Abstract
Purpose
Graves’ disease (GD) can present as an isolated disease (iGD) or in association with other autoimmune diseases (aGD). The aim of this study, performed in two Endocrine referral centers settled in different geographical areas of Italy, was to compare the anthropometric, clinical, and biochemical phenotype of iGD patients with that of the aGD ones.
Methods
Clinical history, physical examination data, serum levels of TSH, FT4, FT3, thyroglobulin (TgAb), thyroid-peroxidase (TPOAb) and TSH-receptor (TRAb) antibody, presence of Graves’ orbitopathy (GO), and thyroid ultrasound examination at disease diagnosis were recorded.
Results
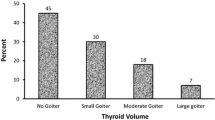
68 aGD and 136 iGD patients were consecutively recruited. At diagnosis, aGD and iGD patients did not differ for F/M ratio, age at presentation, thyroid function parameters, serum levels of TRAb, TgAb, TPOAb, presence of GO, and thyroid volume. The serum levels of TRAb were strongly correlated with the circulating concentrations of both FT3 (ρ = 0.667; p < 0.0001) and FT4 (ρ = 0.628; p < 0.001) in iGD patient, but not in the aGD ones (FT3: ρ = 0.231; p = 0.058; FT4: ρ = 0.096; p = 0.435). Compared with iGD patients, the aGD ones displayed a higher rate of transition from the previous hypothyroidism to hyperthyroidism (χ2 = 6.375; p = 0.012).
Conclusion
Despite similar anthropometric, clinical, and biochemical features at diagnosis, aGD patients display a higher rate of transition from a thyroid functional status to the other as compared with iGD patients.

Similar content being viewed by others
References
Brent GA (2008) Clinical practice. Graves’ disease. N Engl J Med 358(24):2594–2605. https://doi.org/10.1056/NEJMcp0801880
Weetman AP (2000) Graves’ disease. N Engl J Med 343(17):1236–1248. https://doi.org/10.1056/NEJM200010263431707
Bartalena L (2013) Diagnosis and management of Graves disease: a global overview. Nat Rev Endocrinol 9(12):724–734. https://doi.org/10.1038/nrendo.2013.193
Bartalena L, Fatourechi V (2014) Extrathyroidal manifestations of Graves’ disease: a 2014 update. J Endocrinol Invest 37(8):691–700. https://doi.org/10.1007/s40618-014-0097-2
Bartalena L, Masiello E, Magri F et al (2016) The phenotype of newly diagnosed Graves’ disease in Italy in recent years is milder than in the past: results of a large observational longitudinal study. J Endocrinol Invest 39(12):1445–1451. https://doi.org/10.1007/s40618-016-0516-7
Struja T, Kaeslin M, Boesiger F et al (2017) External validation of the GREAT score to predict relapse risk in Graves’ disease: results from a multicenter, retrospective study with 741 patients. Eur J Endocrinol 176(4):413–419. https://doi.org/10.1530/EJE-16-0986
Liu J, Fu J, Xu Y, Wang G (2017) Antithyroid drug therapy for Graves’ disease and implications for recurrence. Int J Endocrinol 2017:3813540. https://doi.org/10.1155/2017/3813540
Marinò M, Latrofa F, Menconi F, Chiovato L, Vitti P (2015) Role of genetic and non-genetic factors in the etiology of Graves’ disease. J Endocrinol Invest 38(3):283–294. https://doi.org/10.1007/s40618-014-0214-2
Rotondi M, Capelli V, Coperchini F et al (2018) Post-partum and non-post-partum relapsing Graves’ hyperthyroidism display different response to anti-thyroid drugs. Eur J Endocrinol 178(6):589–594. https://doi.org/10.1530/EJE-17-1063
Rotondi M, Cappelli C, Pirali B et al (2008) The effect of pregnancy on subsequent relapse from Graves’ disease after a successful course of antithyroid drug therapy. J Clin Endocrinol Metab 93(10):3985–3988. https://doi.org/10.1210/jc.2008-0966
Neufeld M, Maclaren N, Blizzard R (1980) Autoimmune polyglandular syndromes. Pediatr Ann 9(4):154–162
Husebye ES, Anderson MS, Kämpe O (2018) Autoimmune polyendocrine syndromes. N Engl J Med 378(26):2543–2544. https://doi.org/10.1056/NEJMc1805308
Ruggeri RM, Trimarchi F, Giuffrida G et al (2017) Autoimmune comorbidities in Hashimoto’s thyroiditis: different patterns of association in adulthood and childhood/adolescence. Eur J Endocrinol 176(2):133–141. https://doi.org/10.1530/EJE-16-0737
