Abstract
Purpose
Impaired activity of the peptidylprolyl cis/trans isomerase NIMA-interacting 1 (PIN1) isomerase might contribute to link disturbed glucose metabolism and risk of glucose related neurotoxicity, neurodegeneration and cognitive decline. The isomerase modulates also pathways of peripheral insulin sensitivity and secretion.
We aimed at investigating the levels of circulating PIN1 in adolescents with obesity and any association with their glucose metabolism.
Methods
We enrolled 145 adolescents (age 12–17.8 years); 67 lean controls (46.2%) and 78 (53.8%) with overweight or obesity (males n = 62, 46%). We estimated glucose and insulin in fasting condition and after a standard oral glucose tolerance test; fasting serum levels of PIN1, amyloid β-protein 42 (Aβ42), presenilin 1 (PSEN1), glucagon-like peptide 1 (GLP1) and Non Esterified Fatty Acids (NEFA). We calculated the homeostasis model assessment of insulin resistance (HOMA-IR), the β cell function (HOMA-β) and the Adipo-IR.
Results
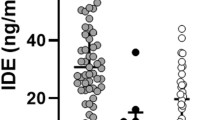
There was no difference in PIN1 serum levels between normal weight individuals and patients with obesity. However, there was an inverse correlation between serum fasting PIN1 and glucose (r − 0.183 and p = 0.027). We confirmed levels of Aβ42 and PSEN1 were higher in teens with obesity than in lean controls and their correlation with the body mass index (Aβ42: r = 0.302, p = 0.0001, PSEN1 r = 0.231, p = 0.005) and the HOMA-IR (Aβ42: r = 0.219, p = 0.009, r = 0.170, p < 0.042).
Conclusions
There was no significant rise of circulating PIN1 levels in young individuals with obesity. Increased levels reported in the literature in adult patients are likely to occur late in the natural history of the disease with the onset of an overt impairment of glucose homeostasis.
Graphical abstract


Similar content being viewed by others
Availability of data and materials
The data set generated and analyzed during the current study is not publicly available for reasons related to privacy and participants’ consent but is available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Alzheimer disease
- Aβ42:
-
Amyloid β-protein 42
- Akt:
-
Protein-chinasi B
- AMPK:
-
AMP-activated protein kinase
- APP:
-
Amyloid precursor protein
- AUC0–120 :
-
Areas under the glucose and insulin curves
- βPin1 KO:
-
β Cell-specific Pin1 KO
- BMI:
-
Body mass index
- CRE:
-
CAMP-responsive element
- CRTC2:
-
Cyclic AMP-response element-binding protein-regulated transcription coactivator 2
- GLP1:
-
GLP1 glucagon-like peptide 1
- GSK-3β:
-
Glycogen synthase kinase-3β
- HOMA-β:
-
β Cell function
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- IR:
-
Insulin resistance
- IRS-1:
-
Insulin receptor substrate 1
- NEFA:
-
Non esterified fatty acids
- OGTT:
-
Standard glucose oral tolerance test
- PI3K:
-
PhosphatidylInositol 3-kinase
- PIN1:
-
Peptidylprolyl cis/trans isomerase NIMA-interacting 1
- PSEN1:
-
Presenilin 1
- ROS:
-
Reactive oxygen species
- SD:
-
Standard deviation
- SDS:
-
Standard deviation score
- SIK2:
-
Salt-inducible kinase 2
- T2D:
-
Type 2 diabetes
References
