Abstract
Purpose
Sodium is essential to life. However, its dietary excess is detrimental to the cardiovascular system, and sodium restriction is a crucial step in cardiovascular prevention. Iodine deficiency has been fought worldwide for decades, and substantial success has been achieved introducing the use of iodine-enriched salt. Nevertheless, areas of iodine deficiency persist around the world, both in developing and industrialized countries, and a major concern affecting dietary sodium reduction programs is represented by a possible iodine intake deficiency. There are substantial differences in the source of alimentary iodine among countries, such as iodized salt added, household tap water, seafood, or salt employed in packaged food. It is clear that a sodium-restricted diet can induce differences in terms of iodine intake, depending on the country considered. Moreover, iodine status has undergone relevant changes in many countries in the last years.
Methods
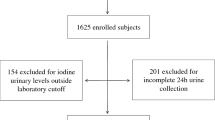
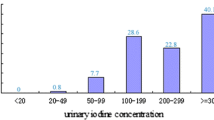
Systematic review of literature evidence about the possible effects of sodium restriction on population iodine status.
Results
To date, the available results are conflicting, depending on country, salt iodization policy, as well as time frame of data collection. However, to ensure an optimal iodine supply by salt fortification, without exceeding the current recommendation by World Health Organization for salt intake, seems to be an achievable goal.
Conclusion
A balanced approach may be obtained by an adequate iodine concentration in fortified salt and by promoting the availability of iodized salt for household consumption and food industry use. In this scenario, updated prospective studies are strongly needed.

Similar content being viewed by others
References
James PA, Oparil S, Carter BL et al (2014) 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA 311(5):507–520. https://doi.org/10.1001/jama.2013.284427
Van Horn L, Carson JAS, Appel LJ et al (2016) Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A scientific statement from the American Heart Association. Circulation 134(22):e505–e529. https://doi.org/10.1161/CIR.0000000000000462
Whelton PK, Carey RM, Aronow WS et al (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension 71(6):1269–1324. https://doi.org/10.1161/HYP.0000000000000066
Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 39(33):3021–3104. https://doi.org/10.1093/eurheartj/ehy339
Kotchen TA, Cowley AW Jr, Frohlich ED (2013) Salt in Health and Disease - A Delicate Balance. N Engl J Med 368(13):1229–1237. https://doi.org/10.1056/NEJMra1212606
Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP (2009) Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ 339:b4567. https://doi.org/10.1136/bmj.b4567
He FJ, MacGregor GA (2011) Salt reduction lowers cardiovascular risk: Meta-analysis of outcome trials. Lancet 378(9789):380–382. https://doi.org/10.1016/S0140-6736(11)61174-4
Taylor RS, Ashton KE, Moxham T et al (2011) Reduced dietary salt for the prevention of cardiovascular disease: A meta-analysis of randomized controlled trials (Cochrane review). Am J Hypertens 24(8):843–853. https://doi.org/10.1038/ajh.2011.115
Bram B, Huang X, Cupples WA, Hamza SM (2017) Understanding the two faces of low-salt intake. Curr Hypertens Rep 19(6):49. https://doi.org/10.1007/s11906-017-0744-z
Graudal N, Jurgens G, Baslund B, Alderman MH (2014) Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: A meta-analysis. Am J Hypertens 27(9):1129–1137. https://doi.org/10.1093/ajh/hpu028
O’Donnell M, Mente A, Rangarajan S et al (2014) Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med 371:612–623. https://doi.org/10.1056/NEJMoa1311889
Oparil S (2014) Low sodium intake-Cardiovascular health benefit or risk? N Engl J Med 371:677–679. https://doi.org/10.1056/NEJMe1407695
