Abstract
Objective
We aimed at defining the most effective routine immunoassay- or liquid chromatography-tandem mass spectrometry (LC–MS/MS)-determined steroid biomarkers for identifying non-classic adrenal hyperplasia due to 21-hydroxylase deficiency (21-NCAH) in a PCOS-like population before genotyping.
Methods
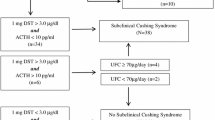
Seventy PCOS-like patients in reproductive age with immunoassay-determined follicular 17OH-progesterone (17OHP) ≥ 2.00 ng/mL underwent CYP21A2 gene analysis and 1–24ACTH test. Serum steroids were measured by immunoassays at baseline and 60 min after ACTH stimulation; basal steroid profile was measured by LC–MS/MS.
Results
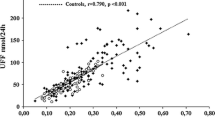
Genotyping revealed 23 21-NCAH, 15 single allele heterozygous CYP21A2 mutations (21-HTZ) and 32 PCOS patients displaying similar clinical and metabolic features. Immunoassays revealed higher baseline 17OHP and testosterone, and after ACTH stimulation, higher 17OHP (17OHP60) and lower cortisol, whereas LC–MS/MS revealed higher 17OHP (17OHPLC-MS/MS), progesterone and 21-deoxycortisol and lower corticosterone in 21-NCAH compared with both 21-HTZ and PCOS patients. Steroid thresholds best discriminating 21-NCAH from 21-HTZ and PCOS were estimated, and their diagnostic accuracy in identifying 21-NCAH from PCOS was established by ROC analysis. The highest accuracy was observed for 21-deoxycortisol ≥ 0.087 ng/mL, showing 100% sensitivity, while the combination of 17OHPLC-MS/MS ≥ 1.79 ng/mL and corticosterone ≤ 8.76 ng/mL, as well as the combination of ACTH-stimulated 17OHP ≥ 6.77 ng/mL and cortisol ≤ 240 ng/mL by immunoassay, showed 100% specificity.
Conclusions
LC–MS/MS measurement of basal follicular 21-deoxycortisol, 17OHP and corticosterone seems the most convenient method for diagnosing 21-NCAH in a population of PCOS with a positive first level screening, providing high accuracy and reducing the need for ACTH stimulation test.

Similar content being viewed by others
References
Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, Welt CK, Endocrine Society (2013) Diagnosis and treatment of polycystic ovary syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 98:4565–4592
Pasquali R, Diamanti-Kandarakis E, Gambineri A (2016) Secondary polycystic ovary syndrome: theoretical and practical aspects. Eur J Endocrinol 175:R157–R169
The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod 2004(19):41–47
Pall M, Azziz R, Beires J, Pignatelli D (2010) The phenotype of hirsute women: a comparison of polycystic ovary syndrome and 21-hydroxylase-deficient nonclassic adrenal hyperplasia. Fertil Steril 94:684–689
Chanukvadze D, Kristesashvili J, Kvashilava N (2012) Correlation of biochemical markers and clinical signs of hyperandrogenism in women with polycystic ovary syndrome (PCOS) and women with non-classic congenital adrenal hyperplasia (NCAH). Iran J Reprod Med 10:307–314
Pignatelli D (2013) Non-classic adrenal hyperplasia due to the deficiency of 21-hydroxylase and its relation to polycystic ovarian syndrome. Front Horm Res 40:158–170
Speiser PW, White PC (1998) Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency. Clin Endocrinol (Oxf) 49:411–417
Pignatelli D, Macut D, Pfeifer M, Yildiz BO, Diamanti-Kandarakis E (2013) Polycystic ovary syndrome: novel insights into causes and therapy. Front Horm Res. 40:158–170
Speiser PW, Arlt W, Auchus RJ, Baskin LS, Conway GS, Merke DP, Meyer-Bahlburg HFL, Miller WL, Murad MH, Oberfield SE, White PC (2018) Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 103:4043–4088
Azziz R, Zacur HA (1989) 21-Hydroxylase deficiency in female hyperandrogenism: screening and diagnosis. J Clin Endocrinol Metab 69:577–584
Azziz R, Hincapie LA, Knochenhauer ES, Dewailly D, Fox L, Boots LR (1999) Screening for 21-hydroxylase-deficient non classic adrenal hyperplasia among hyperandrogenic women: a prospective study. Fertil Steril 72:915–925
Escobar-Morreale HF, Sanchón R, San Millán JL (2008) A prospective study of the prevalence of nonclassical congenital adrenal hyperplasia among women presenting with hyperandrogenic symptoms and signs. J Clin Endocrinol Metab 93:527–533
