Abstract
Objective
Adult cardiovascular disease has its roots in childhood and adolescence. Risks for pediatric hypertension include obesity, male sex, and minority race. We identified risk factors associated with hypertension specifically among African American adolescents ages 13–18.
Methods
We analyzed data from the US National Health and Nutrition Examination Surveys from 2011 to 2018, defining BP consistent with hypertension as average systolic or diastolic BP ≥ 130/80 mmHg or taking medication for a clinical diagnosis of hypertension. Univariate analyses compared characteristics of adolescents with and without hypertensive-level BP. Logistic regression was completed to more precisely identify risk factors.
Results
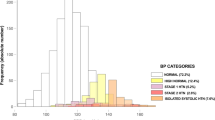
Among 838 African American adolescents, 48 met criteria for hypertensive-level BP, for a population prevalence of 5.8%. Due to low rates of hypertensive-level BP in girls (2.7%), our analysis focused on the subset of boys, who had an 8.9% prevalence rate, increasing to 26.1% for boys with obesity and 35.3% for boys with severe obesity. Boys with hypertensive-level BP had significantly lower family incomes, higher rates of being in single-parent families, more frequent consumption of fast food, were more likely to be taking prescription medications for psychiatric diagnoses, and had higher A1c and cholesterol values.
Conclusions
Our study confirms the much higher risk for hypertensive-level BP in African American boys and emphasizes the important role of social determinants of health in this common illness.
Similar content being viewed by others
Data Availability
The data used in analysis for this manuscript is publicly available from the National Center for Health Statistics of the US Centers for Disease Control and Prevention.
References
Musemwa N, Gadegbeku CA. Hypertension in African Americans. Curr Cardiol Rep. 2017;19(12):129. https://doi.org/10.1007/s11886-017-0933-z.
Ruiz LD, Zuelch ML, Dimitratos SM, Scherr RE. Adolescent obesity: diet quality, psychosocial health, and cardiometabolic risk factors. Nutrients. 2019;12(1):43. https://doi.org/10.3390/nu12010043.
Gartlehner G, Vander Schaaf EB, Orr C, Kennedy SM, Clark R, Viswanathan M. Screening for hypertension in children and adolescents: updated evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2020;324(18):1884–95. https://doi.org/10.1001/jama.2020.11119.
Rao G. Diagnosis, epidemiology, and management of hypertension in children. Pediatrics. 2016;138(2):e20153616. https://doi.org/10.1542/peds.2015-3616.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM. Subcommittee on screening and management of high blood pressure in children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. https://doi.org/10.1542/peds.2017-1904.
Sharma AK, Metzger DL, Rodd CJ. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics guidelines. JAMA Pediatr. 2018;172(6):557–65. https://doi.org/10.1001/jamapediatrics.2018.0223.
Bell CS, Samuel JP, Samuels JA. Prevalence of hypertension in children: applying the new American academy of pediatrics clinical practice guideline. Hypertension. 2019;73(1):148–52. https://doi.org/10.1161/hypertensionaha.118.11673.
Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373(14):1307–17. https://doi.org/10.1056/NEJMoa1502821.
Margerison CE, Catov J, Holzman C. Pregnancy as a window to racial disparities in hypertension. J Womens Health (Larchmont). 2019;28(2):152–61.
Chen L, Simonsen N, Liu L. Racial differences of pediatric hypertension in relation to birth weight and body size in the United States. PLoS ONE. 2015;10(7):e0132606. https://doi.org/10.1371/journal.pone.0132606.
Lamotte C, Iliescu C, Libersa C, Goltrand F. Increased intima-media thickness of the carotid artery in childhood: a systematic review of observational studies. Eur J Pediatr. 2011;170(6):719–29. https://doi.org/10.1007/s00431-010-1328-y.
Mitchell P, Cheung N, de Haseth K, Taylor B, Rochtchina E, Islam FMA, Wang JJ, Saw SM, Wong TY. Blood pressure and retinal arteriolar narrowing in children. Hypertension. 2007;49:1156–62. https://doi.org/10.1161/HYPERTENSIONAHA.106.085910.
Biggazzi R, Bianchi S, Baldari D, Campese VM. Microalbuminuria predicts cardiovascular events and renal insufficiency in patients with essential hypertension. J Hypertens. 1998;16:1325–33. https://doi.org/10.1097/00004872-199816090-00014.
Kavey REW. Left ventricular hypertrophy in hypertensive children and adolescents: predictors and prevalence. Curr Hypertens Rep. 2013;15:453–7. https://doi.org/10.1111/jch.13540.
Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am J Hypertens. 1995;8(7):657–65. https://doi.org/10.1016/0895-7061(95)00116-7.
Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, Cutfield W, Williams MJA, Harrington H, Moffitt TE, Caspi A, Milne B, Poulton R. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66(6):1108–15. https://doi.org/10.1161/HYPERTENSIONAHA.115.05831.
Hao G, Wang X, Treiber FA, Harshfield G, Kapuku G, Su S. Blood pressure trajectories from childhood to young adulthood associated with cardiovascular risk: results from the 23-year longitudinal Georgia Stress and Heart Study. Hypertension. 2017;69(3):435–42. https://doi.org/10.1161/HYPERTENSIONAHA.116.08312.
Taylor-Zapata P, Baker-Smith CM, Burckart G, Daniels SR, Flynn JT, Giacoia G, Green D, Kelly AS, Khurana M, Li JS, Pratt C, Urbina EM, Zajicek A. Research gaps in primary pediatric hypertension. Pediatrics. 2019;143(5):e20183517. https://doi.org/10.1542/peds.2018-3517.
Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298(8):874–9. https://doi.org/10.1001/jama.298.8.874.
Centers for disease control and prevention. National Center for Health Statistics. National health and nutrition examination survey methods and analytic guidelines. https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx. Accessed 15 Mar 2021.
Barlow SE, Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Supplment 4):S164–92. https://doi.org/10.1542/peds.2007-2329C.
Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd ed. New York: Wiley; 2013.
Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873–98. https://doi.org/10.1161/CIR.0000000000000228.
Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. https://doi.org/10.1016/j.socscimed.2013.04.026.
Larson S, Chapman S, Spetz J, Brindis CD. Chronic childhood trauma, mental health, academic achievement, and school-based health center mental health services. J Sch Health. 2017;87(9):675–86. https://doi.org/10.1111/josh.12541.
Noonan RJ. The effect of childhood deprivation on weight status and mental health in childhood and adolescence: longitudinal findings of the millennium cohort study. J Public Health (Oxf). 2019;41(3):456–61. https://doi.org/10.1093/pubmed/fdy139.
Hamdani G, Flynn JT, Becker RC, et al. Prediction of ambulatory hypertension based on clinic blood pressure percentile in adolescents: the SHIP AHOY study. Hypertension. 2018;72(4):955–61. https://doi.org/10.1161/HYPERTENSIONAHA.118.11530.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study conception and design. Data collection, coding, and analysis were performed by Susan Connor, with input on study design, coding parameters, application of clinical guidelines, and interpretation of results from Goutham Rao. The first draft of the manuscript was written by Susan Connor, with subsequent comments and revisions by both Goutham Rao and Susan Connor. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rao, G., Connor, S. Correlates of Hypertensive-Level BP in African American Adolescents. J. Racial and Ethnic Health Disparities 10, 536–541 (2023). https://doi.org/10.1007/s40615-022-01243-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01243-4