Abstract
Purpose
There is much controversy regarding the use of oral contraceptive pills (OCPs) on cardiometabolic parameters, which is why this longitudinal population-based study was conducted to assess the impact of OCP use and its duration on cardiometabolic factors.
Methods
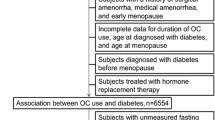
Of 5532 reproductive-aged participants of the Tehran lipid and glucose study, 3160 women who met our inclusion criteria were subdivided according to the duration of OCPs consumption into four sub-groups: (1) Non-users; (2) <11 month users; (3) 12–35 month users, and (4) ≥36 month users, and their cardiometabolic parameters were compared.
Results
No statistical significant differences were observed between the cardiometabolic parameters of these sub-groups, after further adjustment for confounding factors including age, parity, and education, except for mean low-density lipoprotein-cholesterol which was significantly higher in women who used OCPs for >36 months in comparison to non-OCP users. The odds ratio of hypercholesterolemia was significantly higher in women who used OCPs for >36 months in comparison to non-OCP users; being 1.5 times higher than non-users (95 % CI 1.01–2.2).
Conclusion
Results showed that if used for less than 3 years, OCPs have no cardiometabolic effects.

Similar content being viewed by others

References
ESHRE (2006) Hormones and cardiovascular health in women. Hum Reprod Update 12:483–497
Mendelsohn ME, Karas RH (2005) Molecular and cellular basis of cardiovascular gender differences. Science 308(5728):1583–1587
WHO (1998) Cardiovascular disease and steroid hormone contraception. Tech Rep Ser 877:89
Godsland IF, Crook D, Devenport M, Wynn V (1995) Relationships between blood pressure, oral contraceptive use and metabolic risk markers for cardiovascular disease. Contraception 52(3):143–149
Fisch IR, Frank J (1977) Oral contraceptives and blood pressure. JAMA 237(23):2499–2503
Cain MD, Walters WA, Catt KJ (1971) Effects of oral contraceptive therapy on the renin-angiotensin system. J Clin Endocrinol Metab 33(4):671–676
Blum M, Zacharovich D, Gelernter I, Blum I (1988) Influence of oral contraceptive treatment on blood pressure and 24-hour urinary catecholamine excretion in smoking as compared with non-smoking women. Adv Contracept 4(2):143–149
Spellacy WN, Birk SA (1972) The effect of intrauterine devices, oral contraceptives, estrogens, and progestogens on blood pressure. Am J Obstet Gynecol 112(7):912–919
Whitworth JA, Scoggins BA, Andrews J, Williamson PM, Brown MA (1992) Haemodynamic and metabolic effects of short term administration of synthetic sex steroids in humans. Clin Exp Hypertens A 14(5):905–922
Godsland IF, Crook D, Simpson R, Proudler T, Felton C, Lees B et al (1990) The effects of different formulations of oral contraceptive agents on lipid and carbohydrate metabolism. N Engl J Med 323(20):1375–1381
Klaus JR, Hurwitz BE, Llabre MM, Skyler JS, Goldberg RB, Marks JB et al (2009) Central obesity and insulin resistance in the cardiometabolic syndrome: pathways to preclinical cardiovascular structure and function. J Cardiometab Syndr 4(2):63–71
Regitz-Zagrosek V, Lehmkuhl E, Mahmoodzadeh S (2007) Gender aspects of the role of the metabolic syndrome as a risk factor for cardiovascular disease. Gend Med 4(Suppl B):S162–S177
Hurwitz BE, Henry N, Goldberg RB (2009) Long-term oral contraceptive treatment, metabolic syndrome and measures of cardiovascular risk in pre-menopausal women: National Health and Nutrition Examination Survey 1999–2004. Gynecol Endocrinol 25(7):441–449
Brinton EA (1996) Oral estrogen replacement therapy in postmenopausal women selectively raises levels and production rates of lipoprotein A-I and lowers hepatic lipase activity without lowering the fractional catabolic rate. Arterioscler Thromb Vasc Biol 16(3):431–440
Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M et al (2002) Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1). Soz Praventivmed 47(6):408–426
http://www.who.int/mediacentre/factsheets/fs355/en/. Accessed Jan 2015
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645
Ford ES, Giles WH, Dietz WH (2002) Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 287(3):356–359
Ford ES (2005) Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care 28(11):2745–2749
Merz CN, Johnson BD, Berga S, Braunstein G, Reis SE, Bittner V (2006) Past oral contraceptive use and angiographic coronary artery disease in postmenopausal women: data from the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation. Fertil Steril 85(5):1425–1431
