Abstract
Purpose
Undercarboxylated-Osteocalcin (ucOCN), acting on its putative receptor GPRC6A, was shown to stimulate testosterone (T) production by Leydig cells in rodents, in parallel with the hypothalamus-pituitary–gonadal axis (HPG) mediated by luteinizing hormone (LH). The aim of this cross-sectional study was to evaluate the association among serum ucOCN, rs2247911 polymorphism of GPRC6A gene and the endocrine/semen pattern in a cohort of infertile males, possibly identifying an involvement of the ucOCN-GPRC6A axis on testis function.
Methods
190 males, including 74 oligozoospermic subjects, 58 azoosperminc patients and 58 normozoospermic controls, were prospectively recruited at the Orient Hospital for Infertility, Assisted Reproduction and Genetics in Syria (Study N. 18FP), from July 2018 to June 2020. Outpatient evaluation included the clinical history, anthropometrics and a fasting blood sampling for hormonals, serum OCN (both carboxylated and undercarboxylated), glycemic and lipid profile and screening for rs2247911 GPRC6A gene polymorphism.
Results
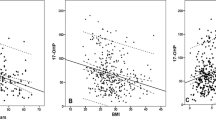
Higher serum ucOCN associated with higher T and HDL-cholesterol (respectively: r = 0.309, P < 0.001 and r = 0.248, P = 0.001), and with lower FSH (r = – 0.327, P < 0.001) and LDL-cholesterol (r = – 0.171; P = 0.018). Patients bearing the GG genotype of rs2247911 had higher sperm count compared to GA genotype (P = 0.043) and, compared to both AG and AA genotypes, had higher serum T (P = 0.004, P = 0.001) and lower triglycerides levels (P = 0.002, P < 0.001). Upon normalization for LH levels and body mass index, rs2274911 and ucOCN were significantly associated with higher serum T at linear stepwise regression analysis (P = 0.013, P = 0.007).
Conclusions
Our data suggest the involvement of ucOCN-GPRC6A axis in the regulation of T production by the testis, subsidiary to HPG.
Similar content being viewed by others
References
Kaprara A, Huhtaniemi IT (2018) The hypothalamus-pituitary-gonad axis: Tales of mice and men. Metabolism: clinical and experimental 86:3–17. https://doi.org/10.1016/J.METABOL.2017.11.018
Karsenty G (2017) Update on the biology of osteocalcin. Endocr Pract 23:1270–1274. https://doi.org/10.4158/EP171966.RA
Hauschka PV, Lian JB, Cole DE, Gundberg CM (1989) Osteocalcin and matrix Gla protein: vitamin K-dependent proteins in bone. Physiol Rev 69:990–1047. https://doi.org/10.1152/PHYSREV.1989.69.3.990
Price PA (1985) Vitamin K-dependent formation of bone gla protein (Osteocalcin) and its function. Vitam Horm 42:65–108. https://doi.org/10.1016/S0083-6729(08)60061-8
Ducy P, Desbois C, Boyce B et al (1996) Increased bone formation in osteocalcin-deficient mice. Nature 382:448–452. https://doi.org/10.1038/382448a0
Cristiani A, Maset F, De Toni L et al (2014) Carboxylation-dependent conformational changes of human osteocalcin. Front Biosci 19:1105–1116. https://doi.org/10.2741/4270
Wei J, Karsenty G (2015) An overview of the metabolic functions of osteocalcin. Rev Endocr Metab Disord 16:93–98. https://doi.org/10.1007/S11154-014-9307-7
Ferron M, Wei J, Yoshizawa T et al (2010) Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell 142:296–308. https://doi.org/10.1016/j.cell.2010.06.003
Foresta C, Strapazzon G, De Toni L et al (2011) Androgens modulate osteocalcin release by human visceral adipose tissue. Clin Endocrinol 75:64–69. https://doi.org/10.1111/j.1365-2265.2011.03997.x
Wei J, Hanna T, Suda N et al (2014) Osteocalcin promotes β-cell proliferation during development and adulthood through Gprc6a. Diabetes 63:1021–1031. https://doi.org/10.2337/db13-0887
Shahrour HE, Al Fahom S, Al-Massarani G et al (2022) Osteocalcin-expressing endothelial progenitor cells and serum osteocalcin forms are independent biomarkers of coronary atherosclerotic disease severity in male and female patients. J Endocrinol Invest. https://doi.org/10.1007/S40618-022-01744-3
