Abstract
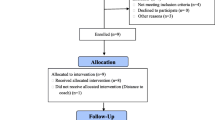
This study examined how a racially and socioeconomically diverse group of caregivers of children with autism spectrum disorder (ASD) responds to national standard measures of family-centered care (FCC) and care coordination (CC) and what aspects of quality care are missing from these measures. Based on survey and interview data collected from 70 caregivers who have a child with ASD that receive services at a community-based autism clinic located in Atlanta, GA, we compared proportions of answers to FCC and CC questions to national and state representative data using chi-square analyses and contextualized our findings through a thematic analysis of qualitative interviews. Compared to national- and state-level data, the Atlanta autism clinic data had a higher percentage of participants who identified as Black, relied on public health insurance, and lived below 200% of the federal poverty line. The Atlanta autism clinic responses were significantly more positive in four measures of FCC but significantly less effective in two CC measures, including a lower reported percentage who received CC and greater reported percentage who needed extra help. Qualitative data revealed a range of positive meanings and challenges associated with FCC and identified areas of help needed beyond CC, including physical and mental health care and emotional connection, especially for low-income single Black female caregivers. Our mixed-method approach identified strengths in FCC, barriers to CC, and suggestions for developing more pragmatic questions in national surveys that address experiences of quality-of-care among low-income, racial minority families of children with ASD.
Similar content being viewed by others
References
Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Review Clin Child Fam Psychol Rev. 2000;15:247–77. https://doi.org/10.1007/s10567-012-0119-6.
Bramlett MD, Blumberg SJ, Ormson AE, George JM, Williams KL, Frasier AM, et al. Design and operation of the National Survey of Children with Special Health Care Needs, 2009-2010. Vital Health Stat 1. 2014;57:1–271.
The Child and Adolescent Health Measurement Initiative, Johns Hopkins Bloomberg School of Public Health. Experience matters: a view into the health and wellbeing of US children and families with autism spectrum disorder (ASD). 2016. https://childhealthdata.org/docs/default-source/cahmi/asdchartbookfinal.pdf?sfvrsn=2. Accessed 23 May 2020.
Vanegas SB, Abdelrahim R. Characterizing the systems of support for families of children with disabilities: a review of the literature. J Fam Soc Work. 2016;19:286–327. https://doi.org/10.1080/10522158.2016.1218399.
Benevides TW, Carretta HJ, Lane SJ. Unmet need for therapy among children with autism spectrum disorder: results from the 2005-2006 and 2009-2010 National Survey of Children with Special Health Care Needs. Matern Child Health J. 2016;20:878–88. https://doi.org/10.1007/s10995-015-1876-x.
Austin J, Manning-Courtney P, Johnson ML, Weber R, Johnson H, Murray D, et al. Improving access to care at autism treatment centers: a system analysis approach. Pediatrics. 2016;137:S149–57. https://doi.org/10.1542/peds.2015-2851M.
Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168:721–8. https://doi.org/10.1001/jamapediatrics.2014.210.
Christon LM, Myers BJ. Family-centered care practices in a multidisciplinary sample of pediatric professionals providing autism spectrum disorder services in the United States. Res Autism Spectr Disord. 2015;20:47–57. https://doi.org/10.1016/j.rasd.2015.08.004.
Zhang W, Baranek G. The impact of insurance coverage types on access to and utilization of health services for US children with autism. Psychiatr Serv. 2016;67:908–11. https://doi.org/10.1176/appi.ps.201500206.
Maenner MJ, Shaw KA, Bak J, Washington A, Patrick M, DiRienzo M, et al. Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ. 2020. https://doi.org/10.15585/mmwr.ss6904a1.
Durkin MS, Maenner MJ, Baio J, Christensen D, Daniels J, Fitzgerald R, et al. Autism spectrum disorder among US children (2002-2010): socioeconomic, racial, and ethnic disparities. Am J Public Health. 2017;107:1818–26. https://doi.org/10.2105/AJPH.2017.304032.
Bishop-Fitzpatrick L, Kind AJH. A scoping review of health disparities in autism spectrum disorder. J Autism Dev Disord. 2017;47:3380–91. https://doi.org/10.1007/s10803-017-3251-9.
Kalb LG, Freedman B, Foster C, Menon D, Landa R, Kishfy L, et al. Determinants of appointment absenteeism at an outpatient pediatric autism clinic. J Dev Behav Pediatr. 2012;33:685–97. https://doi.org/10.1097/DBP.0b013e31826c66ef.
