Abstract
Purpose
This study aimed to evaluate the effect and individual responsiveness after 12 (12wk) and 24 weeks (24wk) of physical exercise (PE) and nutritional guidance (NG) on metabolic syndrome (MetS) criteria and hepatic parameters in overweight adolescents.
Methods
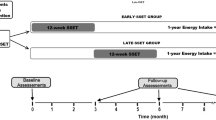
The study comprised 94 overweight adolescents, aged between 10 and 16 years old, from both sexes, allocated into groups: PE and NG (PENGG, n = 64) and control with NG (NGCG, n = 30). Variables were collected at baseline, 12wk, and 24wk. Weight, height, abdominal circumference (AC), blood pressure, and peak oxygen consumption (VO2peak), as well as insulin, triglycerides (TAG), high-density lipoprotein (HDL-c), aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were evaluated. HOMA-IR and QUICKI were calculated. PE session consisted of 45 min of indoor cycling, 45 min of walking, and 20 min of stretching, three times a week. The NG consisted of three collective sessions in the first 12wk. Anova, effect size, and prevalence of responders were used for statistical analysis.
Results
The PENGG12wk reduced anthropometric and metabolic measurements, while increased VO2peak and HDL-c. The PEG24wk promoted anthropometric, blood pressure, metabolic, and VO2peak improvements, but participants without PE returned to pre-exercise status and presented worsening AST and ALT concentrations. Frequencies of respondents in PENGG12wk versus (vs) NGCG12wk were, respectively, AC (69.1% vs 17.6%, p < 0.01), HDL-c (87.2% vs 23.5%, p < 0.01), TAG (67.3% vs 41.7%, p = 0.05) and ALT (45.5% vs 5,9%; p = 0.003).
Conclusion
Interventions with PE were effective to reduce MetS components in 12wk and maintenance in 24wk, showing anthropometric, metabolic, and VO2peak improvements. Higher individual responses were observed in 12wk and in 24wk, important changes in overweight adolescent’s therapy.
Level of evidence
Level I, evidence obtained from well-designed controlled trials randomization.
Trial registration number and date of registration
Brazilian Registry of Clinical Trials (RBR-4v6h7b) and date of registration April 4th, 2020.




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Lobstein T, Jackson-Leach R, Moodie ML et al (2015) Child and adolescent obesity: part of a bigger picture. Lancet 385(9986):2510–2520
Sahoo K, Sahoo B, Choudhury AK et al (2015) Childhood obesity: causes and consequences. J Family Med Prim Care 4(2):187–192
Velfer YA, Philip M, Shalitin S (2019) Increased prevalence of severe obesity and related comorbidities among patients referred to a pediatric obesity clinic during the last decade. Horm Res Paediatr 92(3):169–178
Leite N, Milano GE, Cieslak F et al (2009) Effects of physical exercise and nutritional guidance on metabolic syndrome in obese adolescents. Braz J Phys Ther 13(1):73–81
Nehus E, Mitsnefes M (2019) Childhood obesity and the metabolic syndrome. Pediatr Clin North Am 66(1):31–43
World Health Organization. Physical activity. Available at: https://www.who.int/en/news-room/fact-sheets/detail/physical-activity. Accessed: 06 APR 2020.
