Abstract
Background
Shared decision-making (SDM) is recommended for prostate cancer screening, but little is known about how this process is perceived by patients and providers. SDM is especially important for African American men, who are at high risk for the disease.
Objective
To evaluate agreement in SDM ratings among patients, providers, and objective observers.
Method
African American men ages 45–70 were recruited from primary care practices to participate in a study evaluating a decision aid (DA). Immediately after using the DA, patients proceeded to primary care appointments. Afterwards, patients and physicians completed surveys assessing perceptions about SDM. Clinical visits were also audio-recorded and coded to assess SDM.
Results
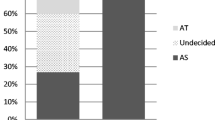
Mean scores on SDM measures among patients were 73.2 (SD = 27.5, 95% CI 55.71–90.62), 83.1 among physicians (SD = 7.8 95% CI 78.14–88.06), and 67.1 among objective raters (SD = 36.8 95% CI 43.72–90.45). Among patient-provider dyads, mean agreement was 49.9%.
Conclusion
Patients, physicians, and objective observers perceived SDM differently. Understanding discordant experiences of SDM is vital for improving clinical guidance about SDM especially among African Americans who have historically faced healthcare discrimination and mistrust. DAs, particularly for African American men, should incorporate strategies to empower patients to advocate for their communication needs and preferences.
Trial Registration
Clinical trials identifier number: NCT02787434


Similar content being viewed by others
Data Availability/Transparency
The dataset generated and analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
- PSA:
-
prostate-specific antigen
- DA:
-
decision aid
- SDM:
-
shared decision-making
References
American Cancer Society. Cancer Facts and Statistics [Internet]. [cited 2019 Mar 4].
Bernal-Soriano MC, Parker LA, López-Garrigos M, Hernández-Aguado I, Caballero-Romeu JP, Gómez-Pérez L, et al. Factors associated with false negative and false positive results of prostate-specific antigen (PSA) and the impact on patient health: cohort study protocol. Medicine. 2019;98(40).
U.S. Preventive Services Task Force. Final Recommendation Statement: Prostate Cancer: Screening 2018 [cited 2019 Aug 6].
American Cancer Society (ACS). American Cancer Society Recommendations for Prostate Cancer Early Detection [cited 2020 Jun 2]. .
Briss P, Rimer B, Reilley B, Coates RC, Lee NC, Mullen P, et al. Promoting informed decisions about cancer screening in communities and healthcare systems. Am J Prev Med. 2004;26(1):67–80.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7.
Cooper DL, Rollins L, Slocumb T, Rivers BM. Are men making informed decisions according to the prostate-specific antigen test guidelines? Analysis of the 2015 behavioral risk factor surveillance system. Am J Mens Health. 2019;13(2):1557988319834843.
Calderon C, Jiménez-Fonseca P, Ferrando PJ, Jara C, Lorenzo-Seva U, Beato C, et al. Psychometric properties of the Shared Decision-Making Questionnaire (SDM-Q-9) in oncology practice. Int J Clin Health Psychol. 2018;18(2):143–51.
Scholl I, Kriston L, Dirmaier J, Buchholz A, Härter M. Development and psychometric properties of the Shared Decision Making Questionnaire–physician version (SDM-Q-Doc). Patient Educ Couns. 2012;88(2):284–90.
Weeks JC, Cook EF, O'Day SJ, Peterson LM, Wenger N, Reding D, et al. Relationship between cancer patientsʼ predictions of prognosis and their treatment preferences. Jama. 1998;279(21):1709–14.
Brown R, Butow P Fau, Wilson-Genderson M, Wilson-Genderson M Fau, Bernhard J, Bernhard J Fau, Ribi K, Ribi K Fau, Juraskova I, Juraskova I. Meeting the decision-making preferences of patients with breast cancer in oncology consultations: impact on decision-related outcomes. (1527-7755 (Electronic)).
Arnett MJ, Thorpe RJ, Gaskin DJ, Bowie JV, LaVeist TA. Race, medical mistrust, and segregation in primary care as usual source of care: findings from the exploring health disparities in integrated communities study. J Urban Health. 2016;93(3):456–67.
Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. 2000.
Leyva B, Persoskie A, Ottenbacher A, Hamilton JG, Allen JD, Kobrin SC, et al. Do men receive information required for shared decision making about PSA testing? Results from a national survey. J Cancer Educ. 2016;31(4):693–701.
Allen JD, Filson CP, Berry DL. Effect of a prostate cancer screening decision aid for African-American men in primary care settings. Cancer Epidemiology and Prevention Biomarkers. 2020.
