Abstract
Purpose
To compare the effects of different thyroid screening scenarios, using the universal and targeted high-risk case-finding approaches with different diagnostic tests on the prevalence of subclinical hypothyroidism (SCH), thyroid autoimmunity, and pregnancy outcomes after adjustments for the intervention.
Methods
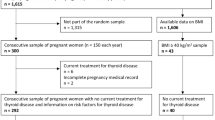
During a secondary analysis of data collected in Tehran Thyroid and Pregnancy Study, a total of 2277 women from the total population, including 1303 high-risk individuals for thyroid dysfunction. The Cochran–Mantel–Haenszel method, adjusted for the intervention, was also used to evaluate the relationships between different screening scenarios [i.e., universal approach using thyroid-stimulating hormone (TSH) and/or thyroid peroxidase antibody (TPOAb) tests and targeted high-risk case-finding approach using TSH and/or TPOAb tests] and pregnancy outcomes (i.e., preterm delivery and NICU admission). The universal approach using both TSH and TPOAb measurements was considered as the reference scenario. We analyzed outcomes of different screening methods in individuals treated with LT4, compared to those individuals who were not treated.
Results
Compared to the universal screening approach with both TSH and TPOAb measurements, the targeted high-risk case-finding approach overlooked approximately 42%, 62%, and 74% of women with elevated TSH (> 4 µlU/mL) when using both TSH and TPOAb tests, TSH alone, and TPO alone, respectively. After adjusting for the missed cases, 2.86% of women with preterm delivery and 2.76% of women with NICU admission were missed when they were screened using the targeted high-risk case-finding approach by measuring both TSH and TPOAb. The percentage of missed cases increased when applying the targeted approach with the TSH test alone, without measuring TPOAb. Overall, 4.16% and 4.02% of women with preterm delivery and NICU admission were overlooked in this scenario, respectively. After adjustments for the intervention, the probability of NICU admission in neonates of mothers, who were screened using the targeted high-risk case-finding approach with TPOAb measurement, was 2.31 folds higher than those screened by the reference scenario.
Conclusion
This study suggests that although the targeted high-risk case-finding approach including both TSH and TPOAb tests, may overlook some women with SCH, it is a reasonable option since it is not associated with a higher risk of adverse pregnancy outcomes.

Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Carney LA, Quinlan JD, West JM (2014) Thyroid disease in pregnancy. Am Fam Physician 89(4):273–278
Negro R, Mestman JH (2011) Thyroid disease in pregnancy. Best Pract Res Clin Endocrinol Metab 25(6):927–943
Karcaaltincaba D, Ozek MA, Ocal N, Calis P, Inan MA, Bayram M (2020) Prevalences of subclinical and overt hypothyroidism with universal screening in early pregnancy. Arch Gynecol Obstet 301:681–686
Dong AC, Stagnaro-Green A (2019) Differences in diagnostic criteria mask the true prevalence of thyroid disease in pregnancy: a systematic review and meta-analysis. Thyroid 29(2):278–289
Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J et al (1999) Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med 341(8):549–555
Negro R, Stagnaro-Green A (2014) Diagnosis and management of subclinical hypothyroidism in pregnancy. BMJ 349:g4929
Casey BM, Thom EA, Peaceman AM, Varner MW, Sorokin Y, Hirtz DG et al (2017) Treatment of subclinical hypothyroidism or hypothyroxinemia in pregnancy. N Engl J Med 376(9):815–825
Yamamoto JM, Benham JL, Nerenberg KA, Donovan LE (2018) Impact of levothyroxine therapy on obstetric, neonatal and childhood outcomes in women with subclinical hypothyroidism diagnosed in pregnancy: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 8(9):e022837
Dhillon-Smith RK, Middleton LJ, Sunner KK, Cheed V, Baker K, Farrell-Carver S et al (2019) Levothyroxine in women with thyroid peroxidase antibodies before conception. N Engl J Med 380(14):1316–1325
