Abstract
Background
Understanding the factors driving recruitment and enrollment of African Americans (AA)s in clinical translational research will assure that underrepresented populations benefit from scientific progress and new developments in the diagnosis and treatment of Alzheimer’s disease and related disorders. While transportation is pivotal to volunteers’ ability to participate in research, its contribution to enrollment in exercise studies on AD is yet to be elucidated. Thus, this research focuses on identifying factors that influence the recruitment and enrollment of African Americans in biomedical studies and determining whether the availability of transportation motivates participation in time-demanding exercise studies on AD.
Methods
We analyzed recruitment data collected from 567 volunteers ages 55 and older screened through various recruitment sources and considered for enrollment in our exercise and memory study. To determine whether transportation influenced the enrollment of African Americans (AA)s in biomedical studies, multiple logistic regression analysis was performed to identify significant factors that drive enrollment. Furthermore, the association of race and demographic factors on the availability of transportation was assessed.
Results
Demographic factors, age at screening, education, gender, and cognitive scores were not significantly different among those enrolled compared to control (not-enrolled). In the relationship of enrollment to transportation, enrolled participants were more likely to have access to transportation (79.12%) than not-enrolled participants who had less access to transportation (71.6%); however, the association was not statistically significant. However, race differentially influenced the likelihood of enrollment, with elderly AAs being significantly less likely to have transportation (p = 0.020) than the Whites but more likely than “others” to have transportation.
Conclusion
Our findings suggest that access to transportation may be a key factor motivating enrollment in an exercise and memory study in a predominantly AA sample. Notably, AAs in our sample were less likely to have transportation than Whites. Other demographic factors and cognitive scores did not significantly influence enrollment in our sample. A larger sample and more detailed assessment of transportation are needed to further discern the role of transportation in clinical trials.
Similar content being viewed by others
Background
Clinical research is necessary to generate evidence for the efficacy and safety of new therapies. Some subgroups of patients may respond differently to medical therapies; for example, women may respond differently than men, and members from one racial or ethnic group may respond differently than those from another [13]. Therefore, a diversity of clinical trial participants is needed to help ensure that the trial population is representative of the patients who will use the medicine or medicinal product and ensure that the results are generalizable [8]. For many decades, ethnic minority groups have historically been underrepresented in clinical trials, a shortcoming that persists in modern trials [27]. Furthermore, because of changing demographics, more than 50% of the US population is projected to be other than non-Hispanic white by 2045 [17]. Congruently, the under-representation of underrepresented ethnic groups in clinical research is a continuing promoter of healthcare disparities in the USA [30]. This under-representation occurs in all types of clinical research and or therapeutic areas, including those diseases that predominantly affect underrepresented groups [7]. Regrettably, the lack of substantive progress affirms that the key parties involved in planning and conducting clinical trials (investigators, sponsors, and regulators) have not fully prioritized inclusion [35]. Upon directives in legislation passed by Congress in the early 1990s, the National Institutes of Health (NIH) instituted policies aimed at increasing the representation of underrepresented populations in clinical trials funded by the agency [5].
The inclusion of diverse participants in clinical research may lead to more robust and complete data that broadens the understanding of racial and ethnic differences in treatment responses, which may contribute to reduced disparities in outcomes [32]. Indorewalla et al. [21] outlined the barriers to recruitment for older adult participants from underrepresented minorities, noting that the need to undergo repeated diagnostic and neurocognitive evaluations, health insurance issues, lack of adequate transportation to and from the medical facility, and high costs of transportation burden participants and deter them from enrolling in ongoing clinical trials [21].
