Abstract
Purpose
The concept of testosterone (T) supplementation (TS) as a new anti-obesity medication in men with testosterone deficiency syndrome (TDS) is emerging. Data from placebo-controlled trials are more conflicting. The aim of this study is to systematically review and meta-analyze available observational and register studies reporting data on body composition in studies on TS in TDS.
Methods
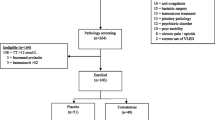
An extensive MEDLINE, Embase, and Cochrane search was performed including the following words: “testosterone” and “body composition.” All observational studies comparing the effect of TS on body weight and other body composition and metabolic endpoints were considered.
Results
Out of 824 retrieved articles, 32 were included in the study enrolling 4513 patients (mean age 51.7 ± 6.1 years). TS was associated with a time-dependent reduction in body weight and waist circumference (WC). The estimated weight loss and WC reduction at 24 months were −3.50 [−5.21; −1.80] kg and −6.23 [−7.94; −4.76] cm, respectively. TS was also associated with a significant reduction in fat and with an increase in lean mass as well as with a reduction in fasting glycemia and insulin resistance. In addition, an improvement of lipid profile (reduction in total cholesterol as well as of triglyceride levels and an improvement in HDL cholesterol levels) and in both systolic and diastolic blood pressure was observed.
Conclusions
Present data support the view of a positive effect of TS on body composition and on glucose and lipid metabolism. In addition, a significant effect on body weight loss was observed, which should be confirmed by a specifically designed RCT.




Similar content being viewed by others
References
Dietz WH, Baur LA, Hall K, Puhl RM, Taveras EM, Uauy R et al (2015) Management of obesity: improvement of health-care training and systems for prevention and care. Lancet 385:2521–2533
Corona G, Rastrelli G, Filippi S, Vignozzi L, Mannucci E, Maggi M (2014) Erectile dysfunction and central obesity: an Italian perspective. Asian J Androl 16:581–591
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, INTERHEART Study Investigators et al (2005) Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case–control study. Lancet 366:1640–1649
Corona G, Rastrelli G, Morelli A, Vignozzi L, Mannucci E, Maggi M (2011) Hypogonadism and metabolic syndrome. J Endocrinol Investig 34:557–567
Corona G, Vignozzi L, Sforza A, Mannucci E, Maggi M (2015) Obesity and late-onset hypogonadism. Mol Cell Endocrinol 418:120–133
Brand JS, Rovers MM, Yeap BB, Schneider HJ, Tuomainen TP, Haring R et al (2014) Testosterone, sex hormone-binding globulin and the metabolic syndrome in men: an individual participant data meta-analysis of observational studies. PLoS ONE 9:e100409
Rastrelli G, Corona G, Mannucci E, Maggi M (2015) Vascular and chronological age in subjects with erectile dysfunction: a cross-sectional study. J Sex Med 12:2303–2312
Iglesias P, Prado F, Macías MC, Guerrero MT, Muñoz A, Ridruejo E et al (2014) Hypogonadism in aged hospitalized male patients: prevalence and clinical outcome. J Endocrinol Invest 37:135–141
Calderón B, Gómez-Martín JM, Vega-Piñero B, Martín-Hidalgo A, Galindo J, Luque-Ramírez M et al (2016) Prevalence of male secondary hypogonadism in moderate to severe obesity and its relationship with insulin resistance and excess body weight. Andrology 4:62–67
Rastrelli G, Corona G, Mannucci E, Maggi M (2016) Vascular and chronological age in men with erectile dysfunction: a longitudinal study. J Sex Med 13(2):200–208
Corona G, Rastrelli G, Vignozzi L, Mannucci E, Maggi M (2012) How to recognize late-onset hypogonadism in men with sexual dysfunction. Asian J Androl 14:251–259
Saad F, Aversa A, Isidori AM, Gooren LJ (2012) Testosterone as potential effective therapy in treatment of obesity in men with testosterone deficiency: a review. Curr Diabetes Rev 8:131–143
Zarotsky V, Huang MY, Carman W, Morgentaler A, Singhal PK, Coffin D et al (2014) Systematic literature review of the risk factors, comorbidities, and consequences of hypogonadism in men. Andrology 2:819–834
Isidori AM, Balercia G, Calogero AE, Corona G, Ferlin A, Francavilla S et al (2015) Outcomes of androgen replacement therapy in adult male hypogonadism: recommendations from the Italian society of endocrinology. J Endocrinol Investig 38:103–112
