Abstract
Objectives
Investigate whether or not race is associated with differences in hospitalization and survival to discharge among patients with coronavirus disease-2019 (COVID-19) at the height of the pandemic in New York City (NYC).
Methods
Single-center retrospective cohort study of COVID-19 patients hospitalized at our university-affiliated NYC hospital from 3/10/20 through 4/13/20 with follow-up to 5/1/20. Our primary endpoint was hospitalization rate among patients with confirmed COVID-19 compared with the regional population based on race. Our secondary endpoint survival to discharge among hospitalized COVID-19 patients. NYC Department of Health data were used to calculate hospitalization odds ratios. Chi-square and t tests were used to compare categorial and continuous variables, respectively. Cox proportional hazards regression and predictive analysis were used to investigate our endpoints further.
Results
Our cohort of 734 patients included 355 women (48.4%), 372 Blacks (50.7%), 214 Whites (29.2%), and 92 Hispanics (12.5%) in our analysis. Blacks were nearly twice as likely as Whites to require hospitalization for COVID-19 (OR 1.89, 95% CI, 1.59–2.24, p < 0.001). Hispanics were also more likely to suffer in-hospital mortality from COVID-19 compared with Whites (HR 1.84; 95% CI 1.21–2.80; p = 0.005). There was a non-significant increased hazard of in-hospital mortality among Blacks when compared with Whites (HR, 1.30; 95% CI, 0.95–1.78; p = 0.09).
Conclusions and Relevance
Blacks were more likely than Whites to require hospitalization for COVID-19 while Hispanics were more likely to experience in-hospital mortality. Further investigation into the socioeconomic factors underlying racial disparities in COVID-19 survival and severity requiring hospitalization is needed on a national scale.
Similar content being viewed by others
Introduction
The novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic has tested the infrastructure of health systems worldwide. At the writing of this article, over 5 million people nationwide have been confirmed to be infected with coronavirus disease-2019 (COVID-19), the illness caused by SARS-CoV-2 [1]. The mortality rate for COVID-19 remains more than 10 times higher than that of influenza despite the lower prevalence rate [1,2,3]. Risk factors for intensive care unit (ICU) admission and negative outcomes with COVID-19 include obesity, hypertension, chronic lung disease, and cardiovascular disease [4,5,6]. Racial disparities in COVID-19 mortality have emerged with Black and Hispanic patients in particular having higher mortality than their White counterparts [7]. Some have ascribed the mortality trends to higher rates of hypertension and diabetes among Black patients [8] as well as to lower socioeconomic status among both populations [9, 10].
The National Medical Association has highlighted the increased exposure risk among patients from poorer backgrounds, especially Black patients, that is compounded by underlying risk factors of heart disease, diabetes, and asthma [11, 12]. New York City (NYC) was the epicenter of the COVID-19 pandemic at the time of our study and Brooklyn had more COVID-19-related deaths (4132) than any other urban locale in the United States (U.S.) through 5/12/2020. Indeed, for much of April and May 2020, New York state alone had more confirmed COVID-19 cases than any country outside the U.S. Primary data analyzing hospitalization rate by race has been limited. We aim to describe hospitalization rate by race among COVID-19 patients and to investigate how race may affect COVID-19 inpatient survival to discharge at the height of the pandemic in NYC.
Methods
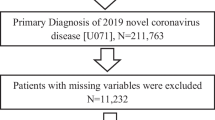
Population and Setting
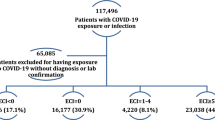
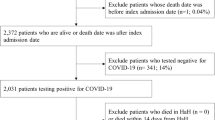
We performed a retrospective study on all adults hospitalized with COVID-19 from 3/10/2020 to 4/13/2020 with follow-up to 5/1/2020. We included all adults ≥ 18 years old who were hospitalized and tested positive on nasal swab polymerase chain reaction (PCR) for SARS-CoV-2. We excluded patients ≤ 17 years old, those still hospitalized at the time of analysis, those who tested positive for SARS-CoV-2 but who did not require hospitalization, and persons under investigation (PUI) for COVID-19 but whose nasal swab PCR was negative. This is a single-center study at a large university-affiliated teaching hospital in NYC that was approved by our Institutional Review Board (IRB #1591128-1).