Ferron M, Hinoi E, Karsenty G, Ducy P (2008) Osteocalcin differentially regulates β cell and adipocyte gene expression and affects the development of metabolic diseases in wild-type mice. Proc Natl Acad Sci USA 105:5266–5270. https://doi.org/10.1073/pnas.0711119105
Karsenty G, Mera P (2018) Molecular bases of the crosstalk between bone and muscle. Bone 115:43–49. https://doi.org/10.1016/j.bone.2017.04.006
Karsenty G (2012) The mutual dependence between bone and gonads. J Endocrinol 213:107–114. https://doi.org/10.1530/JOE-11-0452
Pi M, Quarles LD (2012) Multiligand specificity and wide tissue expression of GPRC6A reveals new endocrine networks. Endocrinology 153:2062–2069. https://doi.org/10.1210/EN.2011-2117
Khrimian L, Obri A, Ramos-Brossier M et al (2017) Gpr158 mediates osteocalcin’s regulation of cognition. J Exp Med. https://doi.org/10.1084/jem.20171320
Lee NK, Sowa H, Hinoi E et al (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130:456–469. https://doi.org/10.1016/j.cell.2007.05.047
Oury F, Sumara G, Sumara O et al (2011) Endocrine regulation of male fertility by the skeleton. Cell 144:796–809. https://doi.org/10.1016/j.cell.2011.02.004
Pi M, Chen L, Huang MZ et al (2008) GPRC6A null mice exhibit osteopenia, feminization and metabolic syndrome. PLoS ONE. https://doi.org/10.1371/journal.pone.0003858
Ferron M, Lacombe J (2014) Regulation of energy metabolism by the skeleton: osteocalcin and beyond. Arch Biochem Biophys 561:137–146. https://doi.org/10.1016/J.ABB.2014.05.022
Oury F, Ferron M, Huizhen W et al (2013) Osteocalcin regulates murine and human fertility through a pancreas-bone-testis axis. J Clin Investig 123:2421–2433. https://doi.org/10.1172/JCI65952.insulin
Haiman CA, Han Y, Feng Y et al (2013) Genome-wide testing of putative functional exonic variants in relationship with breast and prostate cancer risk in a multiethnic population. PLoS Genet 9:e1003419. https://doi.org/10.1371/journal.pgen.1003419
De Toni L, Di Nisio A, Rocca MS et al (2017) Osteocalcin, a bone-derived hormone with important andrological implications. Andrology 5:664–670. https://doi.org/10.1111/ANDR.12359
Sarah M Paksima, Hala N Madanat, Steven R Hawks (2002) A contextual model for reproductive health education: fertility and family planning in Jordan - PubMed. In: Promot Edu. https://pubmed.ncbi.nlm.nih.gov/12426969/. Accessed 4 Mar 2022
(2014) WHO | Infecundity, infertility, and childlessness in developing countries. Demographic and Health Surveys (DHS) Comparative reports No. 9. WHO
Garolla A, Grande G, Palego P et al (2021) Central role of ultrasound in the evaluation of testicular function and genital tract obstruction in infertile males. Andrology 9:1490–1498. https://doi.org/10.1111/ANDR.13060
(2010) WHO laboratory manual for the Examination and processing of human semen FIFTH EDITION
Hosker JP, Matthews DR, Rudenski AS et al (1985) Continuous infusion of glucose with model assessment: measurement of insulin resistance and β-cell function in man. Diabetologia 28:401–411. https://doi.org/10.1007/BF00280882
Di Nisio A, Rocca MS, Fadini GP et al (2017) The rs2274911 polymorphism in GPRC6A gene is associated with insulin resistance in normal weight and obese subjects. Clin Endocrinol 86:185–191. https://doi.org/10.1111/cen.13248
Karsenty G, Oury F (2014) Regulation of male fertility by the bone-derived hormone osteocalcin. Mol Cell Endocrinol 382:521–526. https://doi.org/10.1016/J.MCE.2013.10.008
Oury F (2012) A crosstalk between bone and gonads. Ann N Y Acad Sci 1260:1–7. https://doi.org/10.1111/J.1749-6632.2011.06360.X
Diegel CR, Hann S, Ayturk UM et al (2020) An osteocalcin-deficient mouse strain without endocrine abnormalities. PLoS Genet 16:e1008361. https://doi.org/10.1371/JOURNAL.PGEN.1008361
Lin X, Hanson E, Betik AC et al (2016) Hindlimb Immobilization, But Not Castration, Induces Reduction of Undercarboxylated Osteocalcin Associated With Muscle Atrophy in Rats. J Bone Miner Res 31:1967–1978. https://doi.org/10.1002/JBMR.2884
