Abstract
Objective
To report the domains of Black mothers’ experiences with preterm infants in the neonatal intensive care unit (NICU) and to determine the frameworks used.
Methods
A systematic review of the literature using the PRISMA guideline was performed. An electronic database search of published literature between 2000 and 2022 was conducted based on predetermined search terms and parameters.
Results
Twenty-seven articles met the inclusion and exclusion criteria. Eleven articles focused on feeding practices, ten reported on nursing/maternal care experiences, five reported mental health/social support, and only one focused on mother-infant relationships. Only five papers reported using any frameworks, comprising grounded theory framework (n = 2), theory of planned behavior (n = 1), research justice framework (n = 1), and the patient and public engagement protocol (n = 1).
Discussion
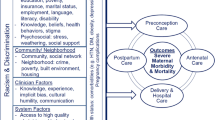
A holistic approach to understanding the multifactorial experiences of Black mothers with preterm infants needs to be socio-culturally competent to ensure their diverse intersections and identities are accurately represented and understood. Rigorous research at the intersection of Black maternal health and the NICU hold promises for advancing maternal health equity in the United States.

Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Centers for Disease Control and Prevention. preterm birth | maternal and infant health | Reproductive Health | CDC. Published 2021. Accessed 18 Jun 2022. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm.
Vogel JP, Chawanpaiboon S, Moller AB, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3–12. https://doi.org/10.1016/J.BPOBGYN.2018.04.003.
Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511. https://doi.org/10.1371/JOURNAL.PONE.0138511.
U.S. Department of Health and Human Services. Infant Mortality and African Americans - The Office of Minority Health. Published 2021. Accessed 18 Jun 2022. https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23.
Riddell CA, Harper S, Kaufman JS. Trends in differences in US Mortality rates between black and white infants. JAMA Pediatr. 2017;171(9):911–3. https://doi.org/10.1001/JAMAPEDIATRICS.2017.1365.
Hoyert LD. Maternal mortality rates in the United States, 2019. Published online April 1, 2020. https://stacks.cdc.gov/view/cdc/103855. Accessed 18 Jun 2022.
Liu J, Sakarovitch C, Sigurdson K, Lee HC, Profit J. Disparities in health care-associated infections in the NICU. Am J Perinatol. 2020;37(2):166–73. https://doi.org/10.1055/S-0039-1688481.
Sigurdson K, Morton C, Mitchell B, Profit J. Disparities in NICU quality of care: a qualitative study of family and clinician accounts. J Perinatol. 2018;38(5):600–7. https://doi.org/10.1038/s41372-018-0057-3.
Janevic T, Zeitlin J, Auger N, et al. Association of race/ethnicity with very preterm neonatal morbidities. JAMA Pediatr. 2018;172(11):1061–9. https://doi.org/10.1001/JAMAPEDIATRICS.2018.2029.
Profit J, Zupancic JAF, Gould JB, et al. Correlation of neonatal intensive care unit performance across multiple measures of quality of care. JAMA Pediatr. 2013;167(1):47–54. https://doi.org/10.1001/jamapediatrics.2013.418.
Horbar JD, Edwards EM, Greenberg LT, et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 2019;173(5):455–61. https://doi.org/10.1001/JAMAPEDIATRICS.2019.0241.
Sigurdson K, Mitchell B, Liu J, et al. Racial/ethnic disparities in neonatal intensive care: A systematic review. Pediatrics. 2019;144(2):e20183114. https://doi.org/10.1542/PEDS.2018-3114/76884.
Bower KM, Geller RJ, Perrin NA, Alhusen J. Experiences of racism and preterm birth: findings from a pregnancy risk assessment monitoring System, 2004 through 2012. Women’s Heal Issues. 2018;28(6):495–501. https://doi.org/10.1016/J.WHI.2018.06.002.
Ruiz RL, Shah MK, Lewis ML, Theall KP. Perceived access to health services and provider information and adverse birth outcomes: findings from LaPRAMS, 2007–2008. South Med J. 2014;107(3):137–43. https://doi.org/10.1097/SMJ.0000000000000065.
Padula AM, Shariff-Marco S, Yang J, et al. Multilevel social factors and NICU quality of care in California. J Perinatol. 2020;41(3):404–12. https://doi.org/10.1038/s41372-020-0647-8.
Giurgescu C, Banks A, Dancy BL, Norr K. African American women’s views of factors impacting preterm birth. MCN Am J Matern Child Nurs. 2013;38(4):229. https://doi.org/10.1097/NMC.0B013E318293BBBB.