Boelaert K, Newby PR, Simmonds MJ et al (2010) Prevalence and relative risk of other autoimmune diseases in subjects with autoimmune thyroid disease. Am J Med 123(2):183.e181–183.e189. https://doi.org/10.1016/j.amjmed.2009.06.030
Ferrari SM, Fallahi P, Ruffilli I et al (2019) The association of other autoimmune diseases in patients with Graves’ disease (with or without ophthalmopathy): review of the literature and report of a large series. Autoimmun Rev 18(3):287–292. https://doi.org/10.1016/j.autrev.2018.10.001
Neumann WL, Coss E, Rugge M, Genta RM (2013) Autoimmune atrophic gastritis–pathogenesis, pathology and management. Nat Rev Gastroenterol Hepatol 10(9):529–541. https://doi.org/10.1038/nrgastro.2013.101
Mueller RB, Schiff M, Kaegi T et al (2015) The new 2010 ACR/EULAR criteria as predictor of clinical and radiographic response in patients with early arthritis. Clin Rheumatol 34(1):51–59. https://doi.org/10.1007/s10067-014-2737-5
Mosca M, Tani C, Vagnani S, Carli L, Bombardieri S (2014) The diagnosis and classification of undifferentiated connective tissue diseases. J Autoimmun 48–49:50–52. https://doi.org/10.1016/j.jaut.2014.01.019
Taïeb A, Picardo M, Members V (2007) The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res 20(1):27–35. https://doi.org/10.1111/j.1600-0749.2006.00355.x
Bai JC, Fried M, Corazza GR et al (2013) World Gastroenterology Organisation global guidelines on celiac disease. J Clin Gastroenterol 47(2):121–126. https://doi.org/10.1097/MCG.0b013e31827a6f83
Miyakis S, Lockshin MD, Atsumi T et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4(2):295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Ludgate M, Emerson CH (2008) Metamorphic thyroid autoimmunity. Thyroid 18(10):1035–1037. https://doi.org/10.1089/thy.2008.1551
Osorio-Salazar C, Lecomte P, Madec AM, Baulieu JL (1994) Basedow disease following autoimmune primary hypothyroidism. Apropos of 7 cases. Ann Endocrinol (Paris) 55(5):185–189
Kamath C, Young S, Kabelis K et al (2012) Thyrotrophin receptor antibody characteristics in a woman with long-standing Hashimoto’s who developed Graves’ disease and pretibial myxoedema. Clin Endocrinol (Oxf) 77(3):465–470. https://doi.org/10.1111/j.1365-2265.2012.04397.x
Takeda K, Takamatsu J, Kasagi K et al (1988) Development of hyperthyroidism following primary hypothyroidism: a case report with changes in thyroid-related antibodies. Clin Endocrinol (Oxf) 28(4):341–344
Chung YH, Ou HY, Wu TJ (2004) Development of hyperthyroidism following primary hypothyroidism: a case report. Kaohsiung J Med Sci 20(4):188–191. https://doi.org/10.1016/S1607-551X(09)70105-6
McLachlan SM, Rapoport B (2013) Thyrotropin-blocking autoantibodies and thyroid-stimulating autoantibodies: potential mechanisms involved in the pendulum swinging from hypothyroidism to hyperthyroidism or vice versa. Thyroid 23(1):14–24. https://doi.org/10.1089/thy.2012.0374
Champion B, Gopinath B, Ma G, El-Kaissi S, Wall JR (2008) Conversion to Graves’ hyperthyroidism in a patient with hypothyroidism due to Hashimoto’s thyroiditis documented by real-time thyroid ultrasonography. Thyroid 18(10):1135–1137. https://doi.org/10.1089/thy.2008.0142
Furqan S, Haque NU, Islam N (2014) Conversion of autoimmune hypothyroidism to hyperthyroidism. BMC Res Notes 7:489. https://doi.org/10.1186/1756-0500-7-489
Gupta Y, Singh S, Ammini AC (2012) Development of Graves’ disease after long-standing hypothyroidism on treatment, with acute toxicity to thionamides and lithium. BMJ Case Rep. https://doi.org/10.1136/bcr-2012-006433
Bell PM, Sinnamon DG, Smyth PP et al (1985) Hyperthyroidism following primary hypothyroidism in association with polyendocrine autoimmunity. Acta Endocrinol (Copenh) 108(4):491–497
Cho BY, Shong YK, Lee HK, Koh CS, Min HK (1989) Graves’ hyperthyroidism following primary hypothyroidism: sequential changes in various activities of thyrotropin receptor antibodies. Acta Endocrinol (Copenh) 120(4):447–450
Takasu N, Yamada T, Sato A et al (1990) Graves’ disease following hypothyroidism due to Hashimoto’s disease: studies of eight cases. Clin Endocrinol (Oxf) 33(6):687–698