Transportation has been shown to play a significant role in the recruitment and enrollment of AA in biomedical studies. Rivers et al. [31] reported that important impediments to successful recruitment of AA to clinical trials included negative attitudes towards clinical trials, low levels of knowledge and awareness regarding clinical trials, and religious beliefs. Importantly structural barriers such as transportation, childcare, and access to healthcare [31] were also noted. The authors acknowledged that AA patients are more likely to have transportation problems getting to their medical appointments than non-Hispanic White patients. Furthermore, the authors added that key strategies that may improve the recruitment and enrollment of AA in clinical trials include resources for transportation to screening appointments, parking, and media advertising [6, 31]. According to Baquet et al. [4], important determinants for participation in clinical trials include lack of transportation, especially for AA females [4]. It is important to note that an exercise study requires multiple visits/weeks over several months. Transportation, therefore, would be critical to volunteers’ ability to participate in clinical trials. Underrepresented minorities may have less transportation due to social-economic means, education, and income [21]. Therefore, we examined factors that influence enrollment of AAs in biomedical studies and determined whether the availability of transportation motivates increased participation. In addition, we examined the association of race and demographic factors on the availability of transportation in motiving participation in these time-demanding exercise studies on memory.
Methods
The Institutional Review Board (IRB) of Howard University approved the protocols used for this study. As part of the requirement for human subject studies, participants completed a signed consent form before enrolling in the study. In addition, a detailed description of the gene, exercise, and memory study (GEMS) has been published.
Screening Study Population
We analyzed recruitment data consisting of potential volunteers ages 55 or older engaged at various recruitment sources. Engaged participants included those contacted or prescreened (no signed consent form); enrolled participants included those that were consented and screened; not-enrolled included those that consented but screen-failed. Volunteers completed a Mini–Mental State Exam (MMSE) as part of screening and recruitment for this study. The screening eligibility of the participants consisted of the ability to exercise vigorously without causing harm to self, no chronic medical condition, and met the Petersen MCI criteria [29], which include the following: age and education adjusted score 24–30 inclusive, have objective memory loss, and memory complaints. After completing the informed consent, demographic and general medical history were obtained from the volunteers. Participants who completed the intervention and confirmed to be MCI were randomly assigned to a 6-month program of either aerobic or stretch exercise. These participants underwent 40 min of supervised training three times/week. VO2Max was determined at baseline and repeated after volunteers completed the 6-month exercise program. Most participants used public transportation for the visits, and only a few owned means of transportation.
During the recruitment period, the Division of Geriatrics organized, sponsored, and participated in many health promotion events to educate a predominantly AA community on the warning signs, identification, treatment, and lifestyle changes to reduce the risk of developing AD. These efforts occurred at geriatric and other medical clinics, church events, health fairs, senior housing and assisted living facilities, and senior wellness centers. Additional community engagement activities occurred during Annual NBC News Expo and Annual Congressional Black Caucus Health Event and Christmas gatherings; engagement of Pastoral Leadership Group; through Direct mailing, Newspaper Advertisements; Hospital and Community-Based Flyers; and Hospital Billboard. Study volunteers were not compensated for initial engagements and screenings but received stipends based on completed study visits. The community and leadership groups were first contacted through third parties or an introductory letter, followed by telephone calls.
Recruitment Strategies
The community outreach program included interactions with several organizations at yearly events and others less systematic but sporadic. During these events, attendees received education on memory disorders, neurodegeneration, and general health concerns common to the geriatric populations. In addition, the principal investigator provided education on risk factors for AD, progress on diagnosis, currently available treatments, and promising preventive strategies. As part of the outreach program, we created sustained alliances. The program includes a Community Alliance for Research Engagement (CARE) group component. This group comprised church leaders in the Washington, DC, metropolitan area who met monthly with the PI and our community outreach team to develop the best strategies for raising awareness in their respective communities. Educational discussions focused on preventing and treating high blood pressure, diabetes, high cholesterol, and memory loss. These alliances occurred mostly in the Howard University geographic region in the District of Columbia and adjacent Prince George’s County, Maryland, that house a predominantly Black population.
Also, the Division of Geriatrics partnered with the Howard University community outreach program and participated in health fairs. Such programs included general health screenings, engagement of seniors and their caregivers, and education on various geriatrics syndromes, including memory loss and AD. We also emphasized the importance of healthy living and emerging preventive strategies for AD. For example, the Washington, DC, Department of Health has over six Senior Wellness Centers where seniors 60 years and older interact and socialize. These centers offer lunch, outings/excursions, computer training, nutrition classes, treadmill exercise, massage, and seminars on health issues affecting their groups and provided education on medication management, health, and other social services issues. The HU community outreach team visited these centers and engaged the attendees through seminars and memory screenings using the MMSE and logical memory to access study eligibility.