Winter L, Colditz PB, Sanders MR, Boyd RN, et al. Depression, posttraumatic stress and relationship distress in parents of very preterm infants. Arch Women’s Mental Health. 2018;21(4):445–51.
Trumello C, Candelori C, Cofini M, Cimino S, et al. Mothers’ depression, anxiety, and mental representations after preterm birth: a study during the infant’s hospitalization in a neonatal intensive care unit. Front Public Health. 2018;7(6):359.
Collins PH. Black feminist thought: knowledge, consciousness, and the politics of empowerment. 2nd ed. New York: Routledge; 2000.
Witt RE, Colvin BN, Lenze SN, Forbes ES, et al. Lived experiences of stress of Black and Hispanic mothers during hospitalization of preterm infants in neonatal intensive care units. J Perinatol. 2022;42(2):195–201.
Calthorpe LM, Baer RJ, Chambers BD, Steurer MA, et al. The association between preterm birth and postpartum mental healthcare utilization among California birthing people. Am J Obstet Gynecol MFM. 2021;3(4):100380.
Salihu HM, Dongarwar D, Oduguwa E, Atkinson JO, Harris TB. Racial/ethnic disparity in suicidal ideation, suicide attempt and non-suicidal intentional self-harm among pregnant women in the United States. J Immigr Minor Health. 2022;24(3):588–96.
Conteh N, Gagliardi J, McGahee S, Molina R, et al. Medical mistrust in perinatal mental health. Harv Rev Psychiatry. 2022;30(4):238–47.
Betancourt JR, Green AR, Carrillo JE. Ananeh-Firempong O (2016) Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2016;118(4):293–302. https://doi.org/10.1016/S0033-3549(04)50253-4.
Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–8. https://doi.org/10.1016/J.SOCSCIMED.2010.07.030.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/S13643-021-01626-4
Huey SJ, Polo AJ. Evidence-based psychosocial treatments for ethnic minority youth. J Clin Child Adolesc Psychol. 2008;37(1):262–301. https://doi.org/10.1080/15374410701820174.
Pina AA, Polo AJ, Huey SJ. Evidence-based psychosocial interventions for ethnic minority youth: the 10-year update. J Clin Child Adolesc Psychol. 2019;48(2):179–202. https://doi.org/10.1080/15374416.2019.1567350.
Ponting C, Mahrer NE, Zelcer H, Dunkel Schetter C, Chavira DA. Psychological interventions for depression and anxiety in pregnant Latina and Black women in the United States: a systematic review. Clin Psychol Psychother. 2020;27(2):249–65. https://doi.org/10.1002/CPP.2424.
Garrard J. Health sciences literature review made easy. 6th edition. MA: Jones & Bartlett Learning. 2020.
Creswell J, Poth NC. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. 4th ed. California: Sage Publications, Inc; 2018.
McLemore MR, Altman MR, Cooper N, Williams S, Rand L, Franck L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc Sci Med. 2018;201:127–35. https://doi.org/10.1016/J.SOCSCIMED.2018.02.013.
Glazer KB, Sofaer S, Balbierz A, Wang E, Howell EA. Perinatal care experiences among racially and ethnically diverse mothers whose infants required a NICU stay. J Perinatol. 2020;41(3):413–21. https://doi.org/10.1038/s41372-020-0721-2.
Martin AE, D’Agostino JA, Passarella M, Lorch SA. Racial differences in parental satisfaction with neonatal intensive care unit nursing care. J Perinatol. 2016;36(11):1001–7. https://doi.org/10.1038/jp.2016.142.
Enlow E, Faherty LJ, Wallace-Keeshen S, Martin AE, Shea JA, Lorch SA. Perspectives of low socioeconomic status mothers of premature infants. Pediatrics. 2017;139(3). https://doi.org/10.1542/PEDS.2016-2310/53638
Rossman B, Greene MM, Meier PP. The role of peer support in the development of maternal identity for “NICU Moms.” J Obstet Gynecol Neonatal Nurs. 2015;44(1):3–16. https://doi.org/10.1111/1552-6909.12527.
Yee LM, Leziak K, Jackson J, Miller ES. Barriers and facilitators to recurrent preterm birth prevention among low-income women: a qualitative study. Am J Perinatol. 2019;36(9):955–63. https://doi.org/10.1055/S-0038-1675790/ID/JR180520-29.
Griffin JB, Pickler RH. Hospital-to-home transition of mothers of preterm infants. MCN Am J Matern Nurs. 2011;36(4):252–7. https://doi.org/10.1097/NMC.0B013E31821770B8.