Wang H, Gao H, Chi H, Zeng L, Xiao W, Wang Y et al (2017) Effect of levothyroxine on miscarriage among women with normal thyroid function and thyroid autoimmunity undergoing in vitro fertilization and embryo transfer: a randomized clinical trial. JAMA 318(22):2190–2198
Hales C, Taylor PN, Channon S, Paradice R, McEwan K, Zhang L et al (2018) Controlled antenatal thyroid screening II: effect of treating maternal suboptimal thyroid function on child cognition. J Clin Endocrinol Metab 103(4):1583–1591
Springer D, Jiskra J, Limanova Z, Zima T, Potlukova E (2017) Thyroid in pregnancy: from physiology to screening. Crit Rev Clin Lab Sci 54(2):102–116
Taylor PN, Okosieme OE, Premawardhana L, Lazarus JH (2015) Should all women be screened for thyroid dysfunction in pregnancy? Women’s Health 11(3):295–307
Spencer L, Bubner T, Bain E, Middleton P (2015) Screening and subsequent management for thyroid dysfunction pre‐pregnancy and during pregnancy for improving maternal and infant health. Cochrane Database Syst Rev (9):CD011263. https://doi.org/10.1002/14651858.CD011263.pub2
Thangaratinam S, Tan A, Knox E, Kilby MD, Franklyn J, Coomarasamy A (2011) Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence. BMJ 342:d2616
Korevaar TI, Medici M, Visser TJ, Peeters RP (2017) Thyroid disease in pregnancy: new insights in diagnosis and clinical management. Nat Rev Endocrinol 13(10):610–622
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C et al (2017) 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27(3):315–389
Vaidya B, Anthony S, Bilous M, Shields B, Drury J, Hutchison S et al (2007) Detection of thyroid dysfunction in early pregnancy: universal screening or targeted high-risk case finding? J Clin Endocrinol Metab 92(1):203–207
Chang DL, Leung AM, Braverman LE, Pearce EN (2011) Thyroid testing during pregnancy at an academic Boston Area Medical Center. J Clin Endocrinol Metab 96(9):E1452–E1456
Jouyandeh Z, Hasani-Ranjbar S, Qorbani M, Larijani B (2015) Universal screening versus selective case-based screening for thyroid disorders in pregnancy. Springer
Berbara TMBL, Morais NSD, Saraiva DA, Corcino CM, Schtscherbyna A, Moreira KL et al (2020) Selective case finding versus universal screening for detecting hypothyroidism in the first trimester of pregnancy: a comparative evaluation of a group of pregnant women from Rio de Janeiro. Arch Endocrinol Metab 64(2):159–164
Yamamoto JM, Metcalfe A, Nerenberg KA, Khurana R, Chin A, Donovan LE (2020) Thyroid function testing and management during and after pregnancy among women without thyroid disease before pregnancy. CMAJ 192(22):E596–E602
De Groot L, Abalovich M, Alexander EK, Amino N, Barbour L, Cobin RH et al (2012) Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97(8):2543–2565
Lazarus J, Brown RS, Daumerie C, Hubalewska-Dydejczyk A, Negro R, Vaidya B (2014) 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J 3(2):76–94
Obstetricians ACo, Gynecologists (2015) Practice bulletin No. 148: thyroid disease in pregnancy. Obstet Gynecol 125(4):996
Granfors M, Åkerud H, Skogö J, Stridsberg M, Wikström A-K, Sundström-Poromaa I (2014) Targeted thyroid testing during pregnancy in clinical practice. Obstet Gynecol 124(1):10–15
Ahmed IZ, Eid YM, El Orabi H, Ibrahim HR (2014) Comparison of universal and targeted screening for thyroid dysfunction in pregnant Egyptian women. Eur J Endocrinol 171:285–291
Taylor PN, Iqbal A, Minassian C, Sayers A, Draman MS, Greenwood R et al (2014) Falling threshold for treatment of borderline elevated thyrotropin levels—balancing benefits and risks: evidence from a large community-based study. JAMA Intern Med 174(1):32–39
Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, Minooee S, Rahmati M et al (2018) Effects of levothyroxine on pregnant women with subclinical hypothyroidism, negative for thyroid peroxidase antibodies. J Clin Endocrinol Metab 103(3):926–935
Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, Alavi Majd H, Azizi F (2017) Effects of levothyroxine treatment on pregnancy outcomes in pregnant women with autoimmune thyroid disease. Eur J Endocrinol 176(2):253–265
Maraka S, Singh Ospina NM, O’Keeffe DT, Rodriguez-Gutierrez R, Espinosa De Ycaza AE, Wi C-I et al (2016) Effects of levothyroxine therapy on pregnancy outcomes in women with subclinical hypothyroidism. Thyroid 26(7):980–986