Statistical Analysis
To assess the characteristics of the recruited participants by enrollment status, we used descriptive statistics. All analyses were performed using SAS version 9.3 [22] and NCSS Statistical Software [19]. We assessed variables of interest from the Exercise Study for data distribution and the assumption of normality. From this number, twelve participants were excluded at level 1 screening. Of the remaining 555 participants, 62 participants were excluded due to MMSE scores below 24 and age below 55. The remaining data included 493 participants (enrolled = 92; met general inclusion criteria, signed consent form and undergone additional screening; not-enrolled = 401). The baseline descriptive analyses expressed numerical variables as mean and standard deviation or as the number of participants and proportions when categorical. We evaluated for significant differences using Student’s t test for continuous variables and employed a chi-square test to analyze categorical data. We present a boxplot distribution of the age at screening and enrollment status as well as gender categories, comparing the enrolled participants vs. those not-enrolled (those that were not enrolled). In addition, we performed logistic regression analyses to inform the role of transportation and identify demographic and cognitive factors that affected enrollment. All p values were based on a two-tailed test with significance set at p < 0.05 and confidence intervals computed at a 95% confidence level.
Results
Enrollment of Engaged Volunteers
A total of 567 senior residents in the DELMARVA area were engaged as potential volunteers in the exercise study. Of the 567 engaged volunteers, 555 had level 1 screenings, while thirteen had incomplete screening data. Inclusion criteria required participants to have an MMSE score ≥ 24 and aged 55 and above. This resulted in a total of 493 with screening data and 62 excluded from the analysis (inclusion criteria, MMSE scores ≥ 24 and age ≥ 55). Overall, 92 (18.66%) signed the study informed consent, while 401 (81.34%) were not-enrolled because they did not meet the enrollment criteria or were lost to follow-up.
Characteristics of Engaged Volunteers
Among the 493 engaged and considered for the study, 81.34% were AAs or Blacks, 9.33% White, and 6.29% considered other race (Table 1). The mean age of the overall sample at screening was 68.27 (7.57), with enrolled participants being significantly older (mean age 69.67±7.46; p = 0.048) compared to the not-enrolled (mean age = 67.95±7.57). Figure 1 shows the distribution of the screening age by enrollment and gender. Among the enrolled and not-enrolled groups, women constituted a higher percent of the sample (74.24%). Further, the mean MMSE score was significantly higher (p = 0.009) among the enrolled (28.43±1.33) than the not-enrolled (28.00±1.72) participants. The samples were relatively similar in years of educational attainment and logical memory scores (LM1 and LM2).
Given the trend in transportation, the characteristics of participants by enrollment and transportation status were examined. In Table 2, we present the characteristics of the participants by enrollment and transportation. Among enrolled participants, those with transportation were slightly older (mean age 70.58±7.05) than those with no transportation (mean age 66.53±8.36), but the difference did not reach statistical significance (p=0.064). The enrolled participants were relatively similar to the not-enrolled in gender, years of educational attainment, MMSE, and logical memory scores (LM1 and LM2). However, as anticipated and among the not enrolled participants, those with transportation were significantly more educated (mean years of education=13.07±5.53) than those without transportation (mean years of education 10.74±5.36) (p=0.001). Notably, not-enrolled participants with transportation performed better on the MMSE cognitive test and cognitive scores than those without transportation.
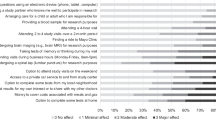
Interestingly, a higher percent of the enrolled participants (79.12%) had access to transportation than the not-enrolled (71.63%). Figure 2 shows the enrolled vs. not-enrolled frequency distribution by transportation and gender (male vs. female). Among female participants, a total of 204 (72.86%) volunteers had transportation while 76 (27.14%) did not, and among male participants, 75 (75.00%) had transportation while 25 (25.00%) did not. Among enrolled female participants, enrolled participants were more likely to have transportation (78.13%) than not-enrolled (71.30%). Conversely, a higher percent (81.48%) of enrolled men had transportation than not-enrolled (72.60%).