Coney P, Washenik K, Langley RG, DiGiovanna JJ, Harrison DD (2001) Weight change and adverse event incidence with a low-dose oral contraceptive: two randomized, placebo-controlled trials. Contraception 63(6):297–302
Lello S, Vittori G, Paoletti AM, Sorge R, Guardianelli F, Melis GB (2007) Effects on body weight and body composition of a low-dose oral estroprogestin containing ethinyl estradiol 20 microg plus levonorgestrel 100 microg. Gynecol Endocrinol 23(11):632–637
Watanabe RM, Azen CG, Roy S, Perlman JA, Bergman RN (1994) Defects in carbohydrate metabolism in oral contraceptive users without apparent metabolic risk factors. J Clin Endocrinol Metab 79(5):1277–1283
Kjos SL, Peters RK, Xiang A, Thomas D, Schaefer U, Buchanan TA (1998) Contraception and the risk of type 2 diabetes mellitus in Latina women with prior gestational diabetes mellitus. JAMA 280(6):533–538
Guazzelli CA, Lindsey PC, de Araujo FF, Barbieri M, Petta CA, Aldrighi JM (2005) Evaluation of lipid profile in adolescents during long-term use of combined oral hormonal contraceptives. Contraception 71(2):118–121
Wiegratz I, Lee JH, Kutschera E, Bauer HH, von Hayn C, Moore C et al (2002) Effect of dienogest-containing oral contraceptives on lipid metabolism. Contraception 65(3):223–229
Cheung MC, Walden CE, Knopp RH (1999) Comparison of the effects of triphasic oral contraceptives with desogestrel or levonorgestrel on apolipoprotein A-I-containing high-density lipoprotein particles. Metabolism 48(5):658–664
Kemmeren JM, Algra A, Grobbee DE (2001) Effect of second and third generation oral contraceptives on lipid metabolism in the absence or presence of the factor V Leiden mutation. J Intern Med 250(5):441–448
Walsh BW, Schiff I, Rosner B, Greenberg L, Ravnikar V, Sacks FM (1991) Effects of postmenopausal estrogen replacement on the concentrations and metabolism of plasma lipoproteins. N Engl J Med 325(17):1196–1204
Campos H, Sacks FM, Walsh BW, Schiff I, O’Hanesian MA, Krauss RM (1993) Differential effects of estrogen on low-density lipoprotein subclasses in healthy postmenopausal women. Metabolism 42(9):1153–1158
Ritsch A, Kaser S, Volgger B, Abfalter E, Sturm W, Ganzer H et al (2002) Enhancement of cholesteryl ester transfer in plasma by hormone-replacement therapy. Metabolism 51(5):599–604
Godsland IF (2004) Biology: risk factor modification by OCs and HRT lipids and lipoproteins. Maturitas 47(4):299–303
Schaefer EJ, Foster DM, Zech LA, Lindgren FT, Brewer HB Jr, Levy RI (1983) The effects of estrogen administration on plasma lipoprotein metabolism in premenopausal females. J Clin Endocrinol Metab 57(2):262–267
Jones DR, Schmidt RJ, Pickard RT, Foxworthy PS, Eacho PI (2002) Estrogen receptor-mediated repression of human hepatic lipase gene transcription. J Lipid Res 43(3):383–391
Carr BR (1998) Uniqueness of oral contraceptive progestins. Contraception 58(3 Suppl):23S–27S quiz 67S
Gaspard U, Endrikat J, Desager JP, Buicu C, Gerlinger C, Heithecker R (2004) A randomized study on the influence of oral contraceptives containing ethinylestradiol combined with drospirenone or desogestrel on lipid and lipoprotein metabolism over a period of 13 cycles. Contraception 69(4):271–278
Tehrani FR (2006) Contraception use behavior of Iranian women (5 selected provinces of Iran), Iran. Report No.: final research project report
Acknowledgments
We are indebted to all the study participants for the substantial time and effort contributed to this study. Acknowledgments are also due to the research staff at the (TLGS) Unit and personnel of the Research Endocrine Laboratory. The authors wish to thank Ms. N. Shiva for critical editing of English grammar and syntax of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests and that the source of funding is independent of the objectives and results found in this study.
Ethical approval
Approval of the ethical committee of the research institute for endocrine sciences was obtained for the study, and written consents were obtained from all study participants.
Informed consent
The written inform consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Farahmand, M., Ramezani Tehrani, F., Rostami Dovom, M. et al. The impact of oral contraceptives on cardiometabolic parameters. J Endocrinol Invest 39, 277–283 (2016). https://doi.org/10.1007/s40618-015-0346-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-015-0346-z