Brufani C, Tura A, Bedogni G, Luciano R, Sbrignadello S, Fintini D, Cappa M, Weiss R, Manco M (2017) Inside out the ragbag of glucose intolerance in obese adolescents. Horm Res Paediatr 87(5):287–294. https://doi.org/10.1159/000464144
Bianchi M, D’Oria V, Braghini MR, Petrini S, Manco M (2019) Liraglutide treatment ameliorates neurotoxicity induced by stable silencing of Pin1. Int J Mol Sci 20(20):5064. https://doi.org/10.3390/ijms20205064
Bianchi M, Manco M (2018) Pin1 modulation in physiological status and neurodegeneration. Any contribution to the pathogenesis of type 3 diabetes? Int J Mol Sci 19(8):2319. https://doi.org/10.3390/ijms19082319
Lu KP, Zhou XZ (2007) The prolyl isomerase PIN1: a pivotal new twist in phosphorylation signalling and disease. Nat Rev Mol Cell Biol 8(11):904–916. https://doi.org/10.1038/nrm2261
Nakatsu Y, Matsunaga Y, Yamamotoya T, Ueda K, Inoue Y, Mori K, Sakoda H, Fujishiro M, Ono H, Kushiyama A, Asano T (2016) Physiological and pathogenic roles of prolyl isomerase Pin1 in metabolic regulations via multiple signal transduction pathway modulations. Int J Mol Sci 17(9):1495. https://doi.org/10.3390/ijms17091495
Nakatsu Y, Sakoda H, Kushiyama A, Zhang J, Ono H, Fujishiro M, Kikuchi T, Fukushima T, Yoneda M, Ohno H, Horike N, Kanna M, Tsuchiya Y, Kamata H, Nishimura F, Isobe T, Ogihara T, Katagiri H, Oka Y, Takahashi S, Kurihara H, Uchida T, Asano T (2011) Peptidyl-prolyl cis/trans isomerase NIMA-interacting 1 associates with insulin receptor substrate-1 and enhances insulin actions and adipogenesis. J Boil Chem 286(23):20812–22. https://doi.org/10.1074/jbc.M110.206904
Ma SL, Pastorino L, Zhou XZ, Lu KP (2012) Prolyl isomerase Pin1 promotes amyloid precursor protein (APP) turnover by inhibiting glycogen synthase kinase-3beta (GSK3beta) activity: novel mechanism for Pin1 to protect against Alzheimer disease. J Biol Chem 287(10):6969–6973. https://doi.org/10.1074/jbc.C111.298596
Liao Y, Hung MC (2010) Physiological regulation of Akt activity and stability. Am J Transl Res 2(1):19–42
Nikoulina SE, Ciaraldi TP, Carter L, Mudaliar S, Park KS, Henry RR (2001) Impaired muscle glycogen synthase in type 2 diabetes is associated with diminished phosphatidylinositol 3-kinase activation. J Clin Endocrinol Metab 86(9):4307–4314. https://doi.org/10.1210/jcem.86.9.7872
Nakatsu Y, Mori K, Matsunaga Y, Yamamotoya T, Ueda K, Inoue Y, Mitsuzaki-Miyoshi K, Sakoda H, Fujishiro M, Yamaguchi S, Kushiyama A, Ono H, Ishihara H, Asano T (2017) The prolyl isomerase Pin1 increases beta-cell proliferation and enhances insulin secretion. J Biol Chem 292(28):11886–11895. https://doi.org/10.1074/jbc.M117.780726
Paneni F, Costantino S, Castello L, Battista R, Capretti G, Chiandotto S, D’Amario D, Scavone G, Villano A, Rustighi A, Crea F, Pitocco D, Lanza G, Volpe M, Del Sal G, Luscher TF, Cosentino F (2015) Targeting prolyl-isomerase Pin1 prevents mitochondrial oxidative stress and vascular dysfunction: insights in patients with diabetes. Eur Heart J 36(13):817–828. https://doi.org/10.1093/eurheartj/ehu179
Driver JA, Zhou XZ, Lu KP (2014) Regulation of protein conformation by Pin1 offers novel disease mechanisms and therapeutic approaches in Alzheimer’s disease. Discov Med 17(92):93–99