Procedures and Endpoints
Data abstraction from the electronic health record was uniform for all patients. We collected demographic and clinical data including race, age, sex, length of hospitalization, initiation of COVID-19-directed medical treatments, need for intubation, and cardiac arrest requiring resuscitation. Our primary endpoint was odds of hospitalization with COVID-19 by race compared with the regional population. Our secondary endpoints included comparative and overall survival to discharge among Blacks, Hispanics, Whites, and Asians.
Statistical Analysis
We used two methods for analysis: traditional hypothesis testing and predictive analysis, a novel technique that allows direct estimation of relevant probabilities [13,14,15]. We calculated rates of hospitalization by comparing our hospitalization data with demographic data provided by the US Census Bureau and NYC Department of Health [16, 17]. We used chi-square tests to compare the survival percentages by sex, race, and underlying comorbidities. We then examined continuous variables and their relationship to survival with t tests. Univariate logistic regressions for target variables were used to construct a predictive model for probability of survival along with odds ratios (OR) for hospitalization. Cox proportional hazards regression models were used to investigate in-hospital mortality by race when adjusting for significant variables identified on univariable analysis. Regression models were reported as hazard ratios (HR) with 95% confidence intervals (CI). Kaplan-Meier plots were used to display survival analysis by race and age. A two-tailed p value < 0.05 was considered statistically significant.
To corroborate our findings, we used predictive analysis to provide direct probabilities of survival to discharge based on race and sex. The predictive forms of these models are presented in plots that depict the probability of surviving at each level of the variables of interest, specifically race and sex. Since predictive analysis gives direct probabilities, there are no confidence bounds or p values involved. Predictive analysis begins in the traditional way of building a model on an observable outcome—in this case, survival to discharge—as a function of other measures, specifically race or sex. It does not end with the analysis of parameters, as in traditional analysis, but adjusts for uncertainty in the parameters to produce direct probabilities of the outcomes for any given measure. In notational form, we produce equations like this: Pr (Survival | Sex, Data) = p. All analyses were carried out in R version 3.5.2 (R Foundation for Statistical Computing, Vienna, Austria) using the rstanarm version 2.18.2, and models fit using default priors and 10,000 iterations per chain, 4 chains per model until convergence was reached.
Results
Baseline Characteristics
During the study period of 3/10/20 through 4/13/20, a total of 865 patients were admitted to our institution with a positive SARS-CoV-2 test. Based on our exclusion criteria, our analysis ultimately included 734 patients (84.8% of all COVID-19 hospitalizations). Our cohort included 355 women (48.4%), 372 Blacks (50.7%), 214 Whites (29.2%), and 92 Hispanics (12.5%). A total of 497 patients were discharged alive (67.7%). The mean age for the cohort was 66.1 years ± 15.6 (median 68 years, range 18–99 years) and the mean body mass index (BMI) was 29.6 ± 7.9 kg/m2 (median 27.9, range 14.5–83.3). Among patients who died, the mean age was 72.7 years ± 13.9 (median 74 years) while those who survived to discharge had mean age 62.9 years ± 15.4 (median 63 years), which was statistically significant (p < 0.001). The cohort’s baseline characteristics are summarized in Table 1.
Primary and Secondary Endpoints
Based upon our hospital data, Blacks in Brooklyn were twice as likely to require hospitalization for COVID-19 compared with Whites (42.9 per 100,000 compared with 22.7 per 100,000; OR, 1.89, 95% CI 1.59–2.24, p < 0.001). This was based on US Census estimates for Brooklyn’s White and Black population in 2019 [16] and our own cohort. There was no statistically significant difference in odds for COVID-19 hospitalization between Hispanics and Whites (OR 0.84, 95% CI 0.66–1.07, p = 0.15).