Manousou S, Stål M, Larsson C et al (2018) A Paleolithic-type diet results in iodine deficiency: a 2-year randomized trial in postmenopausal obese women. Eur J Clin Nutr 72(1):124–129. https://doi.org/10.1038/ejcn.2017.134
Kimball OP (1928) Endemic goiter and public health. Am J Public Health Nations Health 18(5):587–601. https://doi.org/10.2105/ajph.18.5.587
Iodine Global Network (2021) Global Scorecard of Iodine Nutrition in 2020 in the General Population Based on Schoolage Children. Ottawa, Canada: IGN. https://www.ign.org/scorecard.htm. Accessed 13 Dec. 2021
Lazarus JH (2014) Iodine status in Europe in 2014. Eur Thyroid J 3(1):3–6. https://doi.org/10.1159/000358873
Olivieri A, Di Cosmo C, De Angelis S et al (2017) Regional observatory for goiter prevention. The way forward in Italy for iodine. Minerva Med 108(2):159–168. https://doi.org/10.23736/S0026-4806.17.04877-7
Laurberg P, Cerqueira C, Ovesen L et al (2010) Iodine intake as a determinant of thyroid disorders in populations. Best Pract Res Clin Endocrinol Metab 24(1):13–27. https://doi.org/10.1016/j.beem.2009.08.013
World Health Organization (2014) Salt reduction and iodine fortification strategies in public health: report of a joint technical meeting convened by the world health organization and the George institute for global health in collaboration with the international council for the control of iodine deficiency disorders global network, Sydney, Australia. https://apps.who.int/iris/handle/10665/101509. Accessed 13 Dec. 2021
Tayie FA, Jourdan K (2010) Hypertension, dietary salt restriction and iodine deficiency among adults. Am J Hypertens 23(10):1095–1102. https://doi.org/10.1038/ajh.2010.120
Pearce EN, Andersson M, Zimmermann MB (2013) Global iodine nutrition: where do we stand in 2013? Thyroid 23(5):523–528. https://doi.org/10.1089/thy.2013.0128
Konig F, Andersson M, Hotz K et al (2011) Ten repeat collections for urinary from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J Nutr 141(11):2049–2054. https://doi.org/10.3945/jn.111.144071
Perrine CG, Cogswell ME, Swanson CA et al (2014) Comparison of population iodine estimates from 24-hour urine and timed-spot urine samples. Thyroid 24(4):748–757. https://doi.org/10.1089/thy.2013.0404
Ji C, Lu T, Dary O et al (2015) Systematic review of studies evaluating urinary iodine concentration as a predictor of 24 hour urinary iodine excretion for estimating population iodine intake. Rev Panam Salud Publica 38(1):73–81
Conkle J, van der Haar F (2017) The use and interpretation of sodium concentrations in casual (spot) urine collections for popu-lation surveillance and partitioning of dietary iodine intake sources. Nutrients 9(1):7. https://doi.org/10.3390/nu9010007
Simpson FO, Thaler BI, Paulin J et al (1984) Iodide excretion in a salt-restriction trial. N Z Med J 97(770):890–893
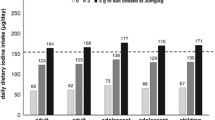
He FJ, Ma Y, Feng X et al (2016) Effect of salt reduction on iodine status assessed by 24 hour urinary iodine excretion in children and their families in northern China: A substudy of a cluster randomised controlled trial. BMJ Open 6(9):e011168. https://doi.org/10.1136/bmjopen-2016-011168
Vega-Vega O, Fonseca-Correa JI, Mendoza-De la Garza A et al (2018) Contemporary dietary intake: Too much sodium, not enough potassium, yet sufficient iodine: The SALMEX Cohort study. Nutrients 10(7):816. https://doi.org/10.3390/nu10070816
Charlton K, Ware LJ, Baumgartner J et al (2018) How will South Africa’s mandatory salt reduction policy affect its salt iodisation programme? A cross-sectional analysis from the WHO-SAGE Wave 2 Salt & Tobacco study. BMJ Open 8(3):e020404. https://doi.org/10.1136/bmjopen-2017-020404
Ershow AG, Skeaff SA, Merkel JM, Pehrsson PR (2018) Development of databases on iodine in foods and dietary supplements. Nutrients 10(1):100. https://doi.org/10.3390/nu10010100