Allen JD, Reich A, Cuevas AG, Ladin K. Preparing African American men to make informed prostate cancer screening decisions: development and pilot testing of an interactive online decision aid. JMIR mHealth and uHealth. 2020;8(5):e15502.
Elwyn G, Hutchings H, Edwards A, Rapport F, Wensing M, Cheung WY, et al. The OPTION scale: measuring the extent that clinicians involve patients in decision-making tasks. Health Expect. 2005;8(1):34–42.
Elwyn G, Grande S, Barr P. The observer OPTION5 manual: measuring shared decision making by assessing recordings or transcripts of encounters from clinical settings, 2016. Available from: Available from: http://www glynelwyn com/uploads/2/4/0/4/24040341/observeroption5manual_july_13_2016 docx pdf.
Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971;76(5):378–82.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. biometrics. 1977:159–74.
Shabason JE, Mao JJ, Frankel ES, Vapiwala N. Shared decision-making and patient control in radiation oncology: implications for patient satisfaction. Cancer. 2014;120(12):1863–70.
Williams D, Edwards A, Wood F, Lloyd A, Brain K, Thomas N, et al. Ability of observer and self-report measures to capture shared decision-making in clinical practice in the UK: a mixed-methods study. (2044-6055 (Electronic)).
Warlick CA, Berge JM, Ho Y-Y, Yeazel M. Impact of a prostate specific antigen screening decision aid on clinic function. Urology practice. 2017;4(6):448–53.
Wunderlich T, Cooper G, Divine G, Flocke S, Oja-Tebbe N, Stange K, et al. Inconsistencies in patient perceptions and observer ratings of shared decision making: the case of colorectal cancer screening. Patient Educ Couns. 2010;80(3):358–63.
Fernald DH, Coombs L, DeAlleaume L, West D, Parnes B. An assessment of the Hawthorne effect in practice-based research. The Journal of the American Board of Family Medicine. 2012;25(1):83–6.
Dillon EC, Stults CD, Wilson C, Chuang J, Meehan A, Li M, et al. An evaluation of two interventions to enhance patient-physician communication using the observer OPTION5 measure of shared decision making. Patient Educ Couns. 2017;100(10):1910–7.
Bomhof-Roordink H, Gärtner FR, Stiggelbout AM, Pieterse AH. Key components of shared decision making models: a systematic review. BMJ Open. 2019;9(12):e031763.
Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21(6):642–7.
Jolles MP, Richmond J, Thomas KC. Minority patient preferences, barriers, and facilitators for shared decision-making with health care providers in the USA: a systematic review. Patient Educ Couns. 2019;102(7):1251–62.
Peek ME, Quinn MT, Gorawara-Bhat R, Odoms-Young A, Wilson SC, Chin MH. How is shared decision-making defined among African-Americans with diabetes? Patient Educ Couns. 2008;72(3):450–8.
Riikonen JM, Guyatt GH, Kilpeläinen TP, Craigie S, Agarwal A, Agoritsas T, et al. Decision aids for prostate cancer screening choice: a systematic review and meta-analysis. JAMA Intern Med. 2019;179(8):1072–82.
Caverly TJ, Hayward RA. Dealing with the lack of time for detailed shared decision-making in primary care: everyday shared decision-making. J Gen Intern Med. 2020:1–5.
Funding
Financial support for this study was provided in part by a grant from the National Institutes of Minority Health and Disparities (5R21CA178296, PI Allen) and by the David E. Mazzone Foundation (PI Allen). The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the interpretation of data and have drafted the work or substantively revised it. All authors have approved the submitted version. JDA: Conceived of study. Drafted the article. TP: Made substantial contribution to the data analysis, interpretation. Drafted sections of article. AK: Made substantial contribution to the data analysis, interpretation. KL: Critically revised article for important intellectual content. Approved final manuscript. KM: Made substantial contribution to the data analysis, interpretation. Drafted sections of the article. DLB: Made substantial contributions to the study concept and design. Critically revised article for important intellectual content.
Corresponding author
Ethics declarations
Ethics
All study procedures were approved by the Institutional Review Boards at Tufts University, Emory University School of Medicine, and the Atlanta VA Medical Center.
Consent for Participation/Publication
Written informed consent for publication of findings was obtained from all participants. We confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) are not identifiable and cannot be identified through the details of the manuscript.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Allen, J.D., Porteny, T., Kaplan, A. et al. Does Shared Decision-Making for Prostate Cancer Screening Among African American Men Happen? It Depends on Who You Ask. J. Racial and Ethnic Health Disparities 9, 1225–1233 (2022). https://doi.org/10.1007/s40615-021-01064-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01064-x