Among those who died, 46% (109/237) were Black, 30% (71/237) were White, 15% (35/237) were Hispanic, and 5% (11/237) were Asian. Moreover, we found that 109/372 Blacks (29.3%), 71/214 Whites (33.2%), 35/92 Hispanics (38.0%), 11/20 Asians (55.0%), and 11/36 other ethnicities (30.6%) experienced in-hospital mortality (p = 0.1). Patients were more likely to die if they had a documented history of hypertension (35.8% vs. 25.0%, p = 0.004), chronic kidney disease (40.2% vs. 29.8%, p = 0.013), coronary artery disease (45.3% vs. 24.8%, p < 0.001), or diabetes mellitus (37.9% vs. 27.9%, p = 0.005). After adjusting for age and the aforementioned variables, Hispanics had a statistically significant increased hazard of in-hospital mortality (HR 1.84; 95% CI 1.21–2.80; p = 0.005) along with Asians (HR 2.06; 95% CI, 1.08–3.93; p = 0.03). There was a non-significant increase in hazard of in-hospital mortality among Blacks when compared with Whites (HR, 1.30; 95% CI, 0.95–1.78; p = 0.09). When compared with women, men were more likely to experience in-hospital mortality (HR, 1.50; 95% CI 1.15–1.96; p = 0.002). In-hospital mortality increased per every year increase in age (HR, 1.03; 95% CI 1.02–1.04; p = <0.001). The outcomes are summarized in Tables 2 and 3 with predictive models and Kaplan-Meier plots provided in Figs. 1, 2, and 3.
Discussion
Among hospitalized COVID-19 patients, Blacks were more likely than Whites to require hospitalization while Hispanics were more likely than Whites to suffer in-hospital mortality. To our knowledge, this is one of the most comprehensive studies analyzing race and its association with COVID-19 hospitalization and mortality based upon primary data. We had a roughly even split of male and female patients and a large number of Black patients to compare with White and Hispanic counterparts. Blacks represented 50.7% (372/734) of our COVID-19 hospitalizations and 46% (109/237) of our COVID-19-related deaths despite their comprising just 35.2% of the borough’s population [16].
Our findings are consistent with population data reported from the Center for Disease Control (CDC) with Blacks representing a disproportionate amount COVID-19-related hospitalizations and overall mortality. The NYC Department of Health has released data regarding the higher rates of COVID-19 hospitalization and death for Blacks and Hispanics in Brooklyn and NYC as a whole compared with Whites [17, 18]. Our own cohort revealed similar findings with Blacks representing half of our hospitalized and COVID-19-related mortality patients, though we found no statistically significant difference in survival to discharge between Black and White patients. This finding is similar to outcomes identified in other NYC boroughs. Golestaneh et al. found that Blacks and Hispanics with COVID-19 were more likely than Whites with COVID-19 to require hospitalization, but in-hospital mortality was equivalent across all three groups [19]. The authors also observed that both Hispanics and Blacks were more likely to test positive for SARS-CoV-2 than Whites, even when adjusting for medical comorbidities and sociodemographic factors, thereby hinting at a greater risk for SARS-CoV-2 exposure among these minority groups compared with Whites. Another possibility is that with Hispanics and Blacks more likely to be exposed to SARS-CoV-2, they may not also have equal access to medical treatment and so their overall COVID-19 mortality is underreported in both literature and health department reports.
Black patients were overrepresented among our hospitalized COVID-19 patients at the height of the pandemic in NYC. We suspect this inequality is multifactorial. Health disparities permeate medical care and researchers have noted that many marginalized ethnic minorities are considered frontline essential workers and do not have the socioeconomic backing to shelter in place [20, 21]. Researchers have revealed a threefold increased risk of positive COVID-19 testing among front-line healthcare workers in western countries [22]. The disproportionate occupational hazard among Blacks and Hispanics has been well documented [23], and the prevalence of work-related disabilities is nearly twice as high among Blacks over 50 years old when compared with their White counterparts [24]. Researchers have also identified an inverse relationship between income and COVID-19 hospitalization among the various NYC boroughs, with lower-income boroughs such as the Bronx, which has more Hispanics and Blacks compared with Whites, having higher hospitalization rates [25]. These findings suggest that socioeconomic disparities increase the risk of occupation-related disease and COVID-19 severity.
Ethnic minorities and elderly patients can be at increased risk for poor outcomes due to issues such as polypharmacy and comorbid conditions, and our own cohort demonstrated that age was significantly associated with in-hospital mortality. Blacks, Hispanics, and Native Americans nationwide suffer disproportionately from chronic illnesses compared with White patients and may be at higher risk for COVID-19 infection and severity [11, 26, 27]. In Chicago, for instance, Blacks make up 30% of the population, but 50% of COVID-19 cases and 70% of deaths [11]. Despite this, Blacks are more likely than Whites to report lack of concern for COVID-19 and less likely to report changed behavior [28], which may be due to limited alternatives in occupational risk exposure or decreased ability to engage in social isolation. Much like other researchers, we found that underlying comorbidities including hypertension, chronic kidney disease, coronary artery disease, and diabetes all increased mortality risk in COVID-19 patients [29, 30].
