Abstract
Purpose
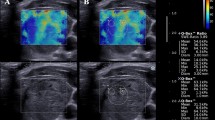
To assess the diagnostic value of SuperSonic shear imaging (SSI) for the differentiation between benign and malignant thyroid nodules through meta-analysis.
Methods
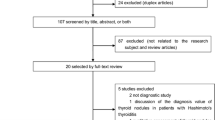
Online database searches were performed on PubMed, EMBASE, the Cochrane Library, and the Web of Science until 31 July 2021. The Quality Assessment of Diagnostic Accuracy Studies-2 tool was used to assess the quality of the included studies. Three measures of diagnostic test performance were used to examine the value of SSI, including the summary area under the receiver operating characteristic curve (AUROC), the summary diagnostic odds ratio (DOR), and the summary sensitivity and specificity. Heterogeneity was explored using meta-regression and subgroup analyses.
Results
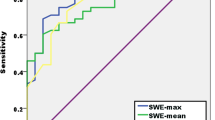
Finally, 21 studies with 3376 patients were included in this study. There were a total of 4296 thyroid nodules, in which 1806 malignant nodules and 2490 benign ones were involved. Thyroid nodules exhibited a malignancy rate of 42.0% (range 5.6–79.8%), 95.1% of which were of papillary variant. SSI showed a summary sensitivity of 74% [95% confidence interval (CI) 67–79%], specificity of 82% (95% CI 77–87%) and AUROC of 0.85 (95% CI 0.82–0.88) for the differentiation between benign and malignant thyroid nodules. The summary positive likelihood ratio (LR), negative LR, and DOR were 4.2 (95% CI 3.3–5.3), 0.32 (95% CI 0.26–0.40), and 13 (95% CI 9–18), respectively.
Conclusions
SSI showed high accuracy in the diagnostic differentiation between benign and malignant thyroid nodules and can be served as a noninvasive and important adjunct for thyroid nodule evaluation.






Similar content being viewed by others
References
Koh J, Lee E, Han K et al (2020) Diagnosis of thyroid nodules on ultrasonography by a deep convolutional neural network. Sci Rep 10:15245
Sebag F, Vaillant-Lombard J, Berbis J et al (2010) Shear wave elastography: a new ultrasound imaging mode for the differential diagnosis of benign and malignant thyroid nodules. J Clin Endocrinol Metab 95:5281–5288
Burman KD, Wartofsky L (2015) Clinical practice. Thyroid nodules. N Engl J Med 373:2347–2356
Zhou H, Jin Y, Dai L et al (2020) Differential diagnosis of benign and malignant thyroid nodules using deep learning radiomics of thyroid ultrasound images. Eur J Radiol 127:108992
Angell TE, Maurer R, Wang Z et al (2019) A cohort analysis of clinical and ultrasound variables predicting cancer risk in 20,001 consecutive thyroid nodules. J Clin Endocrinol Metab 104:5665–5672
Zhang F, Yu X, Lin Z et al (2021) Using tumor-infiltrating immune cells and a ceRNA network model to construct a prognostic analysis model of thyroid carcinoma. Front Oncol 11:658165
Wong R, Farrell SG, Grossmann M (2018) Thyroid nodules: diagnosis and management. Med J Aust 209:92–98
Cappelli C, Pirola I, Agosti B et al (2017) Complications after fine-needle aspiration cytology: a retrospective study of 7449 consecutive thyroid nodules. Br J Oral Maxillofac Surg 55:266–269
Moon WJ, Jung SL, Lee JH et al (2008) Benign and malignant thyroid nodules: US differentiation–multicenter retrospective study. Radiology 247:762–770
Grani G, Sponziello M, Pecce V et al (2020) Contemporary thyroid nodule evaluation and management. J Clin Endocrinol Metab 105:2869–2883
Roth MY, Witt RL, Steward DL (2018) Molecular testing for thyroid nodules: review and current state. Cancer 124:888–898
Bongiovanni M, Spitale A, Faquin WC et al (2012) The Bethesda system for reporting thyroid cytopathology: a meta-analysis. Acta Cytol 56:333–339
