Abstract
Purpose
International guidelines recommend salivary cortisol for the diagnosis of Cushing’s syndrome. Despite mass spectrometry-based assays are considered the analytical gold-standard, there is still the need to define reference intervals and diagnostic accuracy of such methodology.
Methods
100 healthy volunteers and 50 consecutive patients were enrolled to compare LC–MS/MS and electrochemiluminescence assay for the determination of late-night salivary cortisol and cortisone. Moreover, we aimed to determine reference intervals of salivary steroids in a population of healthy individuals and diagnostic accuracy in patients with suspected hypercortisolism and in a population including also healthy individuals.
Results
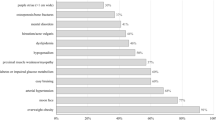
Method comparison highlighted a positive bias (51.8%) of immunoassay over LC–MS/MS. Reference intervals of salivary cortisol (0.17–0.97 µg/L), cortisone (0.84–4.85 µg/L) and ratio (0.08–0.30) were obtained. The most accurate thresholds of salivary cortisol for the diagnosis of hypercortisolism were 1.15 µg/L in the population with suspected hypercortisolism (AUC 1) and 1.30 µg/L in the population including also healthy individuals (AUC 1). Cut-off values of salivary cortisone (7.23 µg/L; Se 92.9%, Sp 97.2%, AUC 0.960 and Se 92.9%, Sp 99.1%, AUC 0.985 in suspected hypercortisolism and in overall population, respectively) and cortisol-to-cortisone ratio (0.20; Se 85.7%, Sp 80.6%, AUC 0.820 and Se 85.7%, Sp 85.5%, AUC 0.855 in suspected hypercortisolism and in overall population, respectively) were accurate and similar in both populations.
Conclusion
LC–MS/MS is the most accurate analytical platform for measuring salivary steroids. Obtained reference intervals are coherent with previously published data and diagnostic accuracy for diagnosis of overt hypercortisolism proved highly satisfactory.



Similar content being viewed by others
References
Newell-Price J, Bertagna X, Grossman AB, Nieman LK (2006) Cushing’s syndrome. Lancet (Lond Engl) 367:1605–1617
Tirabassi G, Boscaro M, Arnaldi G (2014) Harmful effects of functional hypercortisolism: a working hypothesis. Endocrine 46:370–386
Findling JW, Raff H (2001) Diagnosis and differential diagnosis of Cushing’s syndrome. Endocrinol Metab Clin North Am 30:729–747
Nieman LK (2018) Recent updates on the diagnosis and management of Cushing’s syndrome. Endocrinol Metab (Seoul, Korea) 33:139–146
Pivonello R, Isidori AM, De Martino MC, Newell-Price J, Biller BMK, Colao A (2016) Complications of Cushing’s syndrome: state of the art. Lancet Diabetes Endocrinol 4:611–629
Dekkers OM, Horváth-Puh́o E, Jørgensen JOL, Cannegieter SC, Ehrenstein V, Vandenbroucke JP, Pereira AM, Srøensen HT (2013) Multisystem morbidity and mortality in Cushing’s syndrome: a cohort study. J Clin Endocrinol Metab 98:2277–2284
Clayton RN, Raskauskiene D, Reulen RC, Jones PW (2011) Mortality and morbidity in Cushing’s disease over 50 Years in Stoke-on-Trent, UK: audit and meta-analysis of literature. J Clin Endocrinol Metab 96:632–642
Nieman L, Biller B, Findling J, Newell-Price J, Savage M, Stewart P, Montori VM (2008) The diagnosis of Cushing’s syndrome: an endocrine society clinical practice guideline. Clin Endocrinol Metab 95:1526–1540
Chiappin S, Antonelli G, Gatti R, De Palo EF (2007) Saliva specimen: a new laboratory tool for diagnostic and basic investigation. Clin Chim Acta 383:30–40
Tateishi Y, Kouyama R, Mihara M, Doi M, Yoshimoto T, Hirata Y (2012) Evaluation of salivary cortisol measurements for the diagnosis of subclinical Cushing’s syndrome. Endocr J 59:283–289
Perogamvros I, Keevil BG, Ray DW, Trainer PJ, Tateishi Y, Kouyama R, Mihara M, Doi M, Yoshimoto T, Hirata Y et al (2007) Saliva specimen: a new laboratory tool for diagnostic and basic investigation. Endocr J 95:4951–4958