Factors Associated with Enrollment
We performed logistic regression analysis to assess the relationships of enrollment status with demographic factors and cognitive scores (Table 3). In the model, age (at screening), education, gender, and cognitive scores (LM1 and LM2) were not significantly different among those enrolled compared to those not-enrolled. However, differences in access to transportation were not statistically significant (p = 0.088) between groups. Participants who had access to transportation were more likely to be enrolled.
Factors Associated with Transportation
We performed a logistic regression analysis to evaluate potential demographic and race factors that may influence transportation in our sample (Table 4). In the unadjusted model, AAs were less likely to have means of transportation compared to the white volunteers (p = 0.035). Additionally, participants categorized as “others” (Asian, Hispanic, Islander Latino, and Native Americans) combined due to small sample were less likely to have transportation compared to the AAs (p = 0.007). The associations remain consistent after adjusting for age at screening, gender, and education, with AAs still less likely to have transportation than Whites (p = 0.020) but more likely to have transportation than others (p = 0.003). Participants with higher levels of education were more likely to have transportation as well (p = 0.0006).
Discussion
This study examined factors influencing enrollment into a biomedical study in a predominantly AA sample, primarily focusing on transportation. Among the demographic factors, age at screening, education, gender, and cognitive scores (logical memory 1 and 2) were not significantly different among those enrolled compared to those not-enrolled. Overall, transportation was not statistically significantly associated with enrolled status though more enrolled participants had access to transportation than not-enrolled participants. However, an important finding was that enrolled AAs were less likely to have transportation than “Whites” but more likely than “others” category. Similarly, education appeared to be a proxy marker for transportation -- Those with higher levels of education have more transportation.
Our study included a predominantly AA sample with more women than men volunteers. Graham et al. [14] noted that particularly, AA women are motivated to participate in health-related research because of altruism, monetary, and other compensations [14]. Our current study focused on elderly AA population, average age ~70 years. Notably, enrolled volunteers were relatively more educated and performed better on the cognitive assessment tasks (MMSE scores) than the not-enrolled group. Interestingly, those having transportation were more educated (higher years of education) than those without transportation in the not-enrolled group. Potentially, this may have been motivated by a greater sense of altruism and willingness to participate in research among the older (older old) versus younger (young–old) volunteers. Further, not-enrolled participants with transportation (have transportation) performed better on the MMSE than those with no transportation (have no transportation), suggesting that driving and navigating may have cognitive benefits. An interesting and potentially cognitive benefit of navigating ability is supported by Maguire et al. [26], who showed that structural MRIs of the brains of humans with extensive navigation experience (licensed London taxi drivers) had significantly larger posterior hippocampi than control subjects [26].
While the enrollment of elderly AAs into studies on Alzheimer’s disease and related disorders remains relatively low, the role of transportation in the under-enrollment of this population has not been fully elucidated. An important observation from this study is that AAs in our sample were less likely to have transportation than Whites. This indicates that transportation may be an important mediator of lower participation of AAs compared to Whites in clinical translational research. Few studies have examined the role of transportation as a conduit to participation in research. For example, Fox [10], in a survey to assess the need for transportation infrastructure, contacted 843 clinical trial sites in the USA to understand how transportation access impacted participant recruitment and enrollment and the type of transportation participants found most helpful. Of the 49 sites that responded, 95% reported that transportation infrastructure would improve recruitment efforts, and 63% felt it would ensure all studies recruited on time. Eighty-four percent of respondents reported that a taxi or ride-sharing service partnership would be the preferred transportation infrastructure. Also, Frank et al. [11] indicated that individuals who live farther from the clinical trial site seem more likely to accept rides, suggesting that transportation infrastructure may help clinical trial sites engage with harder-to-reach populations and broaden their recruitment networks [11]. These observations are congruent with our findings that transportation may be a likely catalyst to study enrollment. Unfortunately, the importance of transportation is yet to be fully appreciated by study teams. For example, Sertkaya et al. [34] pointed out that coordinators spend minimal time and effort coordinating rides, though patient satisfaction surveys suggest that the service would greatly benefit study participants [34]. Thus, education of staff together with the provision of transportation services may yet enhance study enrollment and reduce attrition, especially in under-resourced AA and other underrepresented groups.