Shiina T, Nightingale KR, Palmeri ML et al (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 1: basic principles and terminology. Ultrasound Med Biol 41:1126–1147
Filho RHC, Pereira FL, Iared W (2020) Diagnostic accuracy evaluation of two-dimensional shear wave elastography in the differentiation between benign and malignant thyroid nodules: systematic review and meta-analysis. J Ultrasound Med 39:1729–1741
Swan KZ, Nielsen VE, Bonnema SJ (2021) Evaluation of thyroid nodules by shear wave elastography: a review of current knowledge. J Endocrinol Invest 44:2043–2056
Cosgrove D, Barr R, Bojunga J et al (2017) WFUMB guidelines and recommendations on the clinical use of ultrasound elastography: part 4. thyroid. Ultrasound Med Biol 43:4–26
Pei S, Zhang B, Cong S et al (2020) Ultrasound real-time tissue elastography improves the diagnostic performance of the ACR Thyroid Imaging Reporting and Data System in differentiating malignant from benign thyroid nodules: a summary of 1525 thyroid nodules. Int J Endocrinol 2020:1749351
Bhatia KS, Tong CS, Cho CC et al (2012) Shear wave elastography of thyroid nodules in routine clinical practice: preliminary observations and utility for detecting malignancy. Eur Radiol 22:2397–2406
McInnes MDF, Moher D, Thombs BD et al (2018) Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319:388–396
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Veyrieres JB, Albarel F, Lombard JV et al (2012) A threshold value in Shear Wave elastography to rule out malignant thyroid nodules: a reality? Eur J Radiol 81:3965–3972
Kim H, Kim JA, Son EJ et al (2013) Quantitative assessment of shear-wave ultrasound elastography in thyroid nodules: diagnostic performance for predicting malignancy. Eur Radiol 23:2532–2537
Szczepanek-Parulska E, Wolinski K, Stangierski A et al (2014) Biochemical and ultrasonographic parameters influencing thyroid nodules elasticity. Endocrine 47:519–527
Liu BX, Xie XY, Liang JY et al (2014) Shear wave elastography versus real-time elastography on evaluation thyroid nodules: a preliminary study. Eur J Radiol 83:1135–1143
Liu B, Liang J, Zheng Y et al (2015) Two-dimensional shear wave elastography as promising diagnostic tool for predicting malignant thyroid nodules: a prospective single-centre experience. Eur Radiol 25:624–634
Park AY, Son EJ, Han K et al (2015) Shear wave elastography of thyroid nodules for the prediction of malignancy in a large scale study. Eur J Radiol 84:407–412
Samir AE, Dhyani M, Anvari A et al (2015) Shear-wave elastography for the preoperative risk stratification of follicular-patterned lesions of the thyroid: diagnostic accuracy and optimal measurement plane. Radiology 277:565–573
Liu B, Liang J, Zhou L et al (2015) Shear wave elastography in the diagnosis of thyroid nodules with coexistent chronic autoimmune hashimoto’s thyroiditis. Otolaryngol Head Neck Surg 153:779–785
Duan SB, Yu J, Li X et al (2016) Diagnostic value of two-dimensional shear wave elastography in papillary thyroid microcarcinoma. Onco Targets Ther 9:1311–1317
Dobruch-Sobczak K, Zalewska EB, Guminska A et al (2016) Diagnostic performance of shear wave elastography parameters alone and in combination with conventional B-mode ultrasound parameters for the characterization of thyroid nodules: a prospective, dual-center study. Ultrasound Med Biol 42:2803–2811
He YP, Xu HX, Wang D et al (2017) First experience of comparisons between two different shear wave speed imaging systems in differentiating malignant from benign thyroid nodules. Clin Hemorheol Microcirc 65:349–361
Chen M, Zhang KQ, Xu YF et al (2016) Shear wave elastography and contrast-enhanced ultrasonography in the diagnosis of thyroid malignant nodules. Mol Clin Oncol 5:724–730