Franck LS, McLemore MR, Williams S, et al. Research priorities of women at risk for preterm birth: findings and a call to action. BMC Pregnancy Childbirth. 2020;20(1):1–17. https://doi.org/10.1186/S12884-019-2664-1/TABLES/4.
Reyna BA, Pickler RH, Thompson A. A descriptive study of mothers’ experiences feeding their preterm infants after discharge. Adv Neonatal Care. 2006;6(6):333. https://doi.org/10.1016/J.ADNC.2006.08.007.
LoVerde B, Falck A, Donohue P, Hussey-Gardener B. supports and barriers to the provision of human milk by mothers of african american preterm infants. Adv Neonatal Care. 2018;18(3):179–88. https://doi.org/10.1097/ANC.0000000000000477.
Riley B, Schoeny M, Rogers L, et al. Barriers to human milk feeding at discharge of very low-birthweight infants: Evaluation of neighborhood structural factors. Breastfeed Med. 2016;11(7):335–42. https://doi.org/10.1089/BFM.2015.0185/ASSET/IMAGES/LARGE/FIGURE2.JPEG.
Fleurant E, Schoeny M, Hoban R, et al. Barriers to human milk feeding at discharge of very-low-birth-weight infants: maternal goal setting as a key social factor. Breastfeed Med. 2017;12(1):20–7. https://doi.org/10.1089/BFM.2016.0105/ASSET/IMAGES/LARGE/FIGURE1.JPEG.
Rossman B, Meier PP, Janes JE, Lawrence C, Patel AL. Human milk provision experiences, goals, and outcomes for teen mothers with low-birth-weight infants in the neonatal intensive care unit. https://home.liebertpub.com/bfm. 2017;12(6):351–358. https://doi.org/10.1089/BFM.2017.0035.
Fabiyi C, Rankin K, Norr K, Yoder JC, Vasa R, White-Traut R. The association of low social support with breast milk expression in low-income mother-preterm infant dyads. J Hum Lact. 2015;31(3):490–7. https://doi.org/10.1177/0890334415586199.
Miracle DJ, Meier PP, Bennett PA. Mothers’ decisions to change from formula to mothers’ milk for very-low-birth-weight infants. J Obstet Gynecol Neonatal Nurs. 2004;33(6):692–703. https://doi.org/10.1177/0884217504270665.
Hoban R, Bigger H, Patel AL, Rossman B, Fogg LF, Meier P. Goals for human milk feeding in mothers of very low birth weight infants: how do goals change and are they achieved during the NICU hospitalization? Breastfeed Med. 2015;10(6):305–11. https://doi.org/10.1089/BFM.2015.0047/ASSET/IMAGES/LARGE/FIGURE1.JPEG.
Dowling DA, Shapiro J, Burant CJ, Elfettoh AA. Factors influencing feeding decisions of black and white mothers of preterm infants. J Obstet Gynecol Neonatal Nurs. 2009;38(3):300–9. https://doi.org/10.1111/J.1552-6909.2009.01018.X.
Patel AL, Johnson TJ, Engstrom JL, et al. Impact of early human milk on sepsis and healthcare costs in very low birth weight infants. J Perinatol. 2013;33(7):514–9. https://doi.org/10.1038/jp.2013.2.
Johnson TJ, Patel AL, Bigger HR, et al. E-mail cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology. 2015;107:271–6. https://doi.org/10.1159/000370058.
White-Traut R, Rankin K, Fabiyi C, Liu L, Cheung I, Norr K. Maternal characteristics associated with social support in at-risk mothers of premature infants. J Obstet Gynecol Neonatal Nurs. 2017;46(6):824–33. https://doi.org/10.1016/J.JOGN.2017.07.008.
Holditch-Davis D, Santos H, Levy J, et al. Patterns of psychological distress in mothers of preterm infants. Infant Behav Dev. 2015;41:154–63. https://doi.org/10.1016/J.INFBEH.2015.10.004.
Holditch-Davis D, Miles MS, Weaver MA, et al. Patterns of distress in African American mothers of preterm infants. J Dev Behav Pediatr. 2009;30(3):193. https://doi.org/10.1097/DBP.0B013E3181A7EE53.
Greene MM, Rossman B, Patra K, Kratovil AL, Janes JE, Meier PP. Depressive, anxious and perinatal post-traumatic distress in mothers of very low birth weight infants in the NICU. J Dev Behav Pediatr. 2015;36(5):362. https://doi.org/10.1097/DBP.0000000000000174.