Maneschi E, Morelli A, Filippi S, Cellai I, Comeglio P, Mazzanti B et al (2012) Testosterone treatment improves metabolic syndrome-induced adipose tissue derangements. J Endocrinol 215:347–362
Saad F, Gooren L, Haider A, Yassin A (2007) An exploratory study of the effects of 12 month administration of the novel long-acting testosterone undecanoate on measures of sexual function and the metabolic syndrome. Arch Androl 53:353–357
Saad F, Gooren LJ, Haider A, Yassin A (2008) A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl 29:102–105
Saad F, Haider A, Doros G, Traish A (2013) Long-term treatment of hypogonadal men with testosterone produces substantial and sustained weight loss. Obesity 21:1975–1981 (Silver Spring)
Francomano D, Lenzi A, Aversa A (2014) Effects of five-year treatment with testosterone undecanoate on metabolic and hormonal parameters in ageing men with metabolic syndrome. Int J Endocrinol 2014:527470
Yassin DJ, Doros G, Hammerer PG, Yassin AA (2014) Long-term testosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters and improves metabolic syndrome and health-related quality of life. J Sex Med 11:1567–1576
Zitzmann M, Saad F, Kliesch S (2014) Long-term treatment with testosterone undecanoate injections leads to sustained weight loss and improvement of metabolic syndrome parameters in 381 hypogonadal men. J Sex Med 11(Suppl. 1):7
Haider A, Saad F, Doros G, Gooren L (2014) Hypogonadal obese men with and without diabetes mellitus type 2 lose weight and show improvement in cardiovascular risk factors when treated with testosterone: an observational study. Obes Res Clin Pract 8:e339–e349
Traish AM, Haider A, Doros G, Saad F (2014) Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study. Int J Clin Pract 68:314–329
Saad F, Yassin A, Doros G, Haider A (2016) Effects of long-term treatment with testosterone on weight and waist size in 411 hypogonadal men with obesity classes I-III: observational data from two registry studies. Int J Obes 40:162–170
Corona G, Maseroli E, Maggi M (2014) Injectable testosterone undecanoate for the treatment of hypogonadism. Expert Opin Pharmacother 15:1903–1926
Neff KJ, le Roux CW (2013) Bariatric surgery: a best practice article. J Clin P athol 66:90–98
Corona G, Giagulli VA, Maseroli E, Vignozzi L, Aversa A, Zitzmann M, Saad F, Mannucci E, Maggi M (2016) THERAPY OF ENDOCRINE DISEASE: testosterone supplementation and body composition: results from a meta-analysis study. Eur J Endocrinol 174(3):R99–R116
Cohen AT, Goto S, Schreiber K, Torp-Pedersen C (2015) Why do we need observational studies of everyday patients in the real-life setting? Eur Heart J Suppl 17(Supplement D):D2–D8
Cox JL, Pieper K (2015) Harnessing the power of real-life data. Eur Heart J Supp. 17(Supplement D):D9–D14
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283:2008–2012
Valdemarsson S, Hedner P, Nilsson-Ehle P (1987) Increase in hepatic lipase activity after testosterone substitution in men with hypogonadism of pituitary origin. Acta Med Scand. 221:363–366
Rebuffé-Scrive M, Mårin P, Björntorp P (1991) Effect of testosterone on abdominal adipose tissue in men. Int J Obes 15:791–795
Forbes GB, Porta CR, Herr BE, Griggs RC (1992) Sequence of changes in body composition induced by testosterone and reversal of changes after drug is stopped. JAMA 267:397–399
Mårin P, Krotkiewski M, Björntorp P (1992) Androgen treatment of middle-aged, obese men: effects on metabolism, muscle and adipose tissues. Eur J Med 1:329–336
Brodsky IG, Balagopal P, Nair KS (1996) Effects of testosterone replacement on muscle mass and muscle protein synthesis in hypogonadal men—a clinical research center study. J Clin Endocrinol Metab 81:3469–3475
Katznelson L, Finkelstein JS, Schoenfeld DA, Rosenthal DI, Anderson EJ, Klibanski A (1996) Increase in bone density and lean body mass during testosterone administration in men with acquired hypogonadism. J Clin Endocrinol Metab 81:4358–4365
Wang C, Eyre DR, Clark R, Kleinberg D, Newman C, Iranmanesh A et al (1996) Sublingual testosterone replacement improves muscle mass and strength, decreases bone resorption, and increases bone formation markers in hypogonadal men—a clinical research center study. J Clin Endocrinol Metab 81:3654–3662