While acknowledging known barriers, we must continuously strive to identify hidden ones and develop new strategies to overcome them. The barriers and influencers of enrollment in biochemical trials among low income, disadvantaged AA groups have been reported by other groups [4, 12, 16, 18, 20, 23, 33, 36]. Given the acknowledged barriers, efforts to dismantle these impediments to scientific progress must be deliberate and continuous. Notably, the under-representation of racial and underrepresented groups would limit the generalizability of research findings. In addition, under-enrollment of racial and ethnic underrepresented groups in clinical trials may also contribute to preventable disparities in treatment outcomes and survival [5]. Amorrortu et al. [3] suggested the need for recruitment strategies that facilitate referrals from physicians outside of the specialty clinics who may see a higher proportion of underrepresented groups of patients [3]. This approach will allow a broader cross-section of these groups to be exposed to available clinical trials. In a survey of 70,000 research volunteers, Alexander-Bridges and Doan [2] reported that underrepresented volunteers were just as likely as majority volunteers to participate in clinical research when approached by their own physicians [2]. Furthermore, while it is believed that underrepresented volunteers fail to participate in trials because of distrust for research and researchers, others have suggested that an additional limiting factor is that underrepresented groups are not routinely asked to participate [9] in clinical studies. Nonetheless, our findings from this study suggest that lack of transportation is yet another puzzle in the barriers to participation in clinical research.
Other factors that are not characterized as transportation may yet serve as proxies for transportation, influence volunteers satisfaction and delay enrollment and timely completion of clinical studies. Estimates of the number of trials that fail to meet scientific objectives because of insufficient accrual rates range from 22 to 50% [27]. Low accrual rates jeopardize the ability of researchers to assess the safety and effectiveness of new approaches to medical care, waste resources, delay follow-up studies, and translation of research into evidence-based practice [25]. Despite the National Institutes of Health requirement that members of underrepresented populations be included in clinical research [15], under-enrollment from lack of transportation is even more significant for economically disadvantaged vulnerable populations such as African Americans. Other factors such as the attitude of research staff have been noted to influence volunteers satisfaction. Also, Adler et al. [1] reported that satisfaction and positive attitudes of research staff and specific trials were important determinants for enrollment, completion, and participation in clinical trials. Additionally, given the importance of cultural competence to the successful design and implementation of a given study, Otado et al. [28] suggested that research teams should consist of multiethnic staff, involve the community, demonstrate trust, and deliver concise education to prospective study volunteers [28]. In addition to lack of transportation to clinic locations for study visits, Kalbaugh et. al. [24] noted that others were unable to accommodate schedule visits. The most significant gap was seen for AA and Hispanics with less than a high school education and people earning less than $25,000 annually. This result is consistent with our findings that AAs are less likely to have the transportation needed to enable their participation in clinical studies. Our finding from the current study suggests that targeting older AA with access to transportation may increase recruitment given that the convenience of transportation would promote compliance. Alternatively, study budgets that include support and provision for transportation or embedding clinical trial centers in the community may help ameliorate the barriers posed by lack of transportation. Some of the limitations of this study included the fact that we did not examine the role of cultural sensitivity, compensation, missing demographic data, and other factors that may additionally influence enrollment and retention. We hope to investigate these factors in future studies.
Conclusion
Our findings suggest transportation may be a key factor mediating the recruitment and enrollment of elderly AAs in an exercise study on AD. Particularly, elderly AAs and other underrepresented minority groups who may live farther from the clinical trial site may be lacking transportation and perhaps more inclined to accept rides. Therefore, a transportation infrastructure may help clinical trial sites engage harder-to-reach populations. The availability and convenience of transportation may broaden recruitment networks, mitigate study recruitment and enrollment, and promote compliance. A larger sample is needed to further discern the role of transportation in clinical trials on AD.