Witt RE, Colvin BN, Lenze SN, et al. Lived experiences of stress of Black and Hispanic mothers during hospitalization of preterm infants in neonatal intensive care units. J Perinatol. 2021;42(2):195–201. https://doi.org/10.1038/s41372-021-01241-0.
Teti DM, Black MM, Viscardi R, et al. Intervention With African American premature infants: four-month results of an early intervention program. 101177/1053815109331864. 2009;31(2):146–166. https://doi.org/10.1177/1053815109331864
Bryant AS, Riley LE, Neale D, et al. Communicating with African-American women who have had a preterm birth about risks for future preterm births. J Racial Ethn Heal Disparities. 2020;7(4):671–7. https://doi.org/10.1007/S40615-020-00697-8/TABLES/1.
Mendez-Escobar E, Adegoke TM, Lee-Parritz A, et al. Health equity accelerator: a health system’s approach. NEJM Catalyst Innov Care Deliv. 2022. https://doi.org/10.1056/CAT.22.0115.
White VanGompel E, Lai JS, Davis DA, et al. Psychometric validation of a patient-reported experience measure of obstetric racism© (The PREM-OB Scale™ suite). Birth. 2022;00:1–12. https://doi.org/10.1111/BIRT.12622.
Chiang KV, Li R, Anstey EH, Perrine CG. Racial and ethnic disparities in breastfeeding initiation─ United States, 2019. Morb Mortal Wkly Rep. 2021;70(21):769.
Putnick D, Sundaram R, Bell E, et al. Trajectories of maternal postpartum depressive symptoms. Pediatrics. 2020;146(5):e20200857. https://doi.org/10.1542/peds.2020-0857.
Gerstein E, Njoroge WFM, Paul RA, et al. Maternal depression and stress in the neonatal intensive care unit: associations with mother− child interactions at age 5 years. J Am Acad Child Adolesc Psychiatry. 2019;58(3):350-358.e2. https://doi.org/10.1016/j.jaac.2018.08.016.
Badr LK. Is the Effect of postpartum depression on mother-infant bonding universal? Infant Behav Dev. 2018;51:15–23. https://doi.org/10.1016/J.INFBEH.2018.02.003.
Gooding J, Cooper L, Blaine A, et al. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35(1):20–8. https://doi.org/10.1053/j.semperi.2010.10.004.
Curry SJ, Krist AH, Owens DK, et al. Interventions to prevent perinatal depression: US preventive services task force recommendation statement. JAMA - J Am Med Assoc. 2019;321(6):580–7. https://doi.org/10.1001/JAMA.2019.0007.
Hans SL, Edwards RC, Zhang Y. Randomized controlled trial of doula-home-visiting services: impact on maternal and infant health. Matern Child Health J. 2018;22(1):105–13. https://doi.org/10.1007/S10995-018-2537-7/TABLES/2.
Gjerdingen D, McGovern P, Pratt R, et al. Postpartum doula and peer telephone support for postpartum depression: a pilot randomized controlled trial. J Prim Care Community Health. 2013;4(1):36–43. https://doi.org/10.1177/2150131912451598.
Mottl-Santiago J, Herr K, Rodrigues D, et al. The birth sisters program: a model of hospital-based doula support to promote health equity. J Health Care Poor Underserved. 2020;31(1):43–55. https://doi.org/10.1353/hpu.2020.0007.
Scott KA. The rise of black feminist intellectual thought and political activism in perinatal quality improvement: a righteous rage about racism, resistance, resilience, and rigor. Wiley Online Libr. 2021;2(1):155–60. https://doi.org/10.1002/fea2.12045.
Sacks V, Murphey D. The prevalence of adverse childhood experiences, nationally, by state, and by race or ethnicity. 2018. http://hdl.handle.net/20.500.11990/1142.
Cavanaugh C, Nelson T. A national study of the influence of adverse childhood experiences on depression among Black adults in the United States. J Affect Disord. 2022;15(311):523–9. https://doi.org/10.1016/j.jad.2022.05.112.
Acknowledgements
We would like to thank Ms. Faith Elenwa, MPH, and Dr. Robin Page for their help screening the articles and reviewing the codebook. We also thank Drs. Carly McCord and Kelly Wilson for their overall guidance during this project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by [Kobi V. Ajayi]. The first draft of the manuscript was written by [Kobi V. Ajayi]. Supervision and revision [Whitney Garney]. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ajayi, K.V., Garney, W.R. Understanding the Domains of Experiences of Black Mothers with Preterm Infants in the United States: A Systematic Literature Review. J. Racial and Ethnic Health Disparities 10, 2453–2469 (2023). https://doi.org/10.1007/s40615-022-01425-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01425-0