Karsenty G, Oury F (2014) Molecular and Cellular Endocrinology Regulation of male fertility by the bone-derived hormone osteocalcin. Mol Cell Endocrinol 382:521–526. https://doi.org/10.1016/j.mce.2013.10.008
Agas D, Lacava G, Sabbieti MG (2018) Bone and bone marrow disruption by endocrine-active substances. J Cell Physiol 234:192–213. https://doi.org/10.1002/JCP.26837
Kirmani S, Atkinson EJ, Melton LJ et al (2011) Relationship of testosterone and osteocalcin levels during growth. J Bone Miner Res 26:2212–2216. https://doi.org/10.1002/jbmr.421
Hiam D, Landen S, Jacques M et al (2021) Osteocalcin and its forms respond similarly to exercise in males and females. Bone. https://doi.org/10.1016/J.BONE.2020.115818
Kanazawa I, Tanaka K, Ogawa N et al (2013) Undercarboxylated osteocalcin is positively associated with free testosterone in male patients with type 2 diabetes mellitus. Osteoporos Int 24:1115–1119. https://doi.org/10.1007/s00198-012-2017-7
Yang Y, Zheng S, Wang W et al (2019) Osteocalcin levels in male idiopathic hypogonadotropic hypogonadism: relationship with the testosterone secretion and metabolic profiles. Front Endocrin 10:1–7. https://doi.org/10.3389/fendo.2019.00687
De Toni L, De Nisio A, Speltra E et al (2016) Polymorphism rs2274911 of GPRC6A as a novel risk factor for testis failure. J Clin Endocrinol Metabol 101:953–961. https://doi.org/10.1210/jc.2015-3967
Skakkebæk NE, Lindahl-Jacobsen R, Levine H et al (2022) Environmental factors in declining human fertility. Nat Rev Endocrinol 18:139–157. https://doi.org/10.1038/S41574-021-00598-8
De Toni L, Jawich K, De Rocco PM et al (2020) Osteocalcin: a protein hormone connecting metabolism, bone and testis function. Protein Pept Lett 27:1268–1275. https://doi.org/10.2174/0929866527666200505220459
Sharma R, Biedenharn KR, Fedor JM, Agarwal A (2013) Lifestyle factors and reproductive health: Taking control of your fertility. Reprod Biol Endocrinol 11:1–15. https://doi.org/10.1186/1477-7827-11-66/TABLES/1
Syria crisis. https://www.who.int/emergencies/situations/syria-crisis. Accessed 2 Jul 2021
Yeap BB, Alfonso H, Paul Chubb SA et al (2015) Higher serum undercarboxylated osteocalcin and other bone turnover markers are associated with reduced diabetes risk and lower estradiol concentrations in older men. J Clin Endocrinol Metab 100:63–71. https://doi.org/10.1210/JC.2014-3019
Acknowledgements
We thank Dr. Khaled Albaghdadi, Dr. Nemah ALsayed Jameel and Farah Brangakgi for their assistance in data collection.
Funding
This study received the support of the University Cooperation Initiatives, University of Padova, Italy and the Scientific Research Support Fund, Ministry of Higher Education and Scientific Research, Syrian Arab Republic.
Author information
Authors and Affiliations
Contributions
K.J. and M.S.R. were responsible for data collection. Data management was performed by K.J., M.S.R. and L.D.T. All authors contributed to the study conception and design. A.D.N. performed the statistical analyses. K.J., S.A.F., M.A., A.F. and L.D.T. drafted the manuscript. C.F. supervised manuscript concept and design. All authors took part in the revision of the manuscript and approved the final version for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
The study was approved by the Ethics Committee of Damascus University (protocol number N.18FP,2018).
Human rights
All procedures in this study were performed in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and subsequent amendments or comparable ethical standards.
Informed consent
Appropriate informed consent was acquired from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jawich, K., Rocca, M.S., Al Fahoum, S. et al. RS 2247911 polymorphism of GPRC6A gene and serum undercarboxylated-osteocalcin are associated with testis function. J Endocrinol Invest 45, 1673–1682 (2022). https://doi.org/10.1007/s40618-022-01803-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01803-9