Abstract
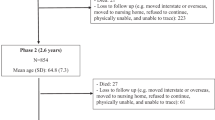
Hispanic women are at high risk for type 2 diabetes (T2D), with obesity and unhealthy eating being important contributing factors. A cross-sectional design was used in this study to identify dietary patterns and their associations with diabetes risk factors. Participants completed a culturally adapted Food Frequency Questionnaire capturing intake over the prior 3 months. Overweight/obese Hispanic women (n = 191) with or at risk for T2D were recruited from a community clinic into a weight loss intervention. Only baseline data was used for this analysis. Dietary patterns and their association with diabetes risk factors (age, body mass index, abdominal obesity, elevated fasting blood glucose [FBG], and hemoglobin A1c). An exploratory factor analysis of dietary data adjusted for energy intake was used to identify eating patterns, and Pearson correlation coefficient (r) to assess the association of the eating patterns with the diabetes risk factors. Six meaningful patterns with healthful and unhealthful traits emerged: (1) sugar and fat-laden, (2) plant foods and fish, (3) soups and starchy dishes, (4) meats and snacks, (5) beans and grains, and (6) eggs and dairy. Scores for the “sugar and fat-laden” and “meats and snacks” patterns were negatively associated with age (r = − 0.230, p = 0.001 and r = − 0.298, p < 0.001, respectively). Scores for “plant foods and fish” were positively associated with FBG (r = 0.152, p = 0.037). Being younger may be an important risk factor for a diet rich in sugar and fat; this highlights the need to assess dietary patterns among younger Hispanic women to identify traits potentially detrimental for their health.
Similar content being viewed by others
References
Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–84.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–7.
Ma Y, Hébert JR, Manson JE, Balasubramanian R, Liu S, Lamonte MJ, et al. Determinants of racial/ethnic disparities in incidence of diabetes in postmenopausal women in the US: the Women’s Health Initiative 1993–2009. Diabetes Care. 2012;35(11):2226–34.
Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. 2015.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021–9. https://doi.org/10.1001/jama.2015.10029.
Centers for Disease Control, Prevention. National diabetes statistics report, 2020. Atlanta: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020.
Ollila M-M, West S, Keinänen-Kiukaanniemi S, Jokelainen J, Auvinen J, Puukka K, et al. Overweight and obese but not normal weight women with PCOS are at increased risk of type 2 diabetes mellitus—a prospective, population-based cohort study. Hum Reprod. 2017;32(2):423–31.
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378(9785):31–40.
Rooney BL, Mathiason MA, Schauberger CW. Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern Child Health J. 2011;15(8):1166–75.
Schack-Nielsen L, Michaelsen KF, Gamborg M, Mortensen EL, Sørensen TI. Gestational weight gain in relation to offspring body mass index and obesity from infancy through adulthood. Int J Obes. 2010;34(1):67–74.
Link CL, McKinlay JB. Disparities in the prevalence of diabetes: is it race/ethnicity or socioeconomic status? Results from the Boston Area Community Health (BACH) survey. Ethn Dis. 2009;19(3):288.
Organization WH. Global health risks: mortality and burden of disease attributable to selected major risks: World Health Organization; 2009.
Dominguez K, Penman-Aguilar A, Chang M-H, Moonesinghe R, Castellanos T, Rodriguez-Lainz A, et al. Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States—2009–2013. MMWR Morb Mortal Wkly Rep. 2015;64(17):469–78.
Montonen J, Knekt P, Järvinen R, Aromaa A, Reunanen A. Whole-grain and fiber intake and the incidence of type 2 diabetes. Am J Clin Nutr. 2003;77(3):622–9.
Villegas R, Liu S, Gao Y-T, Yang G, Li H, Zheng W, et al. Prospective study of dietary carbohydrates, glycemic index, glycemic load, and incidence of type 2 diabetes mellitus in middle-aged Chinese women. Arch Intern Med. 2007;167(21):2310–6.
Malik VS, Popkin BM, Bray GA, Després J-P, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. Diabetes Care. 2010;33(11):2477–83.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9.
Smith AD, Emmett PM, Newby P, Northstone K. Dietary patterns obtained through principal components analysis: the effect of input variable quantification. Br J Nutr. 2013;109(10):1881–91.
