Abstract
Background
Roux‐en‐Y gastric bypass (RYGB) has been widely reported to be safe and feasible, and has a powerful effect on improving metabolism and weight loss in patients with a high body mass index (BMI). A few studies have focused on the comparison of RYGB with medical treatment in type 2 diabetes (T2D) patients with a lower BMI.
Objectives
To compare the metabolic effects and safety of RYGB versus medical treatment during a 2 years follow-up in T2D patients with a BMI of 25 to 32.5 kg/m2.
Methods
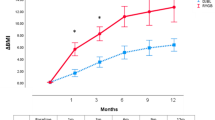
This retrospective and multicenter cohort study participants were extracted from the T2D patients with a lower BMI (25–32.5 kg/m2) from three bariatric centers between 2009 and 2018. Propensity score matching (PSM) was used to minimize bias, and each patient in the surgical group was matched 1:2 to the patients in the medical group with the closest propensity score. Finally, 71 patients who received RYGB and 142 patients who underwent medical treatment with a 2 years follow-up were enrolled to compare the effects of RYGB and medical treatment. The primary endpoint was achievement of the triple endpoint (the simultaneous achievement of hemoglobin A1c (HbA1c) < 7.0%, fasting low-density lipoprotein cholesterol (LDL-C) < 100 mg/dL (2.6 mmol/L), and systolic blood pressure (SBP) < 130 mmHg at the year-1 visit). Changes in weight, BMI, medication usage, complications, and adverse events were assessed.
Results
In total, 213 patients (mean age of 47.4 ± 9.5 years, 70.4% male, mean BMI of 28.6 ± 2.2 kg/m2) were included in this study. At the end of the first year, 17 patients (23.9%) in the surgical group and 10 (7.0%) in the medical group had achieved the composite triple endpoint (OR 4.64; 95% CI 1.82–11.81; p = 0.001). Additionally, 43 patients (60.6%) in the surgical group and 11 patients (19.7%) in the medical group experienced remission of T2D. However, more complications were observed in the surgical group (36 vs. 22, p < 0.01).
Conclusions
Among T2D patients with a BMI between 25.0 and 32.5 kg/m2, RYGB was more effective than medical treatment in resolving metabolic disorders and also resulted in more complications. The risk for complications should be considered in the clinical decision-making process for T2D patients with a low BMI.


Similar content being viewed by others
References:
World Health Organization. Diabetes [Internet]. Accessed 21 July 2020. https://www.who.int/health-topics/diabetes
Zomer E, Gurusamy K, Leach R et al (2016) Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Obes Rev 17(10):1001–1011
Haw JS, Galaviz KI, Straus AN et al (2017) Long-term sustainability of diabetes prevention approaches: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med 177(12):1808–1817
Pories WJ, Swanson MS, MacDonald KG et al (1995) Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222(3):339–350 (Discussion 350-332)
Cummings DE, Cohen RV (2014) Beyond BMI: the need for new guidelines governing the use of bariatric and metabolic surgery. Lancet Diabetes Endocrinol 2(2):175–181
Mingrone G, Panunzi S, De Gaetano A et al (2012) Bariatric surgery versus conventional medical therapy for T2D. N Engl J Med 366(17):1577–1585
Mingrone G, Panunzi S, De Gaetano A et al (2015) Bariatric-metabolic surgery versus conventional medical treatment in obese patients with T2D: 5 year follow-up of an open-label, single-centre, randomized controlled trial. Lancet 386(9997):964–973
Schauer PR, Bhatt DL, Kirwan JP et al (2017) Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med 376(7):641–651
Ikramuddin S, Korner J, Lee WJ et al (2016) Durability of addition of Roux-en-Y gastric bypass to lifestyle intervention and medical management in achieving primary treatment goals for uncontrolled T2D in mild to moderate obesity: a randomized control trial. Diabetes Care 39(9):1510–1518
Fisher DP, Johnson E, Haneuse S et al (2018) Association between bariatric surgery and macrovascular disease outcomes in patients With T2D and severe obesity. JAMA 320(15):1570–1582
Thorpe LE, Upadhyay UD, Chamany S et al (2009) Prevalence and control of diabetes and impaired fasting glucose in New York City. Diabetes Care 32(1):57–62
Palaniappan L, Wang Y, Fortmann SP (2004) Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol 14(7):499–506
O’Brien R, Johnson E, Haneuse S et al (2018) Microvascular outcomes in patients with diabetes after bariatric surgery versus usual care: a matched cohort study. Ann Intern Med 169(5):300–310
der Angelantonio E, Bhupathiraju Sh N, Global BMIMC et al (2016) Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388(10046):776–786
Coutinho T, Goel K, der Corrêa Sá D et al (2013) Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of “normal weight central obesity”. J Am Coll Cardiol 61(5):553–560
Boffetta P, McLerran D, Chen Y et al (2011) Body mass index and diabetes in Asia: a cross-sectional pooled analysis of 900,000 individuals in the Asia cohort consortium. PLoS One 6(6):e19930
Ji G, Li W, Li P et al (2020) Effect of Roux-en-Y gastric bypass for patients with T2D mellitus and a BMI < 32.5 kg/m2: a 6-year study in Chinese patients. Obes Surg 30(7):2631–2636
Yong W, Cunchuan W, Shaihong Z et al (2019) Chinese guidelines for surgical treatment of obesity and T2D (in Chinese). Chin J Pract Surg 39(04):301–306
American DA (2011) Standards of medical care in diabetes–2011. Diabetes Care 34(Suppl 1):S11-61
Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 39(33):3021–3104
Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K (2003) American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation 107(11):1562–1566
