in patients with congenital adrenal hyperplasia: epidemiological studies in a nonbiased national cohort in Sweden. J Clin Endocrinol Metab 99(4):1425–1432
Cull M (2005) Commentary: a support group’s perspective. BMJ 330:341
Morgan JF, Murphy H, Lacey JH, Conway G (2005) Long term psychological outcome for women with congenital adrenal hyperplasia: cross-sectional survey. British Med J 330:340–341
Reisch N, Hahner S, Bleicken B, Flade L, Pedrosa Gil F, Loefflet M, Ventz M, Hinz A, Beuschlein F, Alloli B et al (2011) Quality of life is less impaired in adults with congenital adrenal hyperplasia because of 21-hydroxylase deficiency than in patients with primary adrenal insufficiency. Clin Endocrinol 74:166–173
Han TS, Conway GS, Willis DS, Krone N, Rees DA, Stimson RH, Arlt W, Walker BR, Ross RJ (2014) United Kingdom congenital adrenal hyperplasia adult study executive (CaHASE): relationship between adult height and health outcomes in adults with congenital adrenal hyperplasia: United Kingdom congenital adrenal hyperplasia adult study executive (CaHASE). J Clin Endocrinol Metab 99:E1547–E1555
Nermoen I, Husebye ES, Svartberg J, Løvås K (2010) Subjective health status in men and women with congenital adrenal hyperplasia: a population-based survey in Norway. European J Endocrinol 163:453–459
Frisen L, Nordenstorm A, Falhammar H, Filipsson H, Holmdahl G, Janson PO, Thoren M, Hagenfeldt K, Moller A, Nordenskjold A (2009) Gender role behavior, sexuality, and psychosocial adaptation in women with congenital adrenal hyperplasia due to CYP21A2 deficiency. J Clin Endocrinol Metab 94:3432–3439
Verhees MJM, Engels M, Span PN, Sweep FCG, van Herwaarden AE, Falhammar H, Nordenström A et al (2021) Quality of life in men with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Front Endocrinol 12:626646
Berenbaum SA (2018) Beyond pink and blue: the complexity of early androgen effects on gender development. Child Dev Perspect 12(1):58–64
World Health Organization (1989) United Nations Population Fund, UNICEF, The reproductive health of adolescents: a strategy for action: a joint WHO/UNFPA/ UNICEF Statement. World Health Organization, Geneva, pp 1–18
Piaget J (1962) The stages of the intellectual development of the child. Bull Menninger Clin 26:120–128
Kivnick HQ, Wells CK (2014) Untapped richness in Erik H. Erikson‘s rootstock. Gerontologist 54(1):40–50
Speiser PW, Arlt W, Auchus RJ, Baskin LS, Conway GS, Merke DP, Meyer-Bahlburg HFL, Miller WL, Murad MH, Oberfield SE, White PC (2018) Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 103(11):4043–4088. https://doi.org/10.1210/jc.2018-01865
WHO (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organization, Geneva, pp 1–36 (WHO technical report series, No. 854)
Garrow JS, Webster J (1985) Quetelet’s index (W/H2) as a measure of fatness. Int J Obes 9:147–153
Tutkuviene J (1995) Evaluation of growth and puberty of children (in Lithuanian). Meralas, Vilnius
Schneiderman N, Ironson G, Siegel SD (2005) Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol 1:607–628
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Answer S, Manzar MD, Alghadir AH, Salahuddin M, Hameed UA (2020) Psychometric analysis of the perceived stress scale among healthy university students. Neuropsychiatr Dis Treat 16:2389–2396
Golden-Kreutz DM, Browne MW, Frierson GM, Andersen BL (2004) Assessing stress in cancer patients: a second-order factor analysis model for the perceived stress scale. Assessment 11(3):216–223
Heuchert JP, McNair DM (2012) Profile of Mood States, 2nd ed POMS2. North Tonawanda, Multi Health System
WHO (1996) WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment. World Health Organization, Field Trail Version.