Abbreviations
- AA:
-
African Americans
- AD:
-
Alzheimer’s disease
- GEMS:
-
Gene, exercise, and memory study
- LM:
-
Logical memory
- MMSE:
-
Mini–Mental State Examination
- CARE:
-
Community Alliance for Research Engagement
References
Adler P, Otado J, Kwagyan J. Satisfaction and perceptions of research participants in clinical and translational studies: an urban multi-institution with CTSA. J Clin Transl Sci. 2020;4(4):317–22.
Alexander-Bridges M, Doan LL. Commentary on “increasing minority participation in clinical research”: a white paper from the endocrine society. J Clin Endocrinol Metab. 2007;92(12):4557–9.
Amorrortu RP, Arevalo M, Vernon SW, Mainous AG, Diaz V, McKee MD, et al. Recruitment of racial and ethnic minorities to clinical trials conducted within specialty clinics: an intervention mapping approach. Trials. 2018;19(1):1–10.
Baquet CR, Commiskey P, Mullins CD, Mishra SI. Recruitment and participation in clinical trials: socio-demographic, rural/urban, and health care access predictors. Cancer Detect Prev. 2006;30(1):24–33.
Branson RD, Davis K Jr, Butler KL. African Americans’ participation in clinical research: importance, barriers, and solutions. Am J Surg. 2007;193(1):32–9.
Cook ED, Arnold KB, Hermos JA, McCaskill-Stevens W, Moody-Thomas S, Probstfield JL, et al. Impact of supplemental site grants to increase African American accrual for the selenium and vitamin E cancer prevention trial. Clin Trials. 2010;7(1):90–9.
Corbie-Smith G, Miller WC, Ransohoff DF. Interpretations of ‘appropriate’ minority inclusion in clinical research. Am J Med. 2004;116(4):249–52.
Ejiogu N, Norbeck JH, Mason MA, Cromwell BC, Zonderman AB, Evans MK. Recruitment and retention strategies for minority or poor clinical research participants: lessons from the healthy aging in neighborhoods of diversity across the life span study. Gerontologist. 2011;51(suppl_1):S33–45.
Epstein AM. Health care in America—still too separate, not yet equal. N Engl J Med. 2004;351(6):603–5.
Fox MJ. Accelerating clinical trials: best practices for recruitment and retention. The Michael J. Fox Foundation for Parkinson’s Research. 2018.
Frank S, Berk S, Hernandez L, Hogarth P, Shill HA, Siddiqi B, Simon DK. Transportation innovation to aid Parkinson disease trial recruitment. Contemp Clin Trials Commun. 2019;16:100449.
Friedman DB, Foster C, Bergeron CD, Tanner A, Kim S-H. A qualitative study of recruitment barriers, motivators, and community-based strategies for increasing clinical trials participation among rural and urban populations. Am J Health Promot. 2015;29(5):332–8.
George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16–31.
Graham LA, Ngwa J, Ntekim O, Ogunlana O, Wolday S, Johnson S, et al. Best strategies to recruit and enroll elderly Blacks into clinical and biomedical research. Clin Interv Aging. 2018;13:43–50. https://doi.org/10.2147/CIA.S130112.
Gross CP, Filardo G, Mayne ST, Krumholz HM. The impact of socioeconomic status and race on trial participation for older women with breast cancer. Cancer. 2005;103(3):483–91.
Halverson CM, Ross LF. Engaging African-Americans about biobanks and the return of research results. J Commun Genet. 2012;3(4):275–83.
Hamel LM, Penner LA, Albrecht TL, Heath E, Gwede CK, Eggly S. Barriers to clinical trial enrollment in racial and ethnic minority patients with cancer. Cancer Control. 2016;23(4):327–37.
Heredia NI, Krasny S, Strong LL, Von Hatten L, Nguyen L, Reininger BM, et al. Community perceptions of biobanking participation: a qualitative study among Mexican-Americans in three Texas cities. Public Health Genomics. 2017;20(1):46–57.
NCSS 9 Statistical Software. NCSS, LLC. Kaysville, Utah, USA. 2013. www.ncss.com/software/ncss. Accessed Feb 2021.