Carroll T, Raff H, Findling JW (2009) Late-night salivary cortisol for the diagnosis of Cushing syndrome: a meta -analysis. Endocr Pract 15:335–342
Elias PCL, Martinez EZ, Barone BFC, Mermejo LM, Castro M, Moreira AC (2014) Late-night salivary cortisol has a better performance than urinary free cortisol in the diagnosis of Cushing’s syndrome. J Clin Endocrinol Metab 99:2045–2051
Belaya ZE, Iljin AV, Melnichenko GA, Rozhinskaya LY, Dragunova NV, Dzeranova LK, Butrova SA, Troshina EA, Dedov II (2012) Diagnostic performance of late-night salivary cortisol measured by automated electrochemiluminescence immunoassay in obese and overweight patients referred to exclude Cushing’s syndrome. Endocrine 41:494–500
Erickson D, Singh RJ, Sathananthan A, Vella A, Bryant SC (2012) Late-night salivary cortisol for diagnosis of Cushing’s syndrome by liquid chromatography/tandem mass spectrometry assay. Clin Endocrinol (Oxf) 76:467–472
Raff H (2013) Update on late-night salivary cortisol for the diagnosis of Cushing’s syndrome: methodological considerations. Endocrine 44:346–349
Galm BP, Qiao N, Klibanski A, Biller BMK, Tritos NA (2020) Accuracy of laboratory tests for the diagnosis of Cushing’s syndrome. J Clin Endocrinol Metab 26:979–993
Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM (2016) Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the European network for the study of adrenal tumors. Eur J Endocrinol 175:G1–G34
Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, Irwig L, Levine D, Reitsma JB, De Vet HCW et al (2016) STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 6:1–17
Badrick E, Kirschbaum C, Kumari M (2007) The relationship between smoking status and cortisol secretion. J Clin Endocrinol Metab 92:819–824
Hansen ÅM, Garde AH, Persson R (2008) Sources of biological and methodological variation in salivary cortisol and their impact on measurement among healthy adults: A review. Scand J Clin Lab Invest 68:448–458
Antonelli G, Padoan A, Aita A, Sciacovelli L, Plebani M (2017) Verification of examination procedures in clinical laboratory for imprecision, trueness and diagnostic accuracy according to ISO 15189:2012: a pragmatic approach. Clin Chem Lab Med 55:1501–1508
Öner M, Kocakoç ID (2017) JMASM 49: A compilation of some popular goodness of fit tests for normal distribution: their algorithms and MATLAB codes (MATLAB). J Mod Appl Stat Methods 16:547–575
FDA F, DA (2018) Bioanalytical method validation guidance. Food Drug Adm 1043:25
Monaghan PJ, Keevil BG, Trainer PJ (2013) The use of mass spectrometry to improve the diagnosis and the management of the HPA axis. Rev Endocr Metab Disord 14:143–157
Aberle J, Schulze zur Wiesch C, Flitsch J, Veigel J, Schön G, Jung R, Reining F, Lautenbach A, Rotermund R, Riedel N (2018) Specificity of late-night salivary cortisol measured by automated electrochemiluminescence immunoassay for Cushing’s disease in an obese population. J Endocrinol Invest 41:1325–1331
Ceccato F, Marcelli G, Martino M, Concettoni C, Brugia M, Trementino L, Michetti G, Arnaldi G (2019) The diagnostic accuracy of increased late night salivary cortisol for Cushing’s syndrome: a real-life prospective study. J Endocrinol Invest 42:327–335
Raff H, Findling JW (2010) Biomarkers: salivary cortisol or cortisone? Nat Rev Endocrinol 6:658–660
Van den Ouweland JMW, Kema IP (2012) The role of liquid chromatography-tandem mass spectrometry in the clinical laboratory. J Chromatogr B Anal Technol Biomed Life Sci 883–884:18–32
Kushnir MM, Rockwood AL, Roberts WL, Yue B, Bergquist J, Meikle AW (2011) Liquid chromatography tandem mass spectrometry for analysis of steroids in clinical laboratories. Clin Biochem 44:77–88
Grimes DA, Schulz KF (2002) Uses and abuses of screening tests. Lancet 359:881–884
Antonelli G, Ceccato F, Artusi C, Marinova M, Plebani M (2015) Salivary cortisol and cortisone by LC-MS/MS: validation, reference intervals and diagnostic accuracy in Cushing’s syndrome. Clin Chim Acta 451:247–251