Constantino JN, Abbacchi AM, Saulnier C, Klaiman C, Mandell DS, Zhang Y, et al. Timing of the diagnosis of autism in African American children. Pediatrics. 2019;146:e20193629. https://doi.org/10.1542/peds.2019-3629.
Bilaver LA, Havlicek J. Racial and ethnic disparities in autism-related health and educational services. J Dev Behav Pediatr. 2019;40:501–10. https://doi.org/10.1097/DBP.0000000000000700.
Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism. 2014;18:583–97. https://doi.org/10.1177/1362361313480277.
Longtin SE, Principe GM. The relationship between poverty level and urban African American parents’ awareness of evidence-based interventions for children with autism spectrum disorders: preliminary data. Focus on Autism and Other Dev Disabl. 2016;31:83–91. https://doi.org/10.1177/1088357614522293.
Magnusson DM, Mistry KB. Racial and ethnic disparities in unmet need for pediatric therapy services: the role of family-centered care. Acad Pediatr. 2017;17:27–33. https://doi.org/10.1016/j.acap.2016.06.010.
Zuckerman KE, Mattox KM, Sinche BK, Blaschke GS, Bethell C. Racial, ethnic, and language disparities in early childhood developmental/behavioral evaluations: a narrative review. Clin Pediatr. 2014;53:619–31. https://doi.org/10.1177/0009922813501378.
Williams DR. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav. 2018;59:466–85. https://doi.org/10.1177/0022146518814251.
Magana S, Parish SL, Son E. Have racial and ethnic disparities in the quality of health care relationships changed for children with developmental disabilities and ASD? Am J Intellect Dev Disabil. 2015;120:504–13. https://doi.org/10.1352/1944-7558-120.6.504.
Montes G, Halterman JS. White-black disparities in family-centered care among children with autism in the United States: Evidence from the NS-CSHCN 2005-2006. Acad Pediatr. 2011;11:297–304. https://doi.org/10.1016/j.acap.2011.02.002.
Bromley J, Hare DJ, Davison K, Emerson E. Mothers supporting children with autistic spectrum disorders-social support, mental health status and satisfaction with services. Autism. 2004;8:409–23. https://doi.org/10.1177/1362361304047224.
Hodgetts S, Nicholas D, Zwaigenbaum L, McConnell D. Parents’ and professionals’ perceptions of family-centered care for children with autism spectrum disorder across service sectors. Soc Sci Med. 2013;96:138–46. https://doi.org/10.1016/j.socscimed.2013.07.012.
Pearson JN, Meadan H, Malone KM, Martin BM. Parent and professional experiences supporting African-American children with autism. J Racial Ethn Health Disparities. 2020;7:305–15. https://doi.org/10.1007/s40615-019-00659-9.
Singh JS, Bunyak G. Autism disparities: a systematic review and meta-ethnography of qualitative research. Qual Health Res. 2019. https://doi.org/10.1177/1049732318808245.
Creswell J, Creswell J. Research design: qualitative, quantitative, and mixed methods approaches. 5th ed. Los Angeles, CA: Sage; 2018.
Centers for Disease Control and Prevention National Center for Health Statistics. (2011). 2009-2010 National Survey of Children with Special Health Care Needs Questionnaire Version: December 14, 2011. https://www.cdc.gov/nchs/slaits/cshcn.htm. Accessed 25 May 2020.
HyperRESEARCH 3.7.5. Computer Software. Researchware, Inc. 2015.
Department of Health and Human Services Office of the Secretary. Annual update of the HHS poverty guidelines: a notice by the Health and Human Services Department on 01/18/2018. In Department of Health and Human Services (Ed.). 2018. Federal Register. https://www.federalregister.gov/documents/2018/01/18/2018-00814/annual-update-of-the-hhs-poverty-guidelines. Accessed 25 May 2020.
Centers for Disease Control and Prevention National Center for Health Statistics State and Local Area Integrated Telephone Survey. 2009-2010 National Survey of Children with Special Health Care Needs Frequently Asked Questions. https://www.cdc.gov/nchs/slaits/cshcn.htm. Accessed on 28 May 2020.
SAS Software Version 9.4. Copyright © 2013. SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39:124–30. https://doi.org/10.1207/s15430421tip3903_2.