Zgliczynski S, Ossowski M, Slowinska-Srzednicka J, Brzezinska A, Zgliczynski W, Soszynski P et al (1996) Effect of testosterone replacement therapy on lipids and lipoproteins in hypogonadal and elderly men. Atherosclerosis 121:35–43
Bhasin S, Storer TW, Berman N, Yarasheski KE, Clevenger B, Phillips J et al (1997) Testosterone replacement increases fat-free mass and muscle size in hypogonadal men. J Clin Endocrinol Metab 82:407–413
Tan KC, Shiu SW, Pang RW, Kung AW (1998) Effects of testosterone replacement on HDL subfractions and apolipoprotein A-I containing lipoproteins. Clin Endocrinol (Oxf). 48:187–194
Brill KT, Weltman AL, Gentili A, Patrie JT, Fryburg DA, Hanks JB et al (2002) Single and combined effects of growth hormone and testosterone administration on measures of body composition, physical performance, mood, sexual function, bone turnover, and muscle gene expression in healthy older men. J Clin Endocrinol Metab 87:5649–5657
Minnemann T, Schubert M, Hübler D, Gouni-Berthold I, Freude S, Schumann C et al (2007) A four-year efficacy and safety study of the long-acting parenteral testosterone undecanoate. Aging Male 10:155–158
Naharci MI, Pinar M, Bolu E, Olgun A (2007) Effect of testosterone on insulin sensitivity in men with idiopathic hypogonadotropic hypogonadism. Endocr Pract 13:629–635
La Vignera S, Calogero AE, Condorelli R, Lanzafame F, Giammusso B, Vicari E (2009) Andrological characterization of the patient with diabetes mellitus. Minerva Endocrinol 34:1–9
Moon DG, Park MG, Lee SW, Park K, Park JK, Kim SW, Park NC et al (2010) The efficacy and safety of testosterone undecanoate (Nebido®) in testosterone deficiency syndrome in Korean: a multicenter prospective study. J Sex Med 7(6):2253–2260
Permpongkosol S, Tantirangsee N, Ratana-olarn K (2010) Treatment of 161 men with symptomatic late onset hypogonadism with long-acting parenteral testosterone undecanoate: effects on body composition, lipids, and psychosexual complaints. J Sex Med 7:3765–3774
Garcia JA, Sanchez PE, Fraile C, Escovar P (2011) Testosterone undecanoate improves erectile dysfunction in hypogonadal men with the metabolic syndrome refractory to treatment with phosphodiesterase type 5 inhibitors alone. Andrologia 43:293–296
Schwarz ER, Willix RD Jr (2011) Impact of a physician-supervised exercise-nutrition program with testosterone substitution in partial androgen-deficient middle-aged obese men. J Geriatr Cardiol 8:201–206
Arafa M, Zohdy W, Aboulsoud S, Shamloul R (2012) Prevalence of late-onset hypogonadism in men with type 2 diabetes mellitus. Andrologia. 44(Suppl 1):756–763
Schroeder ET, He J, Yarasheski KE, Binder EF, Castaneda-Sceppa C, Bhasin S et al (2012) Value of measuring muscle performance to assess changes in lean mass with testosterone and growth hormone supplementation. Eur J Appl Physiol 112:1123–1131
Jo DG, Lee HS, Joo YM, Seo JT (2013) Effect of testosterone replacement therapy on bone mineral density in patients with Klinefelter syndrome. Yonsei Med J 54:1331–1335
Ko YH, Moon DG, Moon KH (2013) Testosterone replacement alone for testosterone deficiency syndrome improves moderate lower urinary tract symptoms: one year follow-up. World J Mens Health 31:47–52
Rodriguez-Tolrà J, Torremadé Barreda J, del Rio L, di Gregorio S, Franco Miranda E (2013) Effects of testosterone treatment on body composition in males with testosterone deficiency syndrome. Aging Male. 16:184–190
Tirabassi G, Delli Muti N, Corona G, Maggi M, Balercia G (2013) Androgen receptor gene CAG repeat polymorphism regulates the metabolic effects of testosterone replacement therapy in male postsurgical hypogonadotropic hypogonadism. Int J Endocrinol. 2013:816740
Zitzmann M, Mattern A, Hanisch J, Gooren L, Jones H, Maggi M (2013) IPASS: a study on the tolerability and effectiveness of injectable testosterone undecanoate for the treatment of male hypogonadism in a worldwide sample of 1,438 men. J Sex Med 10:579–588
Pexman-Fieth C, Behre HM, Morales A, Kan-Dobrosky N, Miller MG (2014) A 6-month observational study of energy, sexual desire, and body proportions in hypogonadal men treated with a testosterone 1% gel. Aging Male 17:1–11
Conway AJ, Boylan LM, Howe C, Ross G, Handelsman DJ (1988) Randomized clinical trial of testosterone replacement therapy in hypogonadal men. Int J Androl 11:247–264
Sorva R, Kuusi T, Taskinen MR, Perheentupa J, Nikkilä EA (1988) Testosterone substitution increases the activity of lipoprotein lipase and hepatic lipase in hypogonadal males. Atherosclerosis 69:191–197