Ambroziak U, Kepczyńska-Nik A, Kurylwicz A, Malunowicz EM, Wójcicka A, Miśkiewicz P, Macech M (2016) The diagnosis of non classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency, based on serum basal or post-ACTH stimulation 17-hydroxyprogesterone, can lead to false-positive diagnosis. Clin Endocrinol 84:23–29
New MI, Lorenzen F, Lerner AJ, Kohn B, Oberfield SE, Pollack MS, Dupont B, Stoner E, Levy DJ, Pang S, Levine LS (1983) Genotyping steroid 21-hydroxylase deficiency: hormonal reference data. J Clin Endocrinol Metab 57:320–326
Dewailly D, Vantyghem-Haudiquet MC, Sainsard C, Buvat J, Cappoen JP, Ardaens K, Racadot A, Lefebvre J, Fossati P (1986) Clinical and biological phenotypes in late-onset 21-hydroxylase deficiency. J Clin Endocrinol Metab 63:418–423
Wedell A, Thilen A, Ritzen EM, Stengler B, Luthman H (1994) Mutational spectrum of the steroid 21-hydroxylase gene in Sweden: implications for genetic diagnosis and association with disease manifestations. J Clin Endocrinol Metab 78:1145–1152
Witchel SF, Lee PA (1998) Identification of heterozygotic carriers of 21-hydroxylase deficiency: sensitivity of ACTH stimulation tests. Am J Med Genet 76:337–342
Napolitano E, Manieri C, Restivo F, Composto E, Lanfranco F, Repici M, Pasini B, Einaudi S, Menegatti E (2011) Correlation between genotype and hormonal levels in heterozygous mutation carriers and noncarriers of 21-hydroxylase deficiency. J Endocrinol Invest 34:498–501
Ketha SS, Singh RJ, Ketha H (2017) Role of mass spectrometry in clinical endocrinology. Endocrinol Metab Clin North Am 46:593–613
Final Report National Institute of Health. Evidence-based Methodology Workshop on Polycystic Ovary Syndrome, 3–5 December 2012. Excecutive summary at: https://prevention.nih.gov/workshos/2012/pcos/resourc-es.aspx.
Keefe CC, Goldman MM, Zhang K, Clarke N, Reitz RE, Welt CK (2014) Simultaneous measurement of thirteen steroid hormones in women with polycystic ovary syndrome and control women using liquid chromatography–tandem mass spectrometry. PLoS ONE 9:e93805
Pasquali R, Zanotti L, Fanelli F, Mezzullo M, Fazzini A, Morselli Labate AM, Repaci A, Ribichini D, Gambineri A (2016) Defining hyperandrogenism in women with polycystic ovary syndrome: a challenging perspective. J Clin Endocrinol Metab 101:2013–2022
Fanelli F, Belluomo I, Di Lallo VD, Cuomo G, De Iasio R, Baccini M, Casadio E, Casetta B, Vicennati V, Gambineri A, Grossi G, Pasquali R, Pagotto U (2011) Serum steroid profiling by isotopic dilution-liquid chromatography–mass spectrometry: comparison with current immunoassays and reference intervals in healthy adults. Steroids 76:244–253
Fiet J, Le Bouc Y, Guéchot J, Hélin N, Maubert M-A, Farabos D, Lamazière A (2017) A liquid chromatography/tandem mass spectometry profile of 16 serum steroids, including 21-deoxycortisol and management of congenital adrenal hyperplasia. J Endocr Soc 1:186–201
Menabò S, Polat S, Baldazzi L, Kulle AE, Holterhus P-M, Grötzinger J, Fanelli F, Balsamo A, Riepe FG (2014) Congenital adrenal hyperplasia due to 11-beta-hydroxylase deficiency: functional consequences of four CYP11B1 mutations. Eur J Hum Genet 22:610–616
Kulle AE, Riepe FG, Hedderich J, Sippell WG, Schmitz J, Niermeyer L, Holterhus PM (2015) LC-MS/MS based determination of basal- and ACTH-stimulated plasma concentrations of 11 steroid hormones: implications for detecting heterozygote CYP21A2 mutation carriers. Eur J Endocrinol 173:517–524
Conway GS, Dewailly D, Diamanti-Kandarakis E, Escobar Morreale H, Franks S, Gambineri A, Kelestimur F, Macut D, Micic D, Pasquali R, Pfeifer M, Pignatelli D, Pugeat M, Yildiz B (2014) The polycystic ovary syndrome: an endocrinological perspective from the European Society of Endocrinology. Eur J Endocrinol 171:P1–P29
Yildiz BO, Bolour S, Woods K, Moore A, Azziz R (2010) Visually scoring hirsutism. Hum Reprod Update 16:51–64
Ludwig E (1977) Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol 97:247–254
Burke BM, Cunliffe WJ (1984) The assessment of acne vulgaris—the Leeds technique. Br J Dermatol 111:83–92
