Abstract
Objective
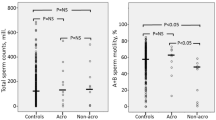
To investigate the changes in semen quality and bioavailable testosterone concentrations in acromegalic male patients according to their disease activity and compare them with patients with non-functional pituitary adenoma (NFA) and healthy controls (HC).
Methods
Twenty-four acromegalic patients with active disease, 22 acromegalic patients in remission, 10 HCs, and 10 patients with NFA were included.
Results
Total and calculated bioavailable testosterone concentrations were lower in patients with pituitary disease. Patients with acromegaly had more severely impaired total testosterone levels and semen parameters in comparison to HCs and patients with NFA. The degree of impairment was more prominent in acromegalic patients with active disease than acromegalic patients in remission. Acromegalic patients in remission had residual impairments in both semen quality and testosterone concentrations. Patients with NFA had the lowest concentrations of calculated bioavailable testosterone, followed by acromegalic patients with active disease and acromegalic patients in remission. Increasing growth hormone (GH) levels were found to be associated with both more severely impaired semen quality and androgen concentrations.
Conclusion
Growth hormone hypersecretion can disturb reproductive biology and thereof semen quality. The reduction in semen quality and androgen levels may not fully recover upon disease control. Clinicians should be aware of the increased risk of impaired semen parameters and reduced total/bioavailable levels in acromegalic patients, especially in the setting of active disease.



Similar content being viewed by others
References
Melmed S (2006) Acromegaly. N Engl J Med 355:2558–2573
Chen Z, Yu Y, He M et al (2019) Higher growth hormone levels are associated with erectile dysfunction in male patients with acromegaly. Endocr Pract 25:562–571
Andreassen M, Juul A, Feldt-Rasmussen U, Jørgensen N (2020) Semen quality in hypogonadal acromegalic patients. Pituitary 23:160–166
Lavrentaki A, Paluzzi A, Wass JA, Karavitaki N (2017) Epidemiology of acromegaly: review of population studies. Pituitary 20:4–9
Vilar L, Vilar CF, Lyra R et al (2017) Acromegaly: clinical features at diagnosis. Pituitary 20:22–32
Katznelson L, Atkinson J, Cook D et al (2011) American Association of Clinical Endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of acromegaly-2011 update. Endocr Pract 17:1–44
Lotti F, Rochira V, Pivonello R et al (2015) Erectile dysfunction is common among men with acromegaly and is associated with morbidities related to the disease. J Sex Med 12:1184–1193
Bartke A, Cecim M, Tang K et al (1994) Neuroendocrine and reproductive consequences of overexpression of growth hormone in transgenic mice. Proc Soc Exp Biol Med 206:345–359
Ml G, Salenave S, Young J, Chanson P (2010) Female gonadal function before and after treatment of acromegaly. J Clin Endocrinol Metab 95:4518–4525
Melmed S, Colao A, Barkan A et al (2009) Guidelines for acromegaly management: an update. J Clin Endocrinol Metab 94:1509–1517
Rosén T, Johannsson G, Johansson J-O, Bengtsson B-Å (1995) Consequences of growth hormone deficiency in adults and the benefits and risks of recombinant human growth hormone treatment. Horm Res Paediatr 43:93–99
Colao A, De Rosa M, Pivonello R et al (2002) Short-term suppression of GH and IGF-I levels improves gonadal function and sperm parameters in men with acromegaly. J Clin Endocrinol Metab 87:4193–4197
Mathews L, Enberg B, Norstedt G (1989) Regulation of rat growth hormone receptor gene expression. J Biol Chem 264:9905–9910
Spiteri-Grech J, Nieschlag E (1992) The role of growth hormone and insulin-like growth factor I in the regulation of male reproductive function. Horm Res Paediatr 38:22–27
Bartke A, Chandrashekar V, Turyn D et al (1999) Effects of growth hormone overexpression and growth hormone resistance on neuroendocrine and reproductive functions in transgenic and knock-out mice2. Proc Soc Exp Biol Med 222:113–123
Melmed S (2017) Acromegaly. In: The pituitary. 4rd edn. Elsevier, pp 423–466
Bhasin S, Cunningham GR, Hayes FJ et al (2010) Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 95:2536–2559
Vermeulen A, Verdonck L, Kaufman JM (1999) A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 84:3666–3672
Cao X-W, Lin K, Li C-Y, Yuan C-W (2011) A review of WHO Laboratory manual for the examination and processing of human semen. Zhonghua Nan Ke Xue 17:1059–1063
Andreassen M, Juul A, Feldt-Rasmussen U, Jørgensen N (2018) Semen quality in patients with pituitary disease and adult-onset hypogonadotropic hypogonadism. Endocr Connect 7:523–533