Krela-Kaźmierczak I, Czarnywojtek A, Skoracka K et al (2021) Is there an ideal diet to protect against iodine deficiency? Nutrients 13(2):513. https://doi.org/10.3390/nu13020513
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Verkaik-Kloosterman J, van’t Veer P, Ocké MC, (2010) Reduction of salt: will iodine intake remain adequate in The Netherlands? Br J Nutr 104(11):1712–1718. https://doi.org/10.1017/S0007114510002722
Charlton KE, Jooste PL, Steyn K, Levitt NS, Ghosh A (2013) A lowered salt intake does not compromise iodine status in Cape Town, South Africa, where salt iodization is mandatory. Nutrition 29(4):630–634. https://doi.org/10.1016/j.nut.2012.09.010
Charlton K, Land MA, Ma G, Yeatman H, Houweling F (2014) Iodine status similarly suboptimal in Australian women who have desirable salt intakes compared to those with excessive intakes. Nutrition 30(2):234–235. https://doi.org/10.1016/j.nut.2013.05.009
Pastorelli AA, Stacchini P, Olivieri A (2015) Daily iodine intake and the impact of salt reduction on iodine prophylaxis in the Italian population. Eur J Clin Nutr 69(2):211–215. https://doi.org/10.1038/ejcn.2014.206
McMahon E, Webster J, O’Dea K, Brimblecombe J (2015) Dietary sodium and iodine in remote Indigenous Australian communities: will salt-reduction strategies increase risk of iodine deficiency? A cross-sectional analysis and simulation study. BMC Public Health 15:1318. https://doi.org/10.1186/s12889-015-2686-1
Land MA, Webster JL, Ma G et al (2016) Salt intake and iodine status of women in Samoa. Asia Pac J Clin Nutr 25(1):142–149. https://doi.org/10.6133/apjcn.2016.25.1.09
Musso N, Conte L, Carloni B et al (2018) Low-salt intake suggestions in hypertensive pa-tients do not jeopardize urinary iodine excretion. Nutrients 10(10):1548. https://doi.org/10.3390/nu10101548
Binnenmars SH, Corpeleijn E, Kwakernaak AJ et al (2019) Impact of moderate sodium restriction and hydrochlorothiazide on iodine excretion in diabetic kidney disease: data from a ran-domized cross-over trial. Nutrients 11(9):2204. https://doi.org/10.3390/nu11092204
Iacone R, Iaccarino Idelson P, Campanozzi A et al (2020) MINISAL-GIRCSI Study Group. Relationship between salt consumption and iodine intake in a pediatric population. Eur J Nutr 60(4):2193–2202. https://doi.org/10.1007/s00394-020-02407-w
Esche J, Thamm M, Remer T (2020) Contribution of iodized salt to total iodine and total salt intake in Germany. Eur J Nutr 59(7):3163–3169. https://doi.org/10.1007/s00394-019-02154-7
Menyanu E, Corso B, Minicuci N et al (2020) Salt-reduction strategies may compromise salt iodization programs: Learnings from South Africa and Ghana. Nutrition 84:111065. https://doi.org/10.1016/j.nut.2020.111065
Vila L, Puig-Domingo M (2018) The Krakow declaration: The last chance for Europe to eradicate iodine deficiency. Endocrinol Diabetes Nutr 65(10):553–555. https://doi.org/10.1016/j.endinu.2018.10.001
Lazarus JH (2021) Monitoring iodine nutritional status: adults or schoolchildren? J Endocrinol Invest 44(2):383–385. https://doi.org/10.1007/s40618-020-01313-6
De Angelis S, Bagnasco M, Moleti M, Regalbuto C, Tonacchera M, Vermiglio F et al (2021) Obesity and monitoring iodine nutritional status in schoolchildren: Is body mass index a factor to consider? Thyroid 31(5):829–840. https://doi.org/10.1089/thy.2020.0189
Miller V, Singh GM, Onopa J et al (2021) Global Dietary Database 2017: data availability and gaps on 54 major foods, beverages and nutrients among 5.6 million children and adults from 1220 surveys worldwide. BMJ Glob Health 6(2):e003585. https://doi.org/10.1136/bmjgh-2020-003585
Gao M, Chen W, Dong S et al (2021) Assessing the impact of drinking water iodine concentrations on the iodine intake of Chinese pregnant women living in areas with restricted iodized salt supply. Eur J Nutr 60(2):1023–1030. https://doi.org/10.1007/s00394-020-02308-y
