Abstract
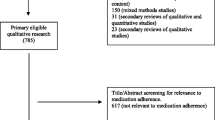
The purpose of this paper was to explore the lack of medication adherence in the African American patient community. The paper will address myths that many African American patients believe related to type 2 diabetes, hypertension treatment, and natural remedies. Research has shown that the disparities in the acceptance of healthcare provider advice and prescriptions are a significant concern particularly in African American patients. The acceptance of a provider’s diagnosis and subsequent intervention can vary based on several issues including healthcare access, patient preferences, trust of a provider, and treatment recommendations. Patient influences can range from their ability to trust the provider (and what he/she says) to following through with their advice. Several studies have looked at the beliefs and misconceptions some African Americans hold regarding the treatment of hypertension and diabetes with some showing a preference for “natural remedies.” This paper will leverage a literature review to seek out myths from African American patients to understand why they are dealing with challenges related to adherence with medication. The searches identified 58 research papers. The study applied an inductive content analysis approach to assess the research papers and identify themes. The barriers identified in this study include disbelief of the diagnosis, distrust for medication, mistrust for physicians and healthcare system, belief in alternative medicine, cultural/generation norms, and access/affordability of care. One of the most prominent factors that crossed all barriers was medical mistrust.


Similar content being viewed by others
Availability of Data and Material (Data Transparency)
Not applicable
References
Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(1_suppl):S15–27.
Copeland VC. African Americans: disparities in health care access and utilization. Health Soc Work. 2005;30(3):265–70.
Assari S. Health disparities due to diminished return among black Americans: public policy solutions. Soc Is sues Policy Rev. 2018;12(1):112–45.
Barr DA. Health disparities in the United States: social class, race, ethnicity, and the social determinants of health. Baltimore: JHU Press; 2014.
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Center for Disease Control and Prevention. U.S. Public Health Service Syphilis Study at Tuskegee. https://www.cdc.gov/tuskegee/index.html. Accessed 1 Aug 2020.
Ojanuga D. The medical ethics of the “father of gynaecology”, Dr J Marion Sims. J Med Ethics. 1993;19(1):28–31.
Washington HA. Medical apartheid: the dark history of medical experimentation on black Americans from colonial times to the present. Doubleday Books. 2006
Matthew DB. Just medicine: a cure for racial inequality in American healthcare. New York: NYU Press; 2018.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750–66.
Masharani U, Sherchan P, Schloetter M, Stratford S, Xiao A, Sebastian A, et al. Metabolic and physiologic effects from consuming a hunter-gatherer (Paleolithic)-type diet in type 2 diabetes. Eur J Clin Nutr. 2015;69(8):944–8.
US Department of Health and Human Services Office of Minority Health. Minority Health. Retrieved from https://www.minorityhealth.hhs.gov. Accessed 1 Aug 2020.
Fineberg D, Jandeleit-Dahm KA, Cooper ME. Diabetic nephropathy: diagnosis and treatment. Nat Rev Endocrinol. 2013;9(12):713–23.
Thomas SJ, Booth JN III, Dai C, Li X, Allen N, Calhoun D, et al. Cumulative incidence of hypertension by 55 years of age in blacks and whites: the CARDIA study. J Am Heart Assoc. 2018;7(14):e007988 1–10.
Guerrero-García C, Rubio-Guerra AF. Combination therapy in the treatment of hypertension. Drugs Context. 2018;7:1–9.
Cuevas AG, O'Brien K, Saha S. African American experiences in healthcare: “I always feel like I’m getting skipped over”. Health Psychol. 2016;35(9):987–95.
Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9(1):1–12.
McQuaid EL, Landier W. Cultural issues in medication adherence: disparities and directions. J Gen Intern Med. 2018;33(2):200–6.
Hatcher E, Whittemore R. Hispanic adults’ beliefs about type 2 diabetes: clinical implications. J Am Acad Nurse Pract. 2007;19(10):536–45.
Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93(1):1–9.
Shiyanbola OO, Brown CM, Ward EC. “I did not want to take that medicine”: African-Americans’ reasons for diabetes medication nonadherence and perceived solutions for enhancing adherence. Patient Preference Adherence. 2018;12:409–12.
Ndumele CD, Shaykevich S, Williams D, Hicks LS. Disparities in adherence to hypertensive care in urban ambulatory settings. J Health Care Poor Underserved. 2010;21(1):132–43.
Lewis LM, Ogedegbe C, Ogedegbe G. Enhancing adherence of antihypertensive regimens in hypertensive African Americans: current and future prospects. Expert Rev Cardiovasc Ther. 2012;10(11):1375–80.
Lukoschek P. African Americans’ beliefs and attitudes regarding hypertension and its treatment: a qualitative study. J Health Care Poor Underserved. 2003;14(4):566–87.