Rao M, Zeng Z, Zhao S, Tang L (2018) Effect of levothyroxine supplementation on pregnancy outcomes in women with subclinical hypothyroidism and thyroid autoimmunity undergoing in vitro fertilization/intracytoplasmic sperm injection: an updated meta-analysis of randomized controlled trials. Reprod Biol Endocrinol 16(1):1–9
Nazarpour S, Tehrani FR, Simbar M, Tohidi M, Azizi F (2016) Thyroid and pregnancy in Tehran, Iran: objectives and study protocol. Int J Endocrinol Metab 14(1):1–7
Negro R, Formoso G, Mangieri T, Pezzarossa A, Dazzi D, Hassan H (2006) Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications. J Clin Endocrinol Metab 91(7):2587–2591
Azizi F, Mehran L, Amouzegar A, Delshad H, Tohidi M, Askari S et al (2013) Establishment of the trimester-specific reference range for free thyroxine index. Thyroid 23(3):354–359
Henriksen TB, Baird DD, Olsen J, Hedegaard M, Secher NJ, Wilcox AJ (1997) Time to pregnancy and preterm delivery. Obstet Gynecol 89(4):594–599
Haidari ES, Lee HC, Illuzzi JL, Phibbs CS, Lin H, Xu X (2020) Hospital variation in admissions to neonatal intensive care units by diagnosis severity and category. J Perinatol 41:1–10
Wang W, Teng W, Shan Z, Wang S, Li J, Zhu L et al (2011) The prevalence of thyroid disorders during early pregnancy in China: the benefits of universal screening in the first trimester of pregnancy. Eur J Endocrinol 164(2):263–268
Sitoris G, Veltri F, Kleynen P, Belhomme J, Rozenberg S, Poppe K (2019) Screening for thyroid dysfunction in pregnancy with targeted high-risk case finding: can it be improved? J Clin Endocrinol Metab 104(6):2346–2354
Lazarus JH, Bestwick JP, Channon S, Paradice R, Maina A, Rees R et al (2012) Antenatal thyroid screening and childhood cognitive function. N Engl J Med 366(6):493–501
Negro R, Mangieri T, Coppola L, Presicce G, Casavola EC, Gismondi R et al (2005) Levothyroxine treatment in thyroid peroxidase antibody-positive women undergoing assisted reproduction technologies: a prospective study. Hum Reprod 20(6):1529–1533
Rotondi M, Capelli V, Chiovato L, Nappi RE (2019) 2017 ATA guidelines on the management of thyroid dysfunctions in pregnancy: what do OB/GYNs need to know? Gynecol Endocrinol 35(4):276–279
Yang H, Shao M, Chen L, Chen Q, Yu L, Cai L et al (2014) Screening strategies for thyroid disorders in the first and second trimester of pregnancy in China. PLoS ONE 9(6):e99611
Nielsen C, Lang RS (1999) Principles of screening. Med Clin North Am 83(6):1323–1337
Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R et al (2011) Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid 21(10):1081–1125
Agresti A (2003) Categorical data analysis. Wiley
Acknowledgements
Authors wish to acknowledge the Shahid Beheshti University of Medical Sciences for approval of this project and its supporting as a research grant.
Funding
This project was approved by the Shahid Beheshti University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
MA was involved in study design, literature search, analyzing and interpreting data, manuscript drafting, critical discussion, and revising the manuscript. SN was involved in primary design of the study and data gathering. AS was contributed in statistical analysis, interpreting data, manuscript drafting, and critical discussion. FRT was involved in study design, and critical discussion and revising the manuscript. FA was involved in the study design and critical discussion.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethics approval
The study was approved by the Ethical Committee of the Research Institute for Endocrine Sciences (RIES), and a written informed consent form was obtained from all participants (IR.SBMU.ENDOCRINE.REC.1400.003).
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amiri, M., Nazarpour, S., Ramezani Tehrani, F. et al. The targeted high-risk case-finding approach versus universal screening for thyroid dysfunction during pregnancy: thyroid-stimulating hormone (TSH) and/or thyroid peroxidase antibody (TPOAb) test?. J Endocrinol Invest 45, 1641–1651 (2022). https://doi.org/10.1007/s40618-021-01738-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01738-7