Abstract
Purpose
Brain tumors are the most common solid tumor in children. The prevalence of survivors from these cancers has been increasing, presenting endocrine sequelae in more than 40% of the cases. Our aim was to characterize the endocrinopathies diagnosed in this population, exploring the outcomes of growth hormone treatment.
Methods
We have performed a retrospective analysis of the survivors that were followed-up through a close protocol at our endocrine late-effects clinic.
Results
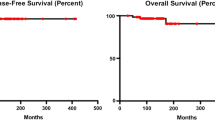
242 survivors, followed during 6.4 (0–23.4) years, were considered. The median age at tumor diagnosis was 6.7 (0–18) years and pilocytic astrocytoma was the most frequent neoplasm (33.5%). The prevalence of endocrinopathies was of 71.5%, with growth hormone deficiency being the most frequent (52.9%). An indirect correlation between the age at the beginning of somatropin and growth velocity in the first year of treatment was observed. Those treated with craniospinal radiotherapy presented a smaller final upper/lower segments ratio comparing with those that only received cranial radiotherapy. However, their final height was not compromised when compared to their family height target. We found pubertal delay in 12%; accelerated/precocious puberty in 13.2%; central and primary hypogonadism in 21.9% and 3.3%, respectively; primary and central hypothyroidism in 23.6% and 14.5%, respectively; thyroid nodules in 7.4%; ACTH deficiency in 10.3% and diabetes insipidus in 12%.
Conclusion
This study reveals a higher prevalence of endocrinopathies in brain tumors survivors and explores the influence of craniospinal irradiation in the adult body proportions. It reinforces the importance of routine follow-up among survivors.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Turner CD, Rey-casserly C, Liptak CC, Chordas C (2009) Late effects of therapy for pediatric brain tumor survivors. J Child Neurol 24:1455–1463. https://doi.org/10.1177/0883073809341709
Saha A, Salley CG, Saigal P, Rolnitzky L, Goldberg J, Scott S et al (2014) Late effects in survivors of childhood CNS tumors treated on head start I and II protocols. Pediatr Blood Cancer 61:1644–1672. https://doi.org/10.1002/pbc.25064
Chemaitilly W, Li Z, Huang S, Ness KK, Clark KL, Green DM et al (2015) Anterior hypopituitarism in adult survivors of childhood cancers treated with cranial radiotherapy: a report from the St Jude lifetime cohort study. J Clin Oncol 33:492–500. https://doi.org/10.1200/JCO.2014.56.7933
Aslan IR, Cheung CC (2014) Early and late endocrine effects in pediatric central nervous system diseases. J Pediatr Rehabil Med 7:281–294. https://doi.org/10.3233/PRM-140299
Seland M, Bjoro T, Furre T, Schreiner T, Bollerslev J, Fosså SD et al (2015) Hormonal dysfunction is frequent in cancer survivors treated with radiotherapy to the head and neck region. J Cancer Surviv 9:630–640. https://doi.org/10.1007/s11764-015-0439-x
Chemaitilly W, Armstrong GT, Gajjar A, Hudson MM (2016) Hypothalamic-pituitary axis dysfunction in survivors of childhood CNS tumors: importance of systematic follow-up and early endocrine consultation. J Clin Oncol 34:4315–4319. https://doi.org/10.1200/JCO.2016.70.1847
Vatner RE, Niemierko A, Misra M, Weyman EA, Goebel CP, Ebb DH et al (2018) Endocrine deficiency as a function of radiation dose to the hypothalamus and pituitary in pediatric and young adult patients with brain tumors. J Clin Oncol 36:2854–2862. https://doi.org/10.1200/JCO.2018.78.1492
Clement SC, Meeteren SM, Boot AM, Grinten HLC, Granzen B, Han KS et al (2016) Prevalence and risk factors of early endocrine disorders in childhood brain tumor survivors: a nationwide, multicenter study. J Clin Oncol 34:4362–4370. https://doi.org/10.1200/JCO.2016.67.5025
Lawson SA, Horne VE, Golekoh MC, Hornung L, Burns K, Fouladi M, Rose S (2019) Hypothalamic—pituitary function following childhood brain tumors: analysis of prospective annual endocrine screening. Pediatr Blood Cancer. https://doi.org/10.1002/pbc.27631
Grimberg A, Divall SA, Polychrnakos C, Allen DB, Cohen LE, Quintos JB et al (2016) Guidelines for growth hormone and insulin-like growth factor-I treatment in children and adolescents: growth hormone deficiency, idiopathic short stature, and primary insulin-like growth factor-I deficiency. Horm Res Paediatr 86:361–397. https://doi.org/10.1159/000452150
Chemaitilly W, Sklar CA (2018) Childhood cancer treatments and associated endocrine late effects: a concise guide for the pediatric endocrinologist. Horm Res Paediatr 9:74–82. https://doi.org/10.1159/000493943