Pastorino L, Sun A, Lu PJ, Zhou XZ, Balastik M, Finn G, Wulf G, Lim J, Li SH, Li X, Xia W, Nicholson LK, Lu KP (2006) The prolyl isomerase Pin1 regulates amyloid precursor protein processing and amyloid-beta production. Nature 440(7083):528–34. https://doi.org/10.1038/nature04543
Luciano R, Barraco GM, Muraca M, Ottino S, Spreghini MR, Sforza RW, Rustico C, Morino GS, Manco M (2015) Biomarkers of Alzheimer disease, insulin resistance, and obesity in childhood. Pediatrics 135(6):1074–81. https://doi.org/10.1542/peds.2014-2391
Balkhiyarova Z, Luciano R, Kaakinen M, Ulrich A, Shmeliov A, Bianchi M, Chioma L, Dallapiccola B, Prokopenko I, Manco M (2022) Relationship between glucose homeostasis and obesity in early life-a study of Italian children and adolescents. Hum Mol Genet 31(5):816–826. https://doi.org/10.1093/hmg/ddab287
Shashaj B, Luciano R, Contoli B, Morino GS, Spreghini MR, Rustico C, Sforza RW, Dallapiccola B, Manco M (2016) Reference ranges of HOMA-IR in normal-weight and obese young Caucasians. Acta Diabetol 53(2):251–60. https://doi.org/10.1007/s00592-015-0782-4
Rosso C, Kazankov K, Younes R, Esmaili S, Marietti M, Sacco M, Carli F, Gaggini M, Salomone F, Møller HJ, Abate ML, Vilstrup H, Gastaldelli A, George J, Grønbæk H, Bugianesi E (2019) Crosstalk between adipose tissue insulin resistance and liver macrophages in non-alcoholic fatty liver disease. J Hepatol 71(5):1012–1021
MacAulay K, Doble BW, Patel S, Hansotia T, Sinclair EM, Drucker DJ, Nagy A, Woodgett JR (2007) Glycogen synthase kinase 3alpha-specific regulation of murine hepatic glycogen metabolism. Cell Metab 6(4):329–37. https://doi.org/10.1016/j.cmet.2007.08.013
Zhang J, Nakatsu Y, Shinjo T, Guo Y, Sakoda H, Yamamotoya T, Otani Y, Okubo H, Kushiyama A, Fujishiro M, Fukushima T, Tsuchiya Y, Kamata H, Iwashita M, Nishimura F, Katagiri H, Takahashi S, Kurihara H, Uchida T, Asano T (2013) Par14 protein associates with insulin receptor substrate 1 (IRS-1), thereby enhancing insulin-induced IRS-1 phosphorylation and metabolic actions. J Biol Chem 288(28):20692–701. https://doi.org/10.1074/jbc.M113.485730
Costantino S, Paneni F, Lüscher TF, Cosentino F (2016) Pin1 inhibitor Juglone prevents diabetic vascular dysfunction. Int J Cardiol 203:702–7. https://doi.org/10.1016/j.ijcard.2015.10.221 (Epub 2015 Oct 30 PMID: 26583846)
Nakatsu Y, Iwashita M, Sakoda H, Ono H, Nagata K, Matsunaga Y, Fukushima T, Fujishiro M, Kushiyama A, Kamata H, Takahashi S, Katagiri H, Honda H, Kiyonari H, Uchida T, Asano T (2015) Prolyl isomerase Pin1 negatively regulates AMP-activated protein kinase (AMPK) by associating with the CBS domain in the γ subunit. J Biol Chem 290(40):24255–66. https://doi.org/10.1074/jbc.M115.658559
Nakatsu Y, Matsunaga Y, Yamamotoya T, Ueda K, Inoue MK, Mizuno Y, Nakanishi M, Sano T, Yamawaki Y, Kushiyama A, Sakoda H, Fujishiro M, Ryo A, Ono H, Minamino T, Takahashi SI, Ohno H, Yoneda M, Takahashi K, Ishihara H, Katagiri H, Nishimura F, Kanematsu T, Yamada T, Asano T (2019) Prolyl Isomerase Pin1 suppresses thermogenic programs in adipocytes by promoting degradation of transcriptional co-activator PRDM16. Cell Rep 26(12):3221-3230e3. https://doi.org/10.1016/j.celrep.2019.02.066