Zhou WJ, Ma SC, Zhao M, Liu C, Guan X-D, Bao Z-S, Jia G-J, Jia W (2018) Risk factors and the prognosis of sexual dysfunction in male patients with pituitary adenomas: a multivariate analysis. Asian J Androl 20:43
Buvat J (2003) Hyperprolactinemia and sexual function in men: a short review. Int J Impot Res 15:373–377
Magon N, Singh S, Saxena A, Sahay R (2011) Growth hormone in male infertility. Indian J Endocrinol Metab 15(Suppl 3):S248–249
Pedersen SA, Jørgensen JO, Christiansen JS et al (1988) Fertility and semen quality in previously growth hormone treated men. Pediatr Res 23:120–120
Monzani ML, Pederzoli S, Volpi L et al (2021) Sexual dysfunction: a neglected and overlooked issue in adult GH deficiency: the management of AGHD study. J Endocrine Society 5:bvab002
Borland K, Mita M, Oppenheimer C et al (1984) The actions of insulin-like growth factors I and II on cultured Sertoli cells. Endocrinology 114:240–246
Carani C, Granata AR, De Rosa M et al (1999) The effect of chronic treatment with GH on gonadal function in men with isolated GH deficiency. Eur J Endocrinol 140:224–230
Hull K, Harvey S (2000) Growth hormone: roles in male reproduction. Endocrine 13:243–250
Naville D, Chatelain P, Avallet O, Saez J (1990) Control of production of insulin-like growth factor I by pig Leydig and Sertoli cells cultured alone or together. Cell-cell interactions. Mol Cell Endocrinol 70:217–224
Figueiredo MA, Fernandes RV, Studzinski AL et al (2013) GH overexpression decreases spermatic parameters and reproductive success in two-years-old transgenic zebrafish males. Anim Reprod Sci 139:162–167
Froment P, Staub C, Hembert SP et al (2004) Reproductive abnormalities in human insulin-like growth factor-binding protein-1 transgenic male mice. Endocrinology 145:2080–2091
Sjögren I, Jönsson M, Madej A et al (1998) Effects of very high doses of human growth hormone (hGH) on the male reproductive system in the dog. Andrologia 30:37–42
Zhang B, Shozu M, Okada M et al (2010) Insulin-like growth factor I enhances the expression of aromatase P450 by inhibiting autophagy. Endocrinology 151:4949–4958
Piotrowska K, Sluczanowska-Glabowska S, Kucia M et al (2015) Histological changes of testes in growth hormone transgenic mice with high plasma level of GH and insulin-like growth factor-1. Folia Histochem Cytobiol 53:249–258
Rosa CE, Figueiredo MA, Lanes CFC et al (2008) Metabolic rate and reactive oxygen species production in different genotypes of GH-transgenic zebrafish. Comp Biochem Physiol B Biochem Mol Biol 149:209–214
Katznelson L, Kleinberg D, Vance ML et al (2001) Hypogonadism in patients with acromegaly: data from the multi-centre acromegaly registry pilot study. Clin Endocrinol 54:183–188
Bartke A (2000) Effects of growth hormone review on male reproductive functions. J Androl 21:181–188
Harman SM, Metter EJ, Tobin JD et al (2001) Longitudinal effects of aging on serum total and free testosterone levels in healthy men. J Clin Endocrinol Metab 86:724–731
Feldman HA, Longcope C, Derby CA et al (2002) Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab 87:589–598
Ashok S, Sigman M (2007) Bioavailable testosterone should be used for the determination of androgen levels in infertile men. J Urol 177:1443–1446
Kaltsas G, Mukherjee J, Jenkins P et al (1999) Menstrual irregularity in women with acromegaly. J Clin Endocrinol Metab 84:2731–2735
de Ronde W, van der Schouw YT, Pols HA et al (2006) Calculation of bioavailable and free testosterone in men: a comparison of 5 published algorithms. Clin Chem 52:1777–1784
Qin J, Su Q-Q, Wang D et al (2015) Cabergoline reduces serum luteinizing hormone and sperm quality in male Rattus losea. Pak J Zool 47(3):831–838
Fombonne J, Csaba Z, Von Boxberg Y et al (2003) Expression of somatostatin receptor type-2 (sst2A) in immature porcine Leydig cells and a possible role in the local control of testosterone secretion. Reprod Biol Endocrinol 1:19
Aurich JE, Kranski S, Parvizi N, Aurich C (2003) Somatostatin treatment affects testicular function in stallions. Theriogenology 60:163–174
Acknowledgements
The study was supported by the Research Fund of the Istanbul University-Cerrahpasa, Istanbul, Turkey, project number TTU-2017-27077.
Funding
The study was supported by the Research Fund of the Istanbul University, Istanbul, Turkey, project number TTU-2017-27077.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, and/or acquisition of data, and/or analysis and interpretation of data; participated in drafting the article or revising it critically for important intellectual content, and gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yilmaz, M.K., Sulu, C., Ozkaya, H.M. et al. Evaluation of sex hormone profile and semen parameters in acromegalic male patients. J Endocrinol Invest 44, 2799–2808 (2021). https://doi.org/10.1007/s40618-021-01593-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01593-6