Howerton MW, Gibbons MC, Baffi CR, Gary TL, Lai GY, Bolen S, et al. Provider roles in the recruitment of underrepresented populations to cancer clinical trials. Cancer. 2007;109(3):465–76.
Indorewalla KK, O’Connor MK, Budson AE, Jackson J. Modifiable barriers for recruitment and retention of older adults participants from underrepresented minorities in Alzheimer’s disease research. J Alzheimers Dis. 2021;80(3):927–40.
SAS Institute. SAS/IML 9.3 user's guide. Sas Institute. Chicago. 2011.
Jones RA, Steeves R, Williams I. Strategies for recruiting African American men into prostate cancer screening studies. Nurs Res. 2009;58(6):452.
Kalbaugh CA, Kalbaugh JM, McManus L, Fisher JA. Healthy volunteers in US phase I clinical trials: sociodemographic characteristics and participation over time. PLoS One. 2021;16(9):e0256994.
Lurie N. Health disparities—less talk, more action. N Engl J Med. 2005;353(7):727–9.
Maguire EA, Gadian DG, Johnsrude IS, Good CD, Ashburner J, Frackowiak RS, Frith CD. Navigation-related structural change in the hippocampi of taxi drivers. Proc Natl Acad Sci. 2000;97(8):4398–403.
McDonald M. Medical research and ethnic minorities. Postgrad Med J. 2003;79(929):125–6.
Otado J, Kwagyan J, Edwards D, Ukaegbu A, Rockcliffe F, Osafo N. Culturally competent strategies for recruitment and retention of African American populations into clinical trials. Clin Transl Sci. 2015;8(5):460–6.
Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–94.
Risch N. Dissecting racial and ethnic differences. N Engl J Med. 2006;354(4):408–11.
Rivers D, August EM, Sehovic I, Green BL, Quinn GP. A systematic review of the factors influencing African Americans' participation in cancer clinical trials. Contemp Clin Trials. 2013;35(2):13–32.
Salman A, Nguyen C, Lee Y-H, Cooksey-James T. A review of barriers to minorities’ participation in cancer clinical trials: implications for future cancer research. J Immigr Minor Health. 2016;18(2):447–53.
Sanderson SC, Diefenbach MA, Zinberg R, Horowitz CR, Smirnoff M, Zweig M, et al. Willingness to participate in genomics research and desire for personal results among underrepresented minority patients: a structured interview study. J Commun Genet. 2013;4(4):469–82.
Sertkaya A, Wong H-H, Jessup A, Beleche T. Key cost drivers of pharmaceutical clinical trials in the United States. Clin Trials. 2016;13(2):117–26.
Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethn Health. 1997;2(1-2):31–45.
Streicher SA, Sanderson SC, Jabs EW, Diefenbach M, Smirnoff M, Peter I, et al. Reasons for participating and genetic information needs among racially and ethnically diverse biobank participants: a focus group study. J Commun Genet. 2011;2(3):153–63.
Acknowledgements
We thank all our colleagues working at the Division of Geriatrics, Department of Medicine and Clinical/Translational Science Program, Howard University Hospital. Thanks to Saba Wolday for her unwavering support for this study and others.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (NIH) grant R01 5R01AG031517 to Obisesan TO and R01-AG045058 to Obisesan TO by the NIA. The funders had no role in the design, data collection, and interpretation of this study
Author information
Authors and Affiliations
Contributions
LG, JSN, TVF, and TOO participated in the design and performed the statistical analysis. LG, JSN, TVF, and TOO conceived the analyses, participated in its design and coordination, and helped draft the manuscript. All authors participated in reviewing the final manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The Howard University Institutional Review Board (IRB) approved the protocol before study initiation. In addition, all participants signed a consent form.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Graham, L., Ngwa, J., Ntekim, O. et al. The Role of Transportation in the Enrollment of Elderly African Americans into Exercise and Memory Study: GEMS Study. J. Racial and Ethnic Health Disparities 10, 1837–1845 (2023). https://doi.org/10.1007/s40615-022-01367-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01367-7