There are several limitations to our study, beginning with the single-center retrospective design and its susceptibility to selection bias. We concede that our cohort may not be a true representation of the nation’s population nor does our institution’s COVID-19 hospitalizations necessarily represent that of the greater NYC area. Our institution’s location can likewise lend itself to selection bias since it is located in a relatively more affluent area of Brooklyn. Moreover, critically ill patients in underserved areas may seek medical care elsewhere; therefore, our hospitalization rates may actually underestimate the true odds of hospitalization among ethnic minorities in Brooklyn. We also did not have enough information documented regarding employment status or health insurance for this cohort to include for analysis. Still, our institution’s location did not preclude us from admitting the full spectrum of patients, including those from socioeconomically disadvantaged areas. Our hospitalization rates and odds ratios are based upon 2019 US Census population records for Brooklyn, so they may not exactly reflect the borough’s population at the time of our study and they do not account for patients that do not reside in Brooklyn or who went to different hospitals. These data are the most up to date for Brooklyn’s population and our cohort, however, and they do not take away from our central message regarding healthcare inequities. Risk assessment scores such as Acute Physiology and Chronic Health Evaluation (APACHE) II were not collected due to inconsistent data reporting at the onset of the pandemic. In addition, we did not include patients hospitalized at time of analysis or patients with clinical findings strongly suggestive of COVID-19 despite having negative swab testing. Although our findings suggest that Asians have increased risk of in-hospital mortality, we recognize that the small cohort size limits reliable interpretation and generalization. The patients’ own preventive care and outpatient follow-up prior to hospitalization was likewise outside the scope of our study.
In conclusion, Blacks were more likely than Whites to require hospitalization for COVID-19 while Hispanics were more likely to experience in-hospital mortality than whites for the same illness in our NYC teaching hospital. Further investigation into the socioeconomic factors underlying racial disparities in COVID-19 infection and survival is needed on a national scale.
Data Availability
Yes
References
John Hopkins University & Medicine Coronavirus Resource Center https://Coronavirus.Jhu.Edu/Data/Racial-Data-Transparency Accessed May 2020 [database on the Internet]. Available from: https://coronavirus.jhu.edu/data. Accessed:
Ruan S. Likelihood of survival of coronavirus disease 2019. Lancet Infect Dis. 2020;20:630–1. https://doi.org/10.1016/S1473-3099(20)30257-7.
Meo SA, Al-Khlaiwi T, Usmani AM, et al. Biological and epidemiological trends in the prevalence and mortality due to outbreaks of novel coronavirus Covid-19. J King Saud Univ Sci. 2020;32:2495–9. https://doi.org/10.1016/j.jksus.2020.04.004.
Team CC-R. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–6. https://doi.org/10.15585/mmwr.mm6913e2.
Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - Covid-Net, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–64. https://doi.org/10.15585/mmwr.mm6915e3.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with Covid-19 in Wuhan, China: A Retrospective Cohort Study. Lancet. 2020;395(10229):1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3.
Laurencin CT, McClinton A. The Covid-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7(3):398–402. https://doi.org/10.1007/s40615-020-00756-0.
Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–45. https://doi.org/10.2174/1573403x11666141122220003.
Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999;896:262–77. https://doi.org/10.1111/j.1749-6632.1999.tb08121.x.
Adler NE, Boyce WT, Chesney MA, et al. Socioeconomic inequalities in health. No Easy Solution JAMA. 1993;269(24):3140–5.
Yancy CW. Covid-19 and African Americans. Jama. 2020;323:1891. https://doi.org/10.1001/jama.2020.6548.
Shah M, Sachdeva M, Dodiuk-Gad RP. Covid-19 and racial disparities. J Am Acad Dermatol. 2020;83:e35. https://doi.org/10.1016/j.jaad.2020.04.046.
Briggs W (2016) Uncertainty: the soul of modeling, probability & statistics 1st Ed. 1st ed. Springer
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–38. https://doi.org/10.1097/EDE.0b013e3181c30fb2.