Gonzalez-Aguilera B, Betea D, Lutteri L et al (2018) Conversion to Graves disease from Hashimoto thyroiditis: a study of 24 patients. Arch Endocrinol Metab 62(6):609–614. https://doi.org/10.20945/2359-3997000000086
Wasniewska M, Corrias A, Arrigo T et al (2010) Frequency of Hashimoto’s thyroiditis antecedents in the history of children and adolescents with graves’ disease. Horm Res Paediatr 73(6):473–476. https://doi.org/10.1159/000313395
Aversa T, Lombardo F, Corrias A, Salerno M, De Luca F, Wasniewska M (2014) In young patients with Turner or Down syndrome, Graves’ disease presentation is often preceded by Hashimoto’s thyroiditis. Thyroid 24(4):744–747. https://doi.org/10.1089/thy.2013.0452
Mortensen KH, Cleemann L, Hjerrild BE et al (2009) Increased prevalence of autoimmunity in Turner syndrome–influence of age. Clin Exp Immunol 156(2):205–210. https://doi.org/10.1111/j.1365-2249.2009.03895.x
Pellegrini FP, Marinoni M, Frangione V et al (2012) Down syndrome, autoimmunity and T regulatory cells. Clin Exp Immunol 169(3):238–243. https://doi.org/10.1111/j.1365-2249.2012.04610.x
Chiovato L, Larizza D, Bendinelli G et al (1996) Autoimmune hypothyroidism and hyperthyroidism in patients with Turner’s syndrome. Eur J Endocrinol 134(5):568–575
Morshed SA, Davies TF (2015) Graves’ disease mechanisms: the role of stimulating, blocking, and cleavage region TSH receptor antibodies. Horm Metab Res 47(10):727–734. https://doi.org/10.1055/s-0035-1559633
Evans M, Sanders J, Tagami T et al (2010) Monoclonal autoantibodies to the TSH receptor, one with stimulating activity and one with blocking activity, obtained from the same blood sample. Clin Endocrinol (Oxf) 73(3):404–412. https://doi.org/10.1111/j.1365-2265.2010.03831.x
Chiovato L, Fiore E, Vitti P et al (1998) Outcome of thyroid function in Graves’ patients treated with radioiodine: role of thyroid-stimulating and thyrotropin-blocking antibodies and of radioiodine-induced thyroid damage. J Clin Endocrinol Metab 83(1):40–46. https://doi.org/10.1210/jcem.83.1.4492
Kasagi K, Hidaka A, Endo K et al (1993) Fluctuating thyroid function depending on the balance between stimulating and blocking types of TSH receptor antibodies: a case report. Thyroid 3(4):315–318. https://doi.org/10.1089/thy.1993.3.315
Kraiem Z, Baron E, Kahana L, Sadeh O, Sheinfeld M (1992) Changes in stimulating and blocking TSH receptor antibodies in a patient undergoing three cycles of transition from hypo to hyper-thyroidism and back to hypothyroidism. Clin Endocrinol (Oxf) 36(2):211–214
Wood LC, Ingbar SH (1979) Hypothyroidism as a late sequela in patient with Graves’ disease treated with antithyroid agents. J Clin Invest 64(5):1429–1436. https://doi.org/10.1172/JCI109601
Tamai H, Kasagi K, Takaichi Y et al (1989) Development of spontaneous hypothyroidism in patients with Graves’ disease treated with antithyroidal drugs: clinical, immunological, and histological findings in 26 patients. J Clin Endocrinol Metab 69(1):49–53. https://doi.org/10.1210/jcem-69-1-49
Shigemasa C, Mitani Y, Taniguchi S et al (1990) Three patients who spontaneously developed persistent hypothyroidism during or following treatment with antithyroid drugs for Graves’ hyperthyroidism. Arch Intern Med 150(5):1105–1109
Funding
This paper was not supported by any grant or funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Formal approval by the ethical committee was not required in accordance with the Italian regulation for non-interventional (observational) retrospective studies concerning human beings (AIFA Guidelines for Observational Studies, see www.AIFA.gov).
Informed consent
All patients signed an informed consent concerning the future use of their clinic data for research purposes and data collected remained strictly confidential and anonymous, according to the ethical rules of our Hospital institutions and to the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rotondi, M., Virili, C., Pinto, S. et al. The clinical phenotype of Graves’ disease occurring as an isolated condition or in association with other autoimmune diseases. J Endocrinol Invest 43, 157–162 (2020). https://doi.org/10.1007/s40618-019-01094-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-019-01094-7