Schützmann K, Brinkmann L, Schacht M, Richter-Appelt H (2009) Psychological distress, self-harminh behavior, and suicidal tendencies in adults with disorders of sex development. Arch Sex Behav 38:16–33
Oner O, Aycan Z, Tiryaki T, Soy D, Cetinkaya E, Kibar E (2009) Variables related to behavioral and emotional problems and gender typed behaviors in female patients with congenital adrenal hyperplasia. J Pediatr Endocrinol Metab 22(2):143–151
Hamed SA, Attiah FA, Elaal RFA, Fawzy M (2021) Behavioral assessment of females with congenital adrenal hyperplasia. Hormones 20:131–141
Engberg H, Butwicka A, Nordenström A, Hirschberg AL, Falhammar H, Lichtenstein P, Frisén L, Landen M (2015) Congenital adrenal hyperplasia and risk for psychiatric disorders in girls and women born between 1915 and 2010: a total population study. Psychoneuroendocrinology 60:195–205
Daae E, Feragen KB, Nermoen I, Falhmmar H (2018) Psychological adjustment, quality of life, and self-perceptions of reproductive health in males with congenital adrenal hyperplasia: a systematic review. Endocrine 62:3–13
de Vries ALC, Roehle R, Marshall L, Frisén L, van de Grift TC, Kreukels BPC, Bouvattier C, Köhler B, Thyen U, Nordenström A, Rapp M, Cohen-Kettenis PT (2019) Mental health of a large group of adults with disorders of sex development in six European countries. Psychosomatic Med 81:629–640
Mueller SC, Ng P, Sinaii N, Leschek EW, Green-Golan L, VanRyzin C, Ernst M, Merke DP (2010) Psychiatric characterization of children with genetic causes of hyperandrogenism. Eur J Endocrinol 163(5):801–810
Berenbaum SA, Duck SC, Bryk K (2000) Behavioral effects of prenatal versus postnatal androgen excess in children with 21-hydroxylase-deficient congenital adrenal hyperplasia. J Clin Endocrinol Metab 2:727–733
Warrington TP, Bostwick JM (2006) Psychiatric adverse effect of corticosteroids. Mayo Clin Proc 81(10):1361–1367
Ernst M, Maheu FS, Schroth E, Hardin J, Golan LG, Cameron J, Allen R, Holzer S, Nelson E, Pine DS, Merke DP (2007) Amygdala function in adolescents with congenital adrenal hyperplasia: a model for the study of early steroid abnormalities. Neuropsychologia 45(9):2104–2113
Nicolaides NC, Lamprokostopoulou KE, A, Chrousos GP, Charmandari EM, (2015) Stress, the stress system and the role of glucocorticoids. Neuriimmunomodulation 22:6–19
Giebels V, Repping-Wuts H, Bleijenberg G, Kroese JM, Stikkelbroeck N, Hermus A (2014) Severe fatigue in patients with adrenal insufficiency: physical, psychosocial and endocrine determinants. J Endocrinol Invest 37:293–301
Zainuddin AA, Grover SR, Ghani NAA, Wu LL, Rasat R, Manaf MRA, Shamsuddin K, Mahdy ZA (2020) Health- related quality of life of female patients with congenital adrenal hyperplasia in Malaysia. Health Qual Life Outcomes 18:258
Bachelot A, Vialon M, Baptiste A, Tejedor I, Elie C, Polak M, Touraine P, The CRMERC study group (2017) Impact of transition on quality of life in patients with congenital adrenal hyperplasia diagnosed during childhood. Endocr Connect 6:422–429
Arlt W, Willis DS, Wild SH, Krone N, Doherty EJ, Hahner S, Han TS, Carroll PV, Conway GS, Rees DA, Stimson RH, Walker BR, Connell JM, Ross RJ (2010) Health status of adults with congenital adrenal hyperplasia: a cohort study of 203 patients. J Clin Endocrinol Metab 95(11):5110–5121
Falhammar H, Nystrom NF, Thoren M (2014) Quality of life, social situation, and sexual satisfaction in adult males with congenital adrenal hyperplasia. Endocrine 47(1):299–307
Statistic Department of Lithuania, Portal of the Official Statistics https://osp.stat.gov.lt. (2021) Accessed date: 04 October 2021.
Stikkelbroeck NMML, Oyen WJG, van der Wilt G-J, Hermus ARMM, Otten BJ (2003) Normal bone mineral density and lean body mass, but increased fat mass, in young adult patients with congenital adrenal hyperplasia. J Clin Endocrinol Metab 88(3):1036–1042
Aycan Z, Akbuğa S, Cetinkaya E, Ocal G, Berberoğlu M, Evliyaoğlu O, Adiyaman P (2009) Final height of patients with classical congenital adrenal hyperplasia. Turk J Pediatr 15(6):539–544
Alzanbagi MA, Milyani AA, Al-Agha E (2018) Growth characteristics in children with congenital adrenal hyperplasia. Saudi Med J 39(7):674–678
Falhammar H, Frisén L, Hirschberg AL, Norrby C, Almqvist C, Nordenskjöld A, Nordenström A (2015) Increased cardiovascular and metabolic morbidity in patients with 21-hydroxylase deficiency: a Swedish population-based national cohort study. J Clin Endocrinol Metab 100(9):3520–3528
Kim MS, Ryabets-Lienhard A, Dao-Tran A, Mittelman SD, Gilsanz V, Schrager SM, Geffner ME (2015) Increased abdominal adiposity in adolescents and young adults with classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 100(8):E1153–E1159
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-of-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interests. The research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
The study was approved by Kaunas Regional Ethics Committee of Biomedical Research (No BE-2-29). For the participants aged below18 years the written consent of their parents or caregivers were obtained as well. As the study involved human participants, the investigation was carried out in accordance with the Declaration of Helsinki.
Informed consent
All procedures were carried out with the adequate understanding and written consent of the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lašaitė, L., Navardauskaitė, R., Semėnienė, K. et al. Psychological stress, emotions, and quality of life in men and women with congenital adrenal hyperplasia. J Endocrinol Invest 45, 1925–1934 (2022). https://doi.org/10.1007/s40618-022-01824-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01824-4