Dickson VV, McCarthy MM, Howe A, Schipper J, Katz SM. Sociocultural influences on heart failure self-care among an ethnic minority black population. J Cardiovasc Nurs. 2013;28(2):111–8.
Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatr. 2001;158(1):29–35.
Rucker-Whitaker C, Flynn KJ, Kravitz G, Eaton C, Calvin JE, Powell LH. Understanding African-American participation in a behavioral intervention: results from focus groups. Contemp Clin Trials. 2006;27(3):274–86.
Brown MT, Bussell J, Dutta S, Davis K, Strong S, Mathew S. Medication adherence: truth and consequences. Am J Med Sci. 2016;351(4):387–99.
World Health Organization (2020) Adherence to Long-Term Therapies. https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Accessed 1 Aug 2020.
Berelson B. Content analysis in communication research. New York: Free Press; 1952.
Krippendorff K. Content analysis: an introduction to its methodology. Thousand Oaks: Sage Publications; 2018.
Cronin P, Ryan F, Coughlan M. Undertaking a literature review: a step-by-step approach. Br J Nurs. 2008;17(1):38–43.
Jordanova L. The social construction of medical knowledge. Soc Hist Med. 1995;8(3):361–81.
Hogan VK, Rowley D, Bennett T, Taylor KD. Life course, social determinants, and health inequities: toward a national plan for achieving health equity for African American infants—a concept paper. Matern Child Health J. 2012;16(6):1143–50.
Harris MI, Klein R, Welborn TA, Knuiman MW. Onset of NIDDM occurs at least 4–7 yr before clinical diagnosis. Diabetes Care. 1992;15(7):815–9.
Rhee MK, Ho YL, Raghavan S, Vassy JL, Cho K, Gagnon D, et al. Random plasma glucose predicts the diagnosis of diabetes. PLoS One. 2019;14(7):1–13.
Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21(6):642–7.
Savoca MR, Arcury TA, Leng X, Bell RA, Chen H, Anderson A, et al. The diet quality of rural older adults in the south as measured by healthy eating index-2005 varies by ethnicity. J Am Diet Assoc. 2009;109(12):2063–7.
Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate healthcare disparities. J Gen Intern Med. 2013;28(11):1504–10.
Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–8.
Holt CL, McClure SM. Perceptions of the religion-health connection among African American church members. Qual Health Res. 2006;16(2):268–81.
Kronish IM, Leventhal H, Horowitz CR. Understanding minority patients’ beliefs about hypertension to reduce gaps in communication between patients and clinicians. The Journal of Clinical Hypertension. 2012;14(1):38–44.
Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53(4):454–61.
Schoenfeld EM, Goff SL, Downs G, Wenger RJ, Lindenauer PK, Mazor KM. A qualitative analysis of patients’ perceptions of shared decision making in the emergency department: “let me know I have a choice”. Acad Emerg Med. 2018;25(7):716–27.
Becker G, Gates RJ, Newsom E. Self-care among chronically ill African Americans: culture, health disparities, and health insurance status. Am J Public Health. 2004;94(12):2066–73.
Skirbekk H, Middelthon AL, Hjortdahl P, Finset A. Mandates of trust in the doctor–patient relationship. Qual Health Res. 2011;21(9):1182–90.
Aikens JE, Piette JD. Diabetic patients’ medication underuse, illness outcomes, and beliefs about antihyperglycemic and antihypertensive treatments. Diabetes Care. 2009;32(1):19–24.
Buckley L, Labonville S, Barr J. A systematic review of beliefs about hypertension and its treatment among African Americans. Curr Hypertens Rep. 2016;18(7):52 1–9.
Bockwoldt D, Staffileno BA, Coke L, Hamilton R, Fogg L, Calvin D, et al. Understanding experiences of diabetes medications among African Americans living with type 2 diabetes. J Transcult Nurs. 2017;28(4):363–71.
Thom DH. Physician behaviors that predict patient trust. J Fam Pract. 2001;50(4):323–4.
Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: relationship to patient requests. Fam Pract. 2002;19(5):476–83.
Cuffee YL, Hargraves JL, Rosal M, Briesacher BA, Schoenthaler A, Person S, et al. Reported racial discrimination, trust in physicians, and medication adherence among inner-city African Americans with hypertension. Am J Public Health. 2013;103(11):e55–62.
LoCurto J, Berg GM. Trust in healthcare settings: scale development, methods, and preliminary determinants. SAGE Open Med. 2016;4:2050312116664224 1–12.
McKee D, Fletcher J. Primary care for urban adolescent girls from ethnically diverse populations: foregone care and access to confidential care. J Health Care Poor Underserved. 2006;17(4):759–74.
Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97(7):1283–9.