Brand C, Martins CMDL, Lemes VB et al (2020) Effects and prevalence of responders after a multicomponent intervention on cardiometabolic risk factors in children and adolescents with overweight/obesity: Action for health study. J Sports Sci 38(6):682–691
Grundy SM (2016) Metabolic syndrome update. Trends Cardiovasc 26(4):364–373
Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365:1415–1428
Coutinho P, Leite N, Lopes WA et al (2015) Association between adiposity indicators, metabolic parameters and inflammatory markers in a sample of female adolescents. Arch Endocrinol Metab 59:325–334
Leite N, Cieslak F, Milano GE et al (2009) Associação entre o perfil lipídico e medidas antropométricas indicadoras de adiposidade em adolescentes. Rev Bras de Cineantropometria e Desempenho Hum 11:127–133
Tozo TA, Pereira BO, Menezes Junior FJ et al (2020) Hypertensive measures in schoolchildren: risk of central obesity and protective effect of moderate-to-vigorous physical activity. Arq Bras Cardiol 115(1):42–49
Milano-Gai GE, Furtado-Alle L, Mota J et al (2018) 12-Week aerobic exercise and nutritional program minimized the presence of the 64Arg allele on insulin resistance. J Pediatr Endocrinol Metab 31(9):1033–1042
Turchiano M, Sweat V, Fierman A et al (2012) Obesity, metabolic syndrome, and insulin resistance in urban high school students of minority race/ethnicity. Arch Pediatr Adolesc Med 166(11):1030–1036
Zuluaga NA, Osorno A, Lozano A et al (2020) Efecto clínico y metabólico de una intervención multidisciplinaria en el marco de un programa de atención integral para niños y adolescentes con obesidad. Biomedica 40(1):166–184
Vasconcellos F, Seabra A, Katzmarzyk PT et al (2014) Physical activity in overweight and obese adolescents: systematic review of the effects on physical fitness components and cardiovascular risk factors. Sports Med 44(8):1139–1152
Lopes WA, Leite N, Silva LR et al (2016) Effects of 12wk of combined training without caloric restriction on inflammatory markers in overweight girls. J Sports Sci 34(20):1902–1912
Bonafiglia JT, Rotundo MP, Whittall JP et al (2016) Inter-individual variability in the adaptive responses to endurance and sprint interval training: A randomized crossover study. PLoS ONE 11(12):e0167790
Alvarez C, Ramírez-Campillo R, Ramírez-Vélez R et al (2017) Effects of 6-weeks high-intensity interval training in schoolchildren with insulin resistance: Influence of biological maturation on metabolic, body composition, cardiovascular and performance non-responses. Front Physiol 29(8):444
Alvarez C, Ramírez-Campillo R, Ramírez-Vélez R et al (2017) Metabolic effects of resistance or high-intensity interval training among glycemic control-nonresponsive children with insulin resistance. Int J Obes 42(1):79–87
Onis M, Onyango AW, Borghi E et al (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85:660–667
Lohmann TAG, Roche AF, Martorell R (1988) Anthropometric standardization reference manual. Human Kinetics Books:177.
Moore SA, McKay HA, MacDonald H, Nettlefold L, Baxter-Jones AD, Cameron N et al (2015) Enhancing a somatic maturity prediction model. Med Sci Sports Exerc 47(8):1755–1764
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Katz A, Nambi SS, Mather K et al (2000) Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85(7):2402–2410
Rowland TW (1990) Exercise and children’s health. Human Kinetics Books, Champaign
Tanaka H, Monahan KD, Seals DR (2001) Age-predicted maximal heart rate revisited. J Am Coll Cardiol 37(1):153–156
Riebe D, Ehrman JK, Liguori G, Magal M (2018) ACSM’s guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer
Karvonen MJ, Kentala E, Mustala O (1957) The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn 35(3):307–315
Cohen J (1988) Statistical power analysis for the behavioral sciences (2.ªed.). Hillsdale: Lawrence Erlbaum Associates.