Waljee AK, Higgins PD, Singal AG. A primer on predictive models. Clin Transl Gastroenterol. 2014;5:e44. https://doi.org/10.1038/ctg.2013.19.
United States Census Bureau State and County Quick Facts 2014 https://Web.Archive.Org/Web/20160217175357/. http://Quickfacts.Census.Gov/Qfd/States/36/36047.html Accessed May 2020 [database on the Internet]. Available from: http://quickfacts.census.gov/qfd/states/36/36047.html. Accessed:
Health NYCDo. Covid-19 Data: https://www1.Nyc.Gov/Site/Doh/Covid/Covid-19-Data-Boroughs.Page. 2020.
Nyc Dept of Health https://www1.Nyc.Gov/Assets/Doh/Downloads/Pdf/Imm/Covid-19-Deaths-Race-Ethnicity-04162020-1.Pdf. Accessed May 2020 [database on the Internet]. Available from: https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-race-ethnicity-04162020-1.pdf. Accessed:
Golestaneh L, Neugarten J, Fisher M, Billett HH, Gil MR, Johns T, et al. The association of race and Covid-19 mortality. EClinicalMedicine. 2020;25:100455. https://doi.org/10.1016/j.eclinm.2020.100455.
Shannon CA, Rospenda KM, Richman JA, Minich LM. Race, racial discrimination, and the risk of work-related illness, injury, or assault: findings from a national study. J Occup Environ Med. 2009;51(4):441–8. https://doi.org/10.1097/JOM.0b013e3181990c17.
Loomis D, Richardson D. Race and the risk of fatal injury at work. Am J Public Health. 1998;88(1):40–4. https://doi.org/10.2105/ajph.88.1.40.
Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of Covid-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–83. https://doi.org/10.1016/S2468-2667(20)30164-X.
Stanbury M, Rosenman KD. Occupational health disparities: a state public health-based approach. Am J Ind Med. 2014;57(5):596–604. https://doi.org/10.1002/ajim.22292.
Seabury SA, Terp S, Boden LI. Racial and ethnic differences in the frequency of workplace injuries and prevalence of work-related disability. Health Aff (Millwood). 2017;36(2):266–73. https://doi.org/10.1377/hlthaff.2016.1185.
Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, et al. Variation in Covid-19 hospitalizations and deaths across New York City boroughs. Jama. 2020;323:2192–5. https://doi.org/10.1001/jama.2020.7197.
Murphy SL, Xu J, Kochanek KD, et al. Mortality in the United States. NCHS Data Brief. 2017;2018(328):1–8.
Murphy SL, Xu J, Kochanek KD, Curtin SC, Arias E. Deaths: final data for 2015. Natl Vital Stat Rep. 2017;66(6):1–75.
Wolf MS, Serper M, Opsasnick L, et al. Awareness, attitudes, and actions related to Covid-19 among adults with chronic conditions at the onset of the U.S. outbreak: a cross-sectional survey. Ann Intern Med. 2020. https://doi.org/10.7326/M20-1239.
Leung C. Risk factors for predicting mortality in elderly patients with Covid-19: a review of clinical data in China. Mech Ageing Dev. 2020;111255:111255. https://doi.org/10.1016/j.mad.2020.111255.
Sahu KK, Mishra AK, Lal A. Comprehensive update on current outbreak of novel coronavirus infection (2019-Ncov). Ann Translat Med. 2020;8(6):393. https://doi.org/10.21037/atm.2020.02.92.
Author information
Authors and Affiliations
Contributions
Intellectual genesis—BDR, DSJ; data extraction and cleaning—BDR, NCK, KC, EB, DSJ; statistical consultation and formal data analysis—WMB, AI; data interpretation—BDR, DSJ; manuscript writing: BDR, WMB, DSJ; critical manuscript review and editing—BDR, SRM, DSJ. All authors approved the final draft as submitted.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Our study was approved by our institutional review board (IRB #1591128-1).
Consent to Participate
Not applicable; this was a retrospective cohort study.
Consent for Publication
Not applicable; this was a retrospective cohort study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Renelus, B.D., Khoury, N.C., Chandrasekaran, K. et al. Racial Disparities in COVID-19 Hospitalization and In-hospital Mortality at the Height of the New York City Pandemic. J. Racial and Ethnic Health Disparities 8, 1161–1167 (2021). https://doi.org/10.1007/s40615-020-00872-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00872-x