Ozata M, Yildirimkaya M, Bulur M, Yilmaz K, Bolu E, Corakci A et al (1996) Effects of gonadotropin and testosterone treatments on Lipoprotein(a), high density lipoprotein particles, and other lipoprotein levels in male hypogonadism. J Clin Endocrinol Metab 81:3372–3378
Tripathy D, Shah P, Lakshmy R, Reddy KS (1998) Effect of testosterone replacement on whole body glucose utilisation and other cardiovascular risk factors in males with idiopathic hypogonadotrophic hypogonadism. Horm Metab Res 30:642–645
Andrade ES Jr, Clapauch R, Buksman S (2009) Short term testosterone replacement therapy improves libido and body composition. Arq Bras Endocrinol Metabol 53:996–1004
Wu XY, Mao JF, Lu SY, Zhang Q, Shi YF (2009) Testosterone replacement therapy improves insulin sensitivity and decreases high sensitivity C-reactive protein levels in hypogonadotropic hypogonadal young male patients. Chin Med J (Engl) 122:2846–2850
Cochrane Handbook for Systematic Reviews of Interventions. Available at http://www.cochrane-handbook.org. Last accessed 26 Dec 2015
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Cohen J (1977) Statistical power analysis for the behavioral sciences. Academic Press, New York
Yassin A, Doros G (2013) Testosterone therapy in hypogonadal men results in sustained and clinically meaningful weight loss. Clin Obes 3:73–83
Crewther BT, Kilduff LP, Cook CJ (2014) Trained and untrained males show reliable salivary testosterone responses to a physical stimulus, but not a psychological stimulus. J Endocrinol Investig 37:1065–1072
Sgrò P, Romanelli F, Felici F, Sansone M, Bianchini S, Buzzachera CF, Baldari C, Guidetti L, Pigozzi F, Lenzi A, Di Luigi L (2014) Testosterone responses to standardized short-term sub-maximal and maximal endurance exercises: issues on the dynamic adaptive role of the hypothalamic-pituitary-testicular axis. J Endocrinol Investig 37:13–24
Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA et al (2016) Effects of testosterone treatment in older men. N Engl J Med 374:611–624
Corona G, Rastrelli G, Maggi M (2015) The pharmacotherapy of male hypogonadism besides androgens. Expert Opin Pharmacother 16:369–487. Erratum in: Expert Opin Pharmacother. 2015;16:941. Ratrelli, Giulia [corrected to Rastrelli, Giulia]
Corona G, Rastrelli G, Vignozzi L, Maggi M (2012) Emerging medication for the treatment of male hypogonadism. Expert Opin Emerg Drugs 17:239–259
Rastrelli G, Giovannini L, Calogero AE, Gianfrilli D, Serra E, Pizzocaro A, Giagulli VA, Motta G, Vancieri G, Sperandio A, Andò S, Selice R, Luca G, Cocchiara F, Canale D, Maggi M (2016) Predictors and clinical consequences of starting androgen therapy in men with low testosterone: results from the SIAMO-NOI registry. J Endocrinol Invest 39(6):695–708
Corona G, Maseroli E, Rastrelli G, Isidori AM, Sforza A, Mannucci E et al (2014) Cardiovascular risk associated with testosterone-boosting medications: a systematic review and meta-analysis. Expert Opin Drug Saf 13:1327–1351
Calof OM, Singh AB, Lee ML, Kenny AM, Urban RJ, Tenover JL et al (2005) Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci 60:1451–1457
Haddad RM, Kennedy CC, Caples SM, Tracz MJ, Boloña ER, Sideras K et al (2007) Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc 82:29–39
Fernández-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ et al (2010) Clinical review 1: adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab 95:2560–2575
Borst SE, Shuster JJ, Zou B, Ye F, Jia H, Wokhlu A, Yarrow JF (2014) Cardiovascular risks and elevation of serum DHT vary by route of testosterone administration: a systematic review and meta-analysis. BMC Med 12:211
Xu L, Freeman G, Cowling BJ, Schooling CM (2013) Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med 11:108
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the review.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Since this is a meta-analysis informed consent is not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Corona, G., Giagulli, V.A., Maseroli, E. et al. Testosterone supplementation and body composition: results from a meta-analysis of observational studies. J Endocrinol Invest 39, 967–981 (2016). https://doi.org/10.1007/s40618-016-0480-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-016-0480-2