Burke JP, Hale DE, Hazuda HP, Stern MP (1999) A quantitative scale of acanthosis nigricans. Diabetes Care 22:1655–1659
WHO 1997 Preventing and Managing the Global Epidemic. Report of a WHO consultation on obesity. WHO/NUT/NCD/98.1 World Health Organization, Geneva
Pasquali R, Patton L, Pocognoli P, Cognigni GE, Gambineri A (2007) 17-Hydroxyprogesterone responses to gonadotropin-releasing hormone disclose distinct phenotypes of functional ovarian hyperandrogenism and polycystic ovary syndrome. J Clin Endocrinol Metab 92:4208–4217
Vermeulen A, Verdonck L, Kaufman JM (1999) A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 84:3666–3672
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Di Dalmazi G, Fanelli F, Mezzullo M, Casadio E, Rinaldi E, Garelli S, Giampalma E, Mosconi C, Golfieri R, Vicennati V, Pagotto U, Pasquali R (2015) Steroid profiling by LC-MS/MS in nonsecreting and subclinical cortisol-secreting adrenocortical adenomas. J Clin Endocrinol Metab 100:3529–3538
Barbaro M, Lajic S, Baldazzi L, Balsamo A, Pirazzoli P, Cicognani A, Wedell A, Cacciari E (2004) Functional analysis of two recurrent amino acid substitutions in the CYP21 gene from Italian patients with congenital adrenal hyperplasia. J Clin Endocrinol Metab 89:2402–2407
Simonetti L, Bruque CD, Fernández CS, Benavides-Mori B, Delea M, Kolomenski JE, Espeche LD, Buzzalino ND, Nadra AD, Dain L (2018) CYP21A2 mutation update: comprehensive analysis of databases and published genetic variants. Hum Mutat. 39:5–22
Morán C, Tapia MC, Hernández E, Vázquez G, García-Hernández E, Bermúdez JA (1994) Etiological review of hirsutism in 250 patients. Arch Med Res 25:311–314
Zargar AH, Wani AI, Masoodi SR, Laway BA, Bashir MI, Salahuddin M (2002) Epidemiologic and etiologic aspects of hirsutism in Kashmiri women in the Indian subcontinent. Fertil Steril 77:674–678
Ambroziak U, Kępczyńska-Nyk A, Kuryłowicz A, Wysłouch-Cieszyńska A, Małunowicz EM, Bartoszewicz Z, Kondracka A, Jaźwiec R, Pawłowska E, Szcześniak M, Dadlez M, Bednarczuk T (2015) LC-MS/MS improves screening towards 21-hydroxylase deficiency. Gynecol Endocrinol 31:296–300
Moran C, Azziz R (2003) 21-hydroxylase-deficient nonclassic adrenal hyperplasia: the great pretender. Semin Reprod Med 21:295–300
Azziz R, Dewailly D, Owerbach D (1994) Clinical review 56: nonclassic adrenal hyperplasia: current concepts. J Clin Endocrinol Metab 78:810–815
Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO (2004) The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab 89:2745–2749
Escobar-Morreale HF, San Millán JL, Smith RR, Sancho J, Witchel SF (1999) The presence of the 21-hydroxylase deficiency carrier status in hirsute women: phenotype–genotype correlations. Fertil Steril 72:629–638
Admoni O, Israel S, Lavi I, Gur M, Tenenbaum-Rakover Y (2006) Hyperandrogenism in carriers of CYP21 mutations: the role of genotype. Clin Endocrinol (Oxf) 64:645–651
Costa-Barbosa FA, Tonetto-Fernandes VF, Carvalho VM, Nakamura OH, Moura V, Bachega TA, Vieira JG, Kater CE (2010) Superior discriminating value of ACTH-stimulated serum 21-deoxycortisol in identifying heterozygote carriers for 21-hydroxylase deficiency. Clin Endocrinol (Oxf) 73:700–706
Acknowledgement
We thank Adrian Wallwork for English language revision.
Funding
This study was supported by the Emilia Romagna-Region, Alessandro Liberati Young Researcher Grant (Grant No. PRUA 1-2012-004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study was approved by the independent ethical committee of Azienda Ospedaliero-Unversitaria of Bologna, Policlinico S. Orsola-Malpighi
Informed consent
All subjects gave their written informed consent before inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oriolo, C., Fanelli, F., Castelli, S. et al. Steroid biomarkers for identifying non-classic adrenal hyperplasia due to 21-hydroxylase deficiency in a population of PCOS with suspicious levels of 17OH-progesterone. J Endocrinol Invest 43, 1499–1509 (2020). https://doi.org/10.1007/s40618-020-01235-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01235-3