Abstract
Background
COVID-19 vaccination is vital for ending the pandemic, yet safety concerns persist among pregnant and postpartum women, especially those who are Black and Hispanic. This study aims to explore factors that influence postpartum women’s vaccination decision-making during pregnancy and postpartum through women’s lived experiences and maternal care providers’ (MCPs) observations.
Methods
From January to August 2022, we conducted semi-structured interviews with postpartum women who are Black and Hispanic and with MCPs. Participants were recruited from obstetric and pediatric clinics in South Carolina and had given birth in 2021. Thematic analysis was employed for data analysis.
Results
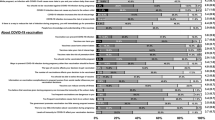
The study involved 19 Black and 20 Hispanic women, along with 9 MCPs, and revealed both barriers and facilitators to COVID-19 vaccination. The factors that influence pregnant and postpartum women’s decision about COVID-19 vaccine uptake included: 1) awareness of health threats associated with COVID-19 vaccines, 2) vaccine availability and accessibility, 3) vaccine-related knowledge and exposure to misinformation, 4) concerns regarding pre-existing health conditions and potential side effects of COVID-19 vaccines, 5) emotional factors associated with vaccination decision-making processes, 6) concerns about the well-being of infants, 7) cultural perspectives, and 8) encouragement by trusted supporters.
Conclusion
The findings suggest that reliable information, social support, and trusted MCPs’ advice can motivate COVID-19 vaccination among pregnant and postpartum women who are Black and Hispanic. However, barriers such as misinformation, mistrust in the health care system, and fears of potential side effects impede vaccination uptake. Future interventions should address these barriers, consider health disparities, involve trusted MCPs, and initiate conversations about vaccines to promote vaccination among these populations.
Similar content being viewed by others
Data Availability
The data presented in this study are available on request from the corresponding author (RZ). The data are not publicly available due to privacy concerns.
Code Availability
Not applicable.
Change history
29 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40615-024-01964-8
References
Razzaghi H, et al. COVID-19 Vaccination Coverage Among Pregnant Women During Pregnancy - Eight Integrated Health Care Organizations, United States, December 14, 2020-May 8, 2021. Mmwr-Morb Mortal Wkly Rep. 2021;70(24):895–9. https://doi.org/10.1101/2021.03.26.21254402v1.
GoncuAyhan S, et al. COVID-19 vaccine acceptance in pregnant women. Int J Gynecol Obstet. 2021;154(2):291–6.
Regan AK, Kaur R, Nosek M, Swathi PA, Gu NY. COVID-19 vaccine acceptance and coverage among pregnant persons in the United States. Prev Med Rep. 2022;29:101977. https://doi.org/10.1016/j.pmedr.2022.101977.
Morgan JA, et al. Research letter maternal outcomes after severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection in vaccinated compared with unvaccinated pregnant patients. Obstet Gynecol. 2022;139(1):107–9. https://doi.org/10.1097/Aog.0000000000004621.
Chervenak FA, et al. Professionally responsible coronavirus disease 2019 vaccination counseling of obstetrical and gynecologic patients. Am J Obstet Gynecol. 2021;224(5):470–8. https://doi.org/10.1016/j.ajog.2021.01.027.
Grunebaum A, McCullough LB, Litvak A, Chervenak FA. Inclusion of pregnant individuals among priority populations for coronavirus disease 2019 vaccination for all 50 states in the United States. Am J Obstet Gynecol. 2021;224(5):536–9. https://doi.org/10.1016/j.ajog.2021.01.026.
Januszek SM, et al. The approach of pregnant women to vaccination based on a COVID-19 systematic review. Medicina (Kaunas). 2021;57(9):977. https://doi.org/10.3390/medicina57090977.
Badell ML, Dude CM, Rasmussen SA, Jamieson DJ. Covid-19 vaccination in pregnancy. BMJ. 2022;378:e069741. https://doi.org/10.1136/bmj-2021-069741.
Male V. Are COVID-19 vaccines safe in pregnancy? Nat Rev Immunol. 2021;21(4):200–1. https://doi.org/10.1038/s41577-021-00525-y.
Blakeway H, et al. COVID-19 vaccination during pregnancy: coverage and safety. Am J Obstet Gynecol. 2022;226(2):236 e1-236 e14. https://doi.org/10.1016/j.ajog.2021.08.007.
Zhang R, Qiao S, McKeever BW, Olatosi B, Li XM. Listening to voices from African American communities in the Southern States about COVID-19 vaccine information and communication: a qualitative study. Vaccines-Basel. 2022;10(7):1046. https://doi.org/10.3390/vaccines10071046.
Mheidly N, Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020;41(4):410–20. https://doi.org/10.1057/s41271-020-00247-w.
Huang L, Riggan KA, Ashby GB, Rivera-Chiauzzi EY, Allyse MA. Pregnant and postpartum patients’ views of COVID-19 vaccination. J Community Health. 2022;47(5):871–8. https://doi.org/10.1007/s10900-022-01118-z.
Rasmussen SA, Jamieson DJ. Pregnancy, postpartum care, and COVID-19 vaccination in 2021. JAMA. 2021;325(11):1099–100. https://doi.org/10.1001/jama.2021.1683.
Siegel MR, James KE, Jaffe E, L’Heureux MM, Kaimal AJ, Goldfarb IT. Provider confidence in counseling preconception, pregnant, and postpartum patients regarding COVID-19 vaccination: a cross-sectional survey study. Health Sci Rep. 2023;6(5):e1163. https://doi.org/10.1002/hsr2.1163.