Saha S, Abu BAZ, Jamshidi-Naeini Y et al (2019) Is iodine deficiency still a problem in sub-Saharan Africa?: a review. Proc Nutr Soc 78(4):554–566. https://doi.org/10.1017/S0029665118002859
Li S, Zheng Q, Xu J et al (2011) Iodine excess or not: analysis on the necessity of reducing the iodine content in edible salt based on the national monitoring results. Asia Pac J Clin Nutr 20(4):501–506
Kassim IA, Moloney G, Busili A et al (2014) Iodine intake in Somalia is excessive and associated with the source of household drinking water. J Nutr 144(3):375–381. https://doi.org/10.3945/jn.113.176693
Szybiński Z, Jarosz M, Hubalewska-Dydejczyk A et al (2010) Iodine-deficiency prophylaxis and the restriction of salt consumption - a 21st century challenge. Endokrynol Pol 61(1):135–140
Perrine CG, Herrick K, Serdula MK, Sullivan KM (2010) Some subgroups of reproductive age women in the United States may be at risk for iodine deficiency. J Nutr 140(8):1489–1494. https://doi.org/10.3945/jn.109.120147
Watutantrige-Fernando S, Barollo S, Bertazza L et al (2018) Efficacy of educational intervention to improve awareness of the importance of iodine, use of iodized salt, and dietary iodine intake in northeastern Italian schoolchildren. Nutrition 53:134–139. https://doi.org/10.1016/j.nut.2018.02.010
Censi S, Manso J, Barollo S et al (2020) Changing dietary habits in veneto region over two decades: still a long road to go to reach an io-dine-sufficient status. Nutrients 12(8):2399. https://doi.org/10.3390/nu12082399
Torres MT, Vila L, Manresa JM et al (2020) Impact of dietary habit, iodine supplementation and smoking habit on urinary iodine concentration during pregnancy in a catalonia population. Nutrients 12(9):2656. https://doi.org/10.3390/nu12092656
Threapleton DE, Waiblinger D, Snart CJP et al (2021) Prenatal and postpartum maternal iodide intake from diet and supplements, urinary iodine and thyroid hormone concentrations in a region of the united kingdom with mild-to-moderate iodine deficiency. Nutrients 13(1):230. https://doi.org/10.3390/nu13010230
Massad S, Gebre-Medhin M, Dary O et al (2020) Micronutrient status of Palestinian school children following salt and flour fortification: a cross-sectional study. BMC Nutr 6:38. https://doi.org/10.1186/s40795-020-00367-2.eCollection2020
Saborido L, Latres de Rauek B, Rezzónico JN et al (1996) Iodine in school children. Relationship with incidence of goiter, socioeconomic group and salt intake. Medicina (B Aires) 56(5 Pt 1):448–454
Yamada C, Oyunchimeg D, Erdenbat A et al (2000) Estimation of salt intake and recommendation for iodine content in iodized salt in Mongolia. Asia Pac J Public Health 12(1):27–31. https://doi.org/10.1177/101053950001200106
Thomson BM, Vannoort RW, Haslemore RM (2008) Dietary exposure and trends of exposure to nutrient elements iodine, iron, selenium and sodium from the 2003–4 New Zealand Total Diet Survey. Br J Nutr 99(3):614–625. https://doi.org/10.1017/S0007114507812001
Basu S, Stuckler D, Vellakkal S, Ebrahim S (2012) Dietary salt reduction and cardiovascular disease rates in India: a mathematical model. PLoS ONE 7(9):e44037. https://doi.org/10.1371/journal.pone.0044037
Campbell NR, Dary O, Cappuccio FP et al (2012) Need for coordinated programs to improve global health by optimizing salt and iodine intake. Rev Panam Salud Publica 32(4):281–286. https://doi.org/10.1590/s1020-49892012001000006
Ovadia YS, Arbelle JE, Gefel D et al (2017) First israeli national iodine survey demonstrates iodine deficiency among school-aged children and pregnant women. Thyroid 27(8):1083–1091. https://doi.org/10.1089/thy.2017.0251
Al-Dakheel MH, Haridi HK, Al-Bashir BM et al (2018) Assessment of household use of iodized salt and adequacy of salt iodization: a cross-sectional National Study in Saudi Arabia. Nutr J 17(1):35. https://doi.org/10.1186/s12937-018-0343-0