Hopkins WG (2007) A spreadsheet for deriving a confidence interval, mechanistic inference and clinical inference from a P value. Sportscience 11:16–21
Bianchini JAA, Silva DF, Nardo CCS et al (2013) Multidisciplinary therapy reduces risk factors for metabolic syndrome in obese adolescents. Eur J Pediatr 172(2):215–221
Faria F, Howe C, Faria R et al (2020) Impact of recreational sports activities on metabolic syndrome components in adolescents. Int J Environ Res Public Health 17(1):143
Moser DC, Giuliano ICB, Titski ACK et al (2013) Anthropometric measures and blood pressure in school children. J Pediatr 89(3):243–249
Ighbariya A, Weiss R (2017) Insulin resistance, prediabetes, metabolic syndrome: what should every pediatrician know? J Clin Res Pediatr Endocrinol 9(suppl 2):49–57
Nolan PB, Keeling SM, Robitaille CA et al (2018) The effect of detraining after a period of training on cardiometabolic health in previously sedentary individuals. Int J Environ Res Public Health 15(10):2303
Gonçalves IO, Oliveira PJ, Ascensão A, Magalhães J (2013) Exercise as a therapeutic tool to prevent mitochondrial degeneration in non-alcoholic steatohepatitis. Eur J Clin Invest 43(11):1184–1194
Chen S, Guo X, Yu S, Zhou Y, Li Z, Sun Y (2016) Metabolic syndrome and serum liver enzymes in the general Chinese population. Int J Environ Res Public Health 13(2):223
Wang CL, Liang L, Fu JF, Zou CC, Hong F, Xue JZ, Lu JR, Wu XM (2008) Effect of lifestyle intervention on non-alcoholic fatty liver disease in Chinese obese children. World J Gastroenterol 14(10):1598–1602
Santomauro M, Paoli-Valeri M, Fernández M, Camacho N, Molina Z, Cicchetti R et al (2012) Hígado graso no alcohólico y su asociación con variables clínicas y bioquímicas en niños y adolescentes obesos: Efecto de un año de intervención en el estilo de vida. Endocrinol Nutr 59(6):346–353
Reinehr T, Schmidt C, Toschke AM, Andler W (2009) Lifestyle intervention in obese children with nonalcoholic fatty liver disease: 2-Year follow-up study. Arch Dis Child 94(6):437–442
Schwimmer JB, McGreal N, Deutsch R, Finegold MJ, Lavine JE (2005) Influence of gender, race, and ethnicity on suspected fatty liver in obese adolescents. Pediatrics 115(5):e561–e565
Polyzos SA, Kountouras J, Mantzoros CS (2016) Adipose tissue, obesity and non-alcoholic fatty liver disease. Minerva Endocrinol 42(2):92–108
Temple JL, Cordero P, Li J, Nguyen V, Oben JA (2016) A guide to non-alcoholic fatty liver disease in childhood and adolescence. Int J Mol Sci 17(6):947
Stevanović J, Beleza J, Coxito P, Ascensão A, Magalhães J (2020) Physical exercise and liver “fitness”: Role of mitochondrial function and epigenetics-related mechanisms in non-alcoholic fatty liver disease. Mol Metab 32:1–14
Kanwar P, Kowdley KV (2016) A síndrome metabólica e sua influência na esteatohepatite não alcoólica. Clin Liver Dis 20:225–243
Myers J, Kokkinos P, Nyelin E (2019) Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients 11(7):1652
Al-Mallah MH, Sakr S, Al-Qunaibet A (2018) Cardiorespiratory fitness and cardiovascular disease prevention: an update. Curr Atheroscler Rep 20(1):1
Funding
This work and authors were supported by Brazilian funding agencies: CAPES, CNPq and Araucaria Foundation-PR/SESA-PR/CNPq/MS-Decit (edital CP 01/2016). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) Finance Code 001. JM was supported by grants: FCT: SFRH/BSAB/142983/2018 and UID/DTP/00617/2019 as well as Santander University Program (2018).
Author information
Authors and Affiliations
Contributions
The manuscript was written by NL, MCT, PRPC, FJMJ and MECC, as well as revised and edited by NL, MCT, ARG, CB, JM and RBR. Conceptualization/design: NL and RBR; methodology: NL and RBR; investigation: NL, GEMG and WAL; supervision/oversight: NL, GEMG and WAL; funding acquisition: NL, PRPC, MCT and JM; data curation: NL, MCT, PRPC, MECC and FJMJ; formal analysis: NL, MCT, PRPC, MECC and FJMJ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interests. The authors declare that they do not have professional relationships with companies or manufacturers that will benefit from the results of this study. The results of the present study do not constitute endorsement of the product by the authors or the NSCA.
Ethics approval
The study protocol has been approved by the Ethics committee of the Hospital de Clinics of the Federal University of Paraná (n.2460.067/2011–03-UFPR).
Informed consent
Parents and/or guardians and adolescents signed the terms of consent for participation in the research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leite, N., Tadiotto, M.C., Corazza, P.R.P. et al. Responsiveness on metabolic syndrome criteria and hepatic parameters after 12 weeks and 24 weeks of multidisciplinary intervention in overweight adolescents. J Endocrinol Invest 45, 741–752 (2022). https://doi.org/10.1007/s40618-021-01699-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01699-x