Liu Z, Jing H, Han X et al (2017) Shear wave elastography combined with the thyroid imaging reporting and data system for malignancy risk stratification in thyroid nodules. Oncotarget 8:43406–43416
Zhao CK, Chen SG, Alizad A et al (2018) Three-dimensional shear wave elastography for differentiating benign from malignant thyroid nodules. J Ultrasound Med 37:1777–1788
Kyriakidou G, Friedrich-Rust M, Bon D et al (2018) Comparison of strain elastography, point shear wave elastography using acoustic radiation force impulse imaging and 2D-shear wave elastography for the differentiation of thyroid nodules. PLoS ONE 13:e0204095
Kim HJ, Kwak MK, Choi IH et al (2019) Utility of shear wave elastography to detect papillary thyroid carcinoma in thyroid nodules: efficacy of the standard deviation elasticity. Korean J Intern Med 34:850–857
Farghadani M, Tabatabaei SA, Barikbin R et al (2019) Comparing the sensitivity and specificity of two-dimensional shear wave elastography and fine needle aspiration in determining malignant thyroid nodules. Adv Biomed Res 8:30
Han RJ, Du J, Li FH et al (2019) Comparisons and combined application of two-dimensional and three-dimensional real-time shear wave elastography in diagnosis of thyroid nodules. J Cancer 10:1975–1984
Shang H, Wu B, Liu Z et al (2020) The effectiveness of shear wave elastography in the diagnosis of PTMC. Technol Health Care 28:221–226
Nattabi HA, Sharif NM, Yahya N et al (2017) Is diagnostic performance of quantitative 2D-shear wave elastography optimal for clinical classification of benign and malignant thyroid nodules?: a systematic review and meta-analysis. Acad Radiol S1076–6332(17):30369
Zhao CK, Ren TT, Yin YF et al (2021) A comparative analysis of two machine learning-based diagnostic patterns with thyroid imaging reporting and data system for thyroid nodules: diagnostic performance and unnecessary biopsy rate. Thyroid 31:470–481
Lin P, Chen M, Liu B et al (2014) Diagnostic performance of shear wave elastography in the identification of malignant thyroid nodules: a meta-analysis. Eur Radiol 24:2729–2738
Magri F, Chytiris S, Capelli V et al (2012) Shear wave elastography in the diagnosis of thyroid nodules: feasibility in the case of coexistent chronic autoimmune Hashimoto’s thyroiditis. Clin Endocrinol (Oxf) 76:137–141
Zhan J, Jin JM, Diao XH et al (2015) Acoustic radiation force impulse imaging (ARFI) for differentiation of benign and malignant thyroid nodules: a meta-analysis. Eur J Radiol 84:2181–2186
Cantisani V, David E, Grazhdani H et al (2019) Prospective evaluation of semiquantitative strain ratio and quantitative 2D ultrasound shear wave elastography (SWE) in association with TIRADS classification for thyroid nodule characterization. Ultraschall Med 40:495–503
Xu SL, Tian YY, Zhou Y et al (2020) Diagnostic value of circulating microRNAs in thyroid carcinoma: a systematic review and meta-analysis. Clin Endocrinol (Oxf) 93:489–498
Magri F, Chytiris S, Chiovato L (2016) The role of elastography in thyroid ultrasonography. Curr Opin Endocrinol Diabetes Obes 23:416–422
Funding
This work was supported by Sciences and Technology project of Fujian Provincial Department (2019J01166), Innovative medical research project of Fujian Province (2018-CX-33) and High-level talent program of sciences and technology project of Quanzhou (2018C044R).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Y., Dong, B., Jiang, Z. et al. SuperSonic shear imaging for the differentiation between benign and malignant thyroid nodules: a meta-analysis. J Endocrinol Invest 45, 1327–1339 (2022). https://doi.org/10.1007/s40618-022-01765-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01765-y