Dold S, Zimmermann MB, Jukic T et al (2018) Universal salt iodization provides sufficient dietary iodine to achieve adequate iodine nutrition during the first 1000 days: a cross-sectional multicenter study. J Nutr 148(4):587–598. https://doi.org/10.1093/jn/nxy015
Vega-Vega O, Fonseca-Correa JI, Mendoza-De la Garza A et al (2018) Contemporary dietary intake: too much sodium, not enough potassium, yet sufficient iodine: The SALMEX cohort results. Nutrients 10(7):816. https://doi.org/10.3390/nu10070816
Powles J, Fahimi S, Micha R et al (2013) Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 3(12):e003733. https://doi.org/10.1136/bmjopen-2013-003733
Elliott P, Brown I (2006) Sodium intakes around the world. Background document prepared for the Forum and Technical meeting on Reducing Salt Intake in Populations. World Health Organization, Paris, France. https://apps.who.int/iris/handle/10665/43738 Accessed 13 Dec. 2021
Olivieri A, Giorgino F, Maffeis C, Bagnasco M (2021) Salt reduction and iodine intake in Italy. J Endocrinol Invest. https://doi.org/10.1007/s40618-021-01708-z
Olivieri A, Trimarchi F, Vitti P (2020) Global iodine nutrition 2020: Italy is an iodine sufficient country. J Endocrinol Invest 43:1671–1672. https://doi.org/10.1007/s40618-020-01402-6
Teti C, Panciroli M, Nazzari E et al (2021) Iodoprophylaxis and thyroid autoimmunity: an update. Immunol Res 69(2):129–138. https://doi.org/10.1007/s12026-021-09192-6
Ruggeri RM, Trimarchi F (2021) Iodine nutrition optimization: are there risks for thyroid autoimmunity? J Endocrionol Invest 44(9):1827–1835. https://doi.org/10.1007/s40618-021-01548-x
https://www.salute.gov.it/portale/documentazione/p6_2_5_1.jsp?lingua=italiano&id=18. Accessed 13 Dec. 2021
UNICEF (2008) Sustainable elimination of iodine deficiency. https://data.unicef.org/resources/sustainable-elimination-of-iodine-deficiency/ Accessed 13 Dec. 2021
GBD 2017 Diet Collaborators (2019) Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 393(10184):1958–1972. https://doi.org/10.1016/S0140-6736(19)30041-8
Acknowledgements
The authors thank Antonella Olivieri* for her helpful comments that improved the manuscript. *Department of Cardiovascular and Endocrine-Metabolic Diseases and Aging, Italian National Institute of Health, Responsible for the Italian National Observatory for Monitoring Iodine Prophylaxis, Rome, Italy.
Funding
No founds, grants, or other support was received for the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: FN, NM and MB; Methodology: DF; Formal analysis and Investigation: FG, MA, FN, LV; Writing—original draft preparation: FN, NM and MB; Writing—review and editing: FG, LV, MA and MB; Supervision, DF, FG and MB. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Diego Ferone has been a speaker for and participated on advisory boards and received research grants from Novartis, Ipsen and Pfizer. Diego Ferone is a member of the Editorial Board of Journal of Endocrinological Investigation. Federico Gatto has been a speaker for Novartis and has participated on advisory boards of Novartis, AMCo Ltd, and IONIS Pharmaceuticals. Diego Ferone and Manuela Albertelli are members of the Editorial Board of the Journal of Endocrinological Investigation. The other Authors have no conflicts of interest to declare.
Ethical approval
This article does not contain any study with human participants and animals performed by any of the authors.
Informed consent
As the present study is a review article no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nista, F., Bagnasco, M., Gatto, F. et al. The effect of sodium restriction on iodine prophylaxis: a review. J Endocrinol Invest 45, 1121–1138 (2022). https://doi.org/10.1007/s40618-022-01749-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01749-y