American Diabetes Association (2020) 16. Diabetes advocacy: standards of medical care in diabetes-2019. Diabetes Care 43(Suppl 1):S203–S204
Jia W, Weng J, Zhu D et al (2019) Standards of medical care for T2D in China 2019. Diabetes Metab Res Rev 35(6):e3158
Buse JB, Caprio S, Cefalu WT et al (2009) How do we define cure of diabetes? Diabetes Care 32(11):2133–2135
Brethauer SA, Kim J, El Chaar M et al (2015) Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg 25(4):587–606
The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group (1991) Perioperative total parenteral nutrition in surgical patients. N Engl J Med 325(8):525–532
Bouillanne O, Morineau G, Dupont C et al (2005) Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 82(4):777–783
Minamisawa M, Seidelmann SB, Claggett B et al (2019) Impact of malnutrition using geriatric nutritional risk index in heart failure with preserved ejection fraction. JACC Heart failure 7(8):664–675
Austin PC (2008) A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med 27(12):2037–2049
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28(25):3083–3107
Ikramuddin S, Korner J, Lee WJ et al (2018) Lifestyle intervention and medical management with vs without Roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the diabetes surgery study. JAMA 319(3):266–278
Feng W, Yin T, Chu X et al (2019) Metabolic effects and safety of Roux-en-Y gastric bypass surgery vs. conventional medication in obese Chinese patients with T2D. Diabetes Metab Res Rev 35(5):e3138
Ikramuddin S, Billington CJ, Lee WJ et al (2015) Roux-en-Y gastric bypass for diabetes (the Diabetes Surgery Study): 2-year outcomes of a 5-year, randomized, controlled trial. Lancet Diabetes Endocrinol 3(6):413–422
Schauer PR, Burguera B, Ikramuddin S et al (2003) Effect of laparoscopic Roux-en Y gastric bypass on T2D mellitus. Ann Surg 238(4):467–484 (Discussion 484-465)
Sjostrom L, Peltonen M, Jacobson P et al (2014) Association of bariatric surgery with long-term remission of T2D and with microvascular and macrovascular complications. JAMA 311(22):2297–2304
Arterburn DE, Olsen MK, Smith VA et al (2015) Association between bariatric surgery and long-term survival. JAMA 313(1):62–70
Maggard-Gibbons M, Maglione M, Livhits M et al (2013) Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes: a systematic review. JAMA 309(21):2250–2261
Muller-Stich BP, Senft JD, Warschkow R et al (2015) Surgical versus medical treatment of T2D mellitus in nonseverely obese patients: a systematic review and meta-analysis. Ann Surg 261(3):421–429
Arterburn DE, Telem DA, Kushner RF, Courcoulas AP (2020) Benefits and risks of bariatric surgery in adults: a review. JAMA 324(9):879–887
Aminian A, Brethauer SA, Andalib A et al (2017) Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg 266(4):650–657
Still CD, Wood GC, Benotti P et al (2014) Preoperative prediction of T2D remission after Roux-en-Y gastric bypass surgery: a retrospective cohort study. Lancet Diabetes Endocrinol 2(1):38–45
Wilhelm SM, Young J, Kale-Pradhan PB (2014) Effect of bariatric surgery on hypertension: a meta-analysis. Ann Pharmacother 48(6):674–682
Schiavon CA, Bersch-Ferreira AC, Santucci EV et al (2018) Effects of bariatric surgery in obese patients with hypertension: the GATEWAY randomized trial (gastric bypass to treat obese patients with steady hypertension). Circulation 137(11):1132–1142
Climent E, Goday A, Pedro-Botet J et al (2020) Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for 5-year hypertension remission in obese patients: a systematic review and meta-analysis. J Hypertens 38(2):185–195
Gloy VL, Briel M, Bhatt DL et al (2013) Bariatric surgery versus nonsurgical treatment for obesity: a systematic review and meta-analysis of randomized controlled trials. BMJ 347:f5934
Oh CA, Kim DH, Oh SJ et al (2012) Nutritional risk index as a predictor of postoperative wound complications after gastrectomy. World J Gastroenterol 18(7):673–678
American Society for Metabolic and Bariatric Surgery. Estimate of bariatric surgery numbers, 2011–2018. Accessed 10 Oct 2020. https://asmbs.org/resources/estimate-of-bariatric-surgerynumbers
Acknowledgements
The authors would like to thank the research assistants and medical students who provided assistances with the study (Jun Li, Chaoqiang Cai, and Xiang Gao, from the Hospital 2); members of this multicenter study at the Hospital 1; and the Hospital 3.
Funding
This research was supported by the program of China–Japan Friendship Hospital introduction of talents grant (2018-RC-1) and by Research and promotion of clinical characteristics and results in Capital (Z151100004015065).
Author information
Authors and Affiliations
Contributions
SZ and LZ take responsibility for the contents of the article. JL and HT have contributed equally to this article. Study design: LZ, SZ, HM, and LW. Acquisition and analysis of data: LZ, HM, and LW. Drafting of the manuscript: JL and HT. Revision of the draft paper and final approval: LZ and SZhu. Statistical analysis: JL and HT.
Corresponding authors
Ethics declarations
Conflict of interest
None reported.
Research involving human participants and/or animals
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Declaration of Helsinki.
Informed consent
Written informed consent for the study was obtained from all individual participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ling, J., Tang, H., Meng, H. et al. Two-year outcomes of Roux‐en‐Y gastric bypass vs medical treatment in type 2 diabetes with a body mass index lower than 32.5 kg/m2: a multicenter propensity score-matched analysis. J Endocrinol Invest 45, 1729–1740 (2022). https://doi.org/10.1007/s40618-022-01811-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01811-9