Baid SK, Sinaii N, Wade M, Rubino D, Nieman LK (2007) Radioimmunoassay and tandem mass spectrometry measurement of bedtime salivary cortisol levels: a comparison of assays to establish hypercortisolism. J Clin Endocrinol Metab 92:3102–3107
Turpeinen U, Välimäki MJ, Hämäläinen E (2009) Determination of salivary cortisol by liquid chromatography-tandem mass spectrometry. Scand J Clin Lab Invest 69:592–597
Kurdi Zerikly R, Amiri L, Faiman C, Gupta M, Singh RJ, Nutter B, Kennedy L, Hatipoglu B, Weil RJ, Hamrahian AH (2010) Diagnostic characteristics of late-night salivary cortisol using liquid chromatography-tandem mass spectrometry. J Clin Endocrinol Metab 95:4555–4559
Bäcklund N, Brattsand G, Israelsson M, Ragnarsson O, Burman P, Engström BE, Høybye C, Berinder K, Wahlberg J, Olsson T et al (2020) Reference intervals of salivary cortisol and cortisone and their diagnostic accuracy in Cushing’s syndrome. Eur J Endocrinol 182:569–582
Sturmer LR, Dodd D, Chao CS, Shi RZ (2018) Clinical utility of an ultrasensitive late night salivary cortisol assay by tandem mass spectrometry. Steroids 129:35–40
Mészáros K, Karvaly G, Márta Z, Magda B, Tőke J, Szücs N, Tóth M, Rácz K, Patócs A (2018) Diagnostic performance of a newly developed salivary cortisol and cortisone measurement using an LC–MS/MS method with simple and rapid sample preparation. J Endocrinol Invest 41:315–323
Palmieri S, Morelli V, Polledri E, Fustinoni S, Mercadante R, Olgiati L, Eller Vainicher C, Cairoli E, Zhukouskaya VV, Beck-Peccoz P et al (2013) The role of salivary cortisol measured by liquid chromatographytandem mass spectrometry in the diagnosis of subclinical hypercortisolism. Eur J Endocrinol 168:289–296
Ceccato F, Barbot M, Zilio M, Ferasin S, Occhi G, Daniele A, Mazzocut S, Iacobone M, Betterle C, Mantero F et al (2013) Performance of salivary cortisol in the diagnosis of Cushing’s syndrome, adrenal incidentaloma, and adrenal insufficiency. Eur J Endocrinol 169:31–36
Ceccato F, Barbot M, Zilio M, Ferasin S, De Lazzari P, Lizzul L, Boscaro M, Scaroni C (2015) Age and the metabolic syndrome affect salivary cortisol rhythm: data from a community sample. Hormones 14:392–398
Raff H (2012) Cushing’s syndrome: diagnosis and surveillance using salivary cortisol. Pituitary 15:64–70
Nunes ML, Vattaut S, Corcuff JB, Rault A, Loiseau H, Gatta B, Valli N, Letenneur L, Tabarin A (2009) Late-night salivary cortisol for diagnosis of overt and subclinical Cushing’s syndrome in hospitalized and ambulatory patients. J Clin Endocrinol Metab 94:456–462
Funding
The study was supported by a grant from the University of Turin. The funding sources had no role in the study design, data collection and analysis, manuscript preparation, or decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
F.S., F.P. had the idea and, together with M.P.C., performed the data analysis and the manuscript writing. F.R., A.N., M.R., E.A., G.P. and S.V. collected the biomaterial and performed the analyses for each patient. L.A. verified the analytical methods and supervised the manuscript drafting. R.G. and G.M. were in charge for overall direction and planning. E.A. and E.G. gave the needed encouragement and support to investigate and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Institutional Ethics Committee.
Informed consent
Written informed consent was obtained from all enrolled patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ponzetto, F., Settanni, F., Parasiliti-Caprino, M. et al. Reference ranges of late-night salivary cortisol and cortisone measured by LC–MS/MS and accuracy for the diagnosis of Cushing’s syndrome. J Endocrinol Invest 43, 1797–1806 (2020). https://doi.org/10.1007/s40618-020-01388-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01388-1