Konje JC, Al Beloushi M, Ahmed B. Immunisation against COVID-19 in pregnancy and of women planning pregnancy. Viruses. 2023;15(3):621. https://doi.org/10.3390/v15030621.
Cox E, et al. A mother’s dilemma: the 5-P model for vaccine decision-making in pregnancy. Vaccines-Basel. 2023;11(7):1248.
Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med. 2011;72(6):977–83. https://doi.org/10.1016/j.socscimed.2011.01.013.
Ogunwole SM, Oguntade HA, Bower KM, Cooper LA, Bennett WL. Health experiences of African American mothers, wellness in the postpartum period and beyond (HEAL): a qualitative study applying a critical race feminist theoretical framework. Int J Environ Res Public Health. 2023;20(13):6283. https://doi.org/10.3390/ijerph20136283.
Conteh N, Gagliardi J, McGahee S, Molina R, Clark CT, Clare CA. Medical mistrust in perinatal mental health. Harv Rev Psychiatry. 2022;30(4):238–47. https://doi.org/10.1097/HRP.0000000000000345.
Shavers VL, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66. https://doi.org/10.2105/AJPH.2012.300773.
Liu J, et al. Multilevel determinants of racial/ethnic disparities in severe maternal morbidity and mortality in the context of the COVID-19 pandemic in the USA: protocol for a concurrent triangulation, mixed-methods study. BMJ Open. 2022;12(6):e062294. https://doi.org/10.1136/bmjopen-2022-062294.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Clarke V, Braun V. Thematic analysis. J Posit Psychol. 2017;12(3):297–8.
Collins J, Alona I, Tooher R, Marshall H. Increased awareness and health care provider endorsement is required to encourage pregnant women to be vaccinated. Hum Vaccin Immunother. 2014;10(10):2922–9. https://doi.org/10.4161/21645515.2014.971606.
Sharma O, Sultan AA, Ding H, Triggle CR. A review of the progress and challenges of developing a vaccine for COVID-19. Front Immunol. 2020;11:585354. https://doi.org/10.3389/fimmu.2020.585354.
Rambhia KJ, Watson M, Sell TK, Waldhorn R, Toner E. Mass vaccination for the 2009 H1N1 pandemic: approaches, challenges, and recommendations. Biosecur Bioterror. 2010;8(4):321–30. https://doi.org/10.1089/bsp.2010.0043.
Njoku A, Joseph M, Felix R. Changing the narrative: structural barriers and racial and ethnic inequities in COVID-19 vaccination. Int J Environ Res Public Health. 2021;18(18):9904. https://doi.org/10.3390/ijerph18189904.
Colon-Lopez V, et al. Understanding parents’ views toward the newly enacted HPV vaccine school entry policy in Puerto Rico: a qualitative study. BMC Public Health. 2021;21(1):1938. https://doi.org/10.1186/s12889-021-11952-w.
Hodgkinson EL, Smith DM, Wittkowski A. Women’s experiences of their pregnancy and postpartum body image: a systematic review and meta-synthesis. BMC Pregnancy Childbirth. 2014;14(1):1–11.
Cai C, Busch S, Wang R, Sivak A, Davenport MH. Physical activity before and during pregnancy and maternal mental health: a systematic review and meta-analysis of observational studies. J Affect Disord. 2022;309:393–403.
Meaney S, Leitao S, Olander EK, Pope J, Matvienko-Sikar K. The impact of COVID-19 on pregnant womens’ experiences and perceptions of antenatal maternity care, social support, and stress-reduction strategies. Women Birth. 2022;35(3):307–16.
Wastnedge EA, et al. Pregnancy and COVID-19. Physiol Rev. 2021;101(1):303–18.
AuYoung M, et al. Addressing racial/ethnic inequities in vaccine hesitancy and uptake: lessons learned from the California alliance against COVID-19. J Behav Med. 2023;46(1–2):153–66. https://doi.org/10.1007/s10865-022-00284-8.
ACOG. Committee Opinion: No. 563: Ethical Issues in Pandemic Influenza Planning Concerning Pregnant Women. Obstet Gynecol. 2013;121(5):1138–43. https://doi.org/10.1097/01.AOG.0000429660.31589.6a.
Funding
This research was supported by the National Institute of Allergy and Infectious Diseases and Office of the Director of the National Institutes of Health under Award Number R01AI127203-5S2 for Implementing a Maternal health and PRegnancy Outcomes Vision for Everyone (IMPROVE). XL and JL are the MPIs for this study.
Author information
Authors and Affiliations
Contributions
JL and SQ conceptualized and designed the study. RZ and TB wrote the first draft and SQ, JL, MET, and XL participated in writing sections of the original proposal. All authors critically reviewed and edited the manuscript. JL, MET, TB, and RZ participated in data collection, data analysis, and data interpretation. JL and XL secured the funding.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Institutional Review Board of the University of South Carolina (Pro00115169).
Consent to Participate
Informed consent was obtained from all individual participants prior to participating in the study.
Consent for Publication
All participants gave consent for the research team to publish the findings of the study.
Conflicts of Interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised due to a retrospective Open Access cancellation.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, R., Byrd, T., Qiao, S. et al. Is It Safe for Me to Get It? Factors Influencing COVID-19 Vaccination Decision-Making among Postpartum Women Who Are Black and Hispanic in Deep South. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-01931-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-01931-3