Lorié Á, Reinero DA, Phillips M, Zhang L, Riess H. Culture and nonverbal expressions of empathy in clinical settings: a systematic review. Patient Educ Couns. 2017;100(3):411–24.
Eiser AR, Ellis G. Cultural competence and the African American experience with health care: the case for specific content in cross-cultural education. Acad Med. 2007;82(2):176–83.
Boyd EL, Taylor SD, Shimp LA, Semler CR. An assessment of home remedy use by African Americans. J Natl Med Assoc. 2000;92(7):341–53.
Gopal J, Anthonydhason V, Muthu M, Gansukh E, Jung S, Chul S, et al. Authenticating apple cider vinegar’s home remedy claims: antibacterial, antifungal, antiviral properties and cytotoxicity aspect. Nat Prod Res. 2019;33(6):906–10.
Avenues of growth in apple cider vinegar market go beyond the health & wellness trend. 2020. Retrieved from https://www.transparencymarketresearch.com/apple-cider-vinegar-market.html. Accessed 1 Aug 2020.
Tkachenko N, Chotvijit S, Gupta N, Bradley E, Gilks C, Guo W, et al. Google trends can improve surveillance of type 2 diabetes. Sci Rep. 2017;7(1):1–10.
Complementary & Alternative Medicine Market Worth $210.81 Billion By 2026. 2019. Retrieved from https://www.grandviewresearch.com/press-release/global-alternative-complementary-medicine-therapies-market. Accessed 1 Aug 2020.
Center for disease for vital signs: racial disparities in age-specific mortality among Blacks or African Americans — United States. https://www.cdc.gov/mmwr/volumes/66/wr/mm6617e1.htm. Accessed 1 Aug 2020.
Baer HA. The limited empowerment of women in black spiritual churches: an alternative vehicle to religious leadership. Sociol Relig. 1993;54(1):65–82.
Whaley AL. Cultural mistrust: an important psychological construct for diagnosis and treatment of African Americans. Prof Psychol Res Pract. 2001;32(6):555–62.
White RM. Unraveling the Tuskegee study of untreated syphilis. Arch Intern Med. 2000;160(5):585–98.
Happe LE, Clark D, Holliday E, Young T. A systematic literature review assessing the directional impact of managed care formulary restrictions on medication adherence, clinical outcomes, economic outcomes, and healthcare resource utilization. J Manag Care Pharm. 2014;20(7):677–84.
Simoens S, Sinnaeve PR. Patient co-payment and adherence to statins: a review and case studies. Cardiovasc Drugs Ther. 2014;28(1):99–109.
Munshi KD, Mager D, Ward KM, Mischel B, Henderson RR. The effect of Florida Medicaid’s state-mandated formulary provision on prescription drug use and health plan costs in a Medicaid managed care plan. J Manag Care Spec Pharm. 2018;24(2):124–31.
Kesselheim AS, Wang B, Franklin JM, Darrow JJ. Trends in utilization of FDA expedited drug development and approval programs, 1987-2014: cohort study. BMJ. 2015;351(h4633):1–7.
Zuvekas SH. Financing of behavioral health services: insurance, managed care, and reimbursement. In: Foundations of Behavioral Health. Cham: Springer; 2020. p. 71–99.
Hall G. Patient-centered clinical care for African Americans. New York: Springer; 2020.
Ngoh LN. Health literacy: a barrier to pharmacist–patient communication and medication adherence. J Am Pharm Assoc. 2009;49(5):e132–49.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30.
Müller S, Kohlmann T, Wilke T. Validation of the adherence barriers questionnaire–an instrument for identifying potential risk factors associated with medication-related non-adherence. BMC Health Serv Res. 2015;15(1):153 1–12.
Soto-Greene ML, Salas-Lopez D, Sanchez J, Like RC. Antecedents to effective treatment of hypertension in Hispanic populations. Clin Cornerstone. 2004;6(3):30–8.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Ferdinand KC, Yadav K, Nasser SA, Clayton-Jeter HD, Lewin J, Cryer DR, et al. Disparities in hypertension and cardiovascular disease in blacks: the critical role of medication adherence. J Clin Hypertens. 2017;19(10):1015–24.
Stanley SJ, Chatham AP, Trivedi N, Aldoory L. Communication and control: hearing the voices of low-income African American adults to improve relationships with healthcare providers. Health Commun. 2019:1–10.
Van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93(2):248–55.
Burgess D, Van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
To Be Used for Non-life Science Journals
Not applicable
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Code Availability (Software Application or Custom Code)
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hall, G.L., Heath, M. Poor Medication Adherence in African Americans Is a Matter of Trust. J. Racial and Ethnic Health Disparities 8, 927–942 (2021). https://doi.org/10.1007/s40615-020-00850-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00850-3