Nakatsu Y, Sakoda H, Kushiyama A, Ono H, Fujishiro M, Horike N, Yoneda M, Ohno H, Tsuchiya Y, Kamata H, Tahara H, Isobe T, Nishimura F, Katagiri H, Oka Y, Fukushima T, Takahashi SI, Kurihara H, Uchida T, Asano T (2010) Pin1 associates with and induces translocation of CRTC2 to the cytosol, thereby suppressing cAMP-responsive element transcriptional activity. J Biol Chem 285(43):33018–33027. https://doi.org/10.1074/jbc.M110.137836
Lee YH, Martin JM, Maple RL, Tharp WG, Pratley RE (2009) Plasma amyloid-beta peptide levels correlate with adipocyte amyloid precursor protein gene expression in obese individuals. Neuroendocrinology 90(4):383–390. https://doi.org/10.1159/000235555
Stinson SE, Jonsson AE, Lund MAV, Frithioff-Bøjsøe C, Aas Holm L, Pedersen O, Ängquist L, Sørensen TIA, Holst JJ, Christiansen M, Holm JC, Hartmann B, Hansen T (2021) Fasting plasma GLP-1 is associated with overweight/obesity and cardiometabolic risk factors in children and adolescents. J Clin Endocrinol Metab 106(6):1718–1727. https://doi.org/10.1210/clinem/dgab098
Manell H, Staaf J, Manukyan L, Kristinsson H, Cen J, Stenlid R, Ciba I, Forslund A, Bergsten P (2016) Altered plasma levels of glucagon, GLP-1 and glicentin during OGTT in adolescents with obesity and type 2 diabetes. J Clin Endocrinol Metab 101(3):1181–9. https://doi.org/10.1210/jc.2015-3885
Carlsson M, Wessman Y, Almgren P, Groop L (2000) High levels of nonesterified fatty acids are associated with increased familial risk of cardiovascular disease. Arterioscler Thromb Vasc Biol 20(6):1588–94. https://doi.org/10.1161/01.atv.20.6.1588
Grundy SM (2015) Adipose tissue and metabolic syndrome: too much, too little or neither. Eur J Clin Invest 45(11):1209–17. https://doi.org/10.1111/eci.12519
Johnston LW, Harris SB, Retnakaran R, Giacca A, Liu Z, Bazinet RP, Hanley AJ (2018) Association of NEFA composition with insulin sensitivity and beta cell function in the prospective metabolism and islet cell evaluation (PROMISE) cohort. Diabetologia 61(4):821–830. https://doi.org/10.1007/s00125-017-4534-6
Funding
This research was funded by the Italian Ministry of Health under the funding scheme “5 x mille”) to M.M. (#201905 MULTI MANCO 1).
Author information
Authors and Affiliations
Contributions
MB: serum assays, data curation and analysis, writing—original draft preparation. MM: conceptualization, funding acquisition, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest. M.M. is member of the Editorial Board of JENI.
Research involving human participants and/or animals
This article does not contain any study on animals. The study research on humans was conducted in line with the Declaration of Helsinky. The Ethical approval was obtained from the Ethics Committee at the “Ospedale Pediatrico Bambino Gesù” (2050_OPBG_2020).
Consent to participate
Written informed consent was obtained from the parents and legal guardians. Patients’ data were treated to guarantee confidentiality.
Consent for publication
Both authors have read and agreed to the published article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bianchi, M., Manco, M. Circulating levels of PIN1 and glucose metabolism in young people with obesity. J Endocrinol Invest 45, 1741–1748 (2022). https://doi.org/10.1007/s40618-022-01812-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01812-8