Minkler M, Fuller-Thomson E. African American grandparents raising grandchildren: a national study using the Census 2000 American Community Survey. J Gerontol Ser B-Psychol Sci Soc Sci. 2005;60:S82–92. https://doi.org/10.1093/geronb/60.2.s82.
Denboba D, McPherson MG, Kenney MK, Strickland B, Newacheck PW. Achieving family and provider partnerships for children with special health care needs. Pediatrics. 2006;118:1607–15. https://doi.org/10.1542/peds.2006-0383.
Debabanah S, Shaia WE, Campion K, Nichols HM. “We had to keep pushing”: Caregivers’ perspectives on autism screening and referral practices of Black children in primary care. Intellect Dev Disabil. 2018. https://doi.org/10.1352/1934-9556-56.5.321.
Burkett K, Morris E, Manning-Courtney P, Anthony J, Shambley-Ebron D. African American families on autism diagnosis and treatment: the influence of culture. J Autism Dev Disord. 2015;45:3244–54. https://doi.org/10.1007/s10803-015-2482-x.
Hong A, Singh JS. Contextualizing the social and structural constraints of accessing autism services among single Black female caregivers in Atlanta, Georgia. Int J Child Health Hum Dev. 2019;12(4):365–378.
Pearson JN, Meadan H. African American parents’ perceptions of diagnosis and services for children with autism. Educ Train Autism Dev Disabil. 2018. https://doi.org/10.2307/26420424.
Hodgetts S, McConnell D, Zwaigenbaum L, Nicholas D. The impact of autism services on mothers’ psychological wellbeing. Child Care Health Dev. 2017;43:18–30. https://doi.org/10.1111/cch.12398.
Hodgetts S, Zwaigenbaum L, Nicholas D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism. 2015;19:673–83. https://doi.org/10.1177/1362361314543531.
Carr T, Lord C. A pilot study promoting participation of families with limited resources in early autism intervention. Res Autism Spectr Disord. 2016;25:87–96. https://doi.org/10.1016/j.rasd.2016.02.003.
Hyman SL, Levy SE, Myers SM, Kuo DZ, Apkon S, Davidson LF, et al. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020;145:e20193447. https://doi.org/10.1542/peds.2019-3447.
Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee. Patient- and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics. 2013. https://doi.org/10.1542/peds.2014-0318.
Cheak-Zamora NC, Farmer JE. The impact of the medical home on access to care for children with autism spectrum disorders. J Autism Dev Disord. 2015;45:636–44. https://doi.org/10.1007/s10803-014-2218-3.
Carbone PS, Behl DD, Azor V, Murphy NA. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. 2010;40:317–24. https://doi.org/10.1007/s10803-009-0874-5.
Jarquin VG, Wiggins LD, Schieve LA, Van Naarden-Braun K. Racial disparities in community identification of autism spectrum disorders over time; metropolitan Atlanta, Georgia, 2000-2006. J Dev Behav Pediatr. 2011;32:179–87. https://doi.org/10.1097/DBP.0b013e31820b4260.
Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51:S15–27. https://doi.org/10.1177/0022146510383838.
Acknowledgements
We would like to express our gratitude to all the women in this study who contributed their valuable time and energy of telling their stories about navigating ASD services, as well as the staff and clinical professionals at the Autism Clinic at Hughes Spalding Children’s Hospital.
Availability of Data and Material
Not available
Code Availability
Not applicable
Funding
This study was supported by a research partnership between Children’s Healthcare of Atlanta and the Georgia Institute of Technology. Funding was also provided by the Ivan Allen College of Liberal Arts, Georgia Institute of Technology.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jennifer S. Singh (qualitative) and Stephanie Wagner (quantitative). The first draft of the manuscript was written by Stephanie Wagner and Jennifer S. Singh, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Approval was obtained from the Institutional Review Boards of Children’s Healthcare of Atlanta (#16-099), Georgia Institute of Technology, and Morehouse School of Medicine, as well as the Grady Research Oversight Committee. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Participants signed informed consent regarding publishing their data. All the participants were given a pseudonym in the presentation of our findings to protect their identity.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wagner, S., Rubin, I.L. & Singh, J.S. Underserved and Undermeasured: a Mixed-Method Analysis of Family-Centered Care and Care Coordination for Low-Income Minority Families of Children with Autism Spectrum Disorder. J. Racial and Ethnic Health Disparities 9, 1474–1487 (2022). https://doi.org/10.1007/s40615-021-01086-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01086-5