Dewire M, Green DM, Sklar CA, Merchant TE, Wallace D, Lin T, Vern-Gross T et al (2015) Pubertal development and primary ovarian insufficiency in female survivors of embryonal brain tumors following risk-adapted craniospinal irradiation and adjuvant chemotherapy. Pediatr Blood Cancer 62:329–334. https://doi.org/10.1002/pbc.25274
Louis DN, Perry A, Reifenberger G, Deimling A, Figarella-Branger D, Cavenee WK et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Childrens Oncology Group (2018) Long-Term Follow-up Guidelines for Survivors Childhood, Adolescent and Young Adult Cancers. www.survivorshipguidelines.org
Lazar L, Pertzelan A, Weintrob N, Phillip M, Kauli R (2015) Sexual precocity in boys: accelerated versus slowly progressive puberty gonadotropin-suppressive therapy and final height. J Clin Endocrinol Metab 86:4127–4132. https://doi.org/10.1210/jcem.86.9.7852
Lazar L, Kauli R, Pertzelan A, Phillip M (2015) Gonadotropin-suppressive therapy in girls with early and fast puberty affects the pace of puberty but not total pubertal growth or final height. J Clin Endocrinol Metab 87:2090–2094. https://doi.org/10.1210/jcem.87.5.8481
Laughton SJ, Merchant TE, Sklar CA, Kun LE, Fouladi M, Broniscer A et al (2015) Endocrine outcomes for children with embryonal brain tumors after risk-adapted craniospinal and conformal primary-site irradiation and high-dose chemotherapy with stem-cell rescue on the SJMB-96 Trial. J Clin Oncol 26:1112–1118. https://doi.org/10.1200/JCO.2008.13.5293
Gan H, Phipps K, Aquilina K, Gaze MN, Hayward R, Spoudeas HA (2015) Neuroendocrine morbidity after pediatric optic gliomas: a longitudinal analysis of 166 children over 30 years. J Clin Endocrinol Metab 100:3787–3799. https://doi.org/10.1210/jc.2015-2028
Armstrong GT, Conklin HM, Huang S, Srivastava D, Sanford R, Ellison DW et al (2011) Survival and long-term health and cognitive outcomes after low-grade glioma. Neuro oncol 13:223–234. https://doi.org/10.1093/neuonc/noq178
Spoudeas HA, Charmandari E, Brook CGD (2003) Hypothalamo-pituitary-adrenal axis integrity after cranial irradiation for childhood posterior fossa tumours. Med Pediatr Oncol 40:224–229. https://doi.org/10.1002/mpo.10267
Shalitin S, Gai M, Goshen Y, Cohen I, Yaniv I, Phillip M (2011) Endocrine outcome in long-term survivors of childhood brain tumors. Horm Res Paediatr 76:113–122. https://doi.org/10.1159/000327584
Gleeson HK, Shalet SM (2004) The impact of cancer therapy on the endocrine system in survivors of childhood brain tumours. Endocr Relat Cancer 11:589–602. https://doi.org/10.1677/erc.1.00779
Lerner SE, Huang GJM, McMahon D, Sklar CA, Oberfield SE (2015) Growth hormone therapy in children after cranial/craniospinal radiation therapy: sexually dimorphic outcomes. JCEM 89:6100–6104. https://doi.org/10.1210/jc.2004-1515
Beckers D, Thomas M, Jamart J, Francois I, Maes M, Lebrethn MC et al (2010) Adult final height after GH therapy for irradiation-induced GH deficiency in childhood survivors of brain tumors: the Belgian experience. Eur J Endocrinol. https://doi.org/10.1530/EJE-09-0690
Clayton PE, Shalet SM (1991) The evolution of spinal growth after irradiation. Clin Oncol 1991:220–222. https://doi.org/10.1016/s0936-6555(05)80744-7
Spoudeas HA (2002) Growth and endocrine function after chemotherapy and radiotherapy in childhood. Eur J Cancer 38:1748–1759. https://doi.org/10.1016/s0959-8049(02)00169-7
Chemaitilly W, Merchant T, Li Z, Barnes N, Amstrong G, Ness K et al (2016) Central precocious puberty following the diagnosis and treatment of pediatric cancer and central nervous system tumors: presentation and long-term outcomes. Clin Endocrinol 84:361–371. https://doi.org/10.1111/cen.12964
Rohrer TR, Beck JD, Grabenbauer GG, Fahlbusch R, Buchfelder M, Dörr HG (2009) Late endocrine sequelae after radiotherapy of pediatric brain tumors are independent of tumor location. J Endocrinol Invest 32:294–297. https://doi.org/10.1007/BF03345714
Acknowledgements
We thank Dr. Sofia Nunes, Dr. João Passos, and Dr. Duarte Salgado from our center’s Pediatric Neurology Department and Dr. Cátia Pedro from our center’s Radiotherapy Department for their constant collaboration with the Endocrinology Department.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no multiplicity of interests to disclose.
Ethical approval
This study complies with the Declaration of Helsinki and was approved by our ethical committee. The data were anonymized and the authors have followed the protocols of their work center on the publication of data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maciel, J., Dias, D., Cavaco, D. et al. Growth hormone deficiency and other endocrinopathies after childhood brain tumors: results from a close follow-up in a cohort of 242 patients. J Endocrinol Invest 44, 2367–2374 (2021). https://doi.org/10.1007/s40618-021-01541-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01541-4