Dietary Guidelines Advisory Committee. 2015–2020 dietary guidelines for Americans. Washington (DC): USDA. 2015.
Santiago-Torres M, Kratz M, Lampe JW, Tapsoba JDD, Breymeyer KL, Levy L, et al. Metabolic responses to a traditional Mexican diet compared with a commonly consumed US diet in women of Mexican descent: a randomized crossover feeding trial, 2. Am J Clin Nutr. 2015;103(2):366–74.
Sofianou A, Fung TT, Tucker KL. Differences in diet pattern adherence by nativity and duration of US residence in the Mexican-American population. J Am Diet Assoc. 2011;111(10):1563–9. e2.
Carrera PM, Gao X, Tucker KL. A study of dietary patterns in the Mexican-American population and their association with obesity. J Am Diet Assoc. 2007;107(10):1735–42.
Norman S, Castro C, Albright C, King A. Comparing acculturation models in evaluating dietary habits among low-income Hispanic women. Ethn Dis. 2004;14(3):399–404.
Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and non-Hispanic whites. J Nutr. 2011;141(10):1898–906.
Davis NJ, Schechter CB, Ortega F, Rosen R, Wylie-Rosett J, Walker EA. Dietary patterns in blacks and Hispanics with diagnosed diabetes in New York City’s South Bronx. Am J Clin Nutr. 2013;97(4):878–85.
Reininger B, Lee M, Jennings R, Evans A, Vidoni M. Healthy eating patterns associated with acculturation, sex and BMI among Mexican Americans. Public Health Nutr. 2017;20(7):1267–78.
Montez JK, Eschbach K. Country of birth and language are uniquely associated with intakes of fat, fiber, and fruits and vegetables among Mexican-American women in the United States. J Am Diet Assoc. 2008;108(3):473–80.
Pachucki MA. Food pattern analysis over time: unhealthful eating trajectories predict obesity. Int J Obes. 2012;36(5):686–94.
Association AD. Standards of medical care in diabetes—2017 abridged for primary care providers. Clin Diabetes. 2017;35(1):5–26.
Taren D, De Tobar M, Ritenbaugh C, Graver E, Whitacre R, Aickin M. Evaluation of the southwest food frequency questionnaire. ECOL FOOD NUTR. 2000;38(6):515–47.
Ritenbaugh C, Aickin M, Taren D, Teufel N, Graver E, Woolf K, et al. Use of a food frequency questionnaire to screen for dietary eligibility in a randomized cancer prevention phase III trial. Cancer Epidemiol Biomarkers Prev. 1997;6(5):347–54.
Hepburn FN. The USDA National Nutrient Data Bank. Am J Clin Nutr. 1982;35(5):1297–301.
Flood A, Rastogi T, Wirfält E, Mitrou PN, Reedy J, Subar AF, et al. Dietary patterns as identified by factor analysis and colorectal cancer among middle-aged Americans. Am J Clin Nutr. 2008;88(1):176–84.
Judd SE, Letter AJ, Shikany JM, Roth DL, Newby P. Dietary patterns derived using exploratory and confirmatory factor analysis are stable and generalizable across race, region, and gender subgroups in the REGARDS study. Front Nutr. 2015;1:29.
Tabachnick BG, Fidell LS. Using multivariate statistics. Boston: Pearson Education. Inc.; 2007.
Bryant FB, Yarnold PR. Principal-components analysis and exploratory and confirmatory factor analysis. 1995.
Hatcher L. A step-by-step approach to using the SAS system for factor analysis and structural equation modeling. Cary: SAS Institute; 2005.
Alhazmi A, Stojanovski E, McEvoy M, Garg ML. The association between dietary patterns and type 2 diabetes: a systematic review and meta-analysis of cohort studies. J Hum Nutr Diet. 2014;27(3):251–60. https://doi.org/10.1111/jhn.12139.
McEvoy CT, Cardwell CR, Woodside JV, Young IS, Hunter SJ, McKinley MC. A posteriori dietary patterns are related to risk of type 2 diabetes: findings from a systematic review and meta-analysis. J Acad Nutr Diet. 2014;114(11):1759–75. e4.
Denova-Gutiérrez E, Castañón S, Talavera JO, Gallegos-Carrillo K, Flores M, Dosamantes-Carrasco D, et al. Dietary patterns are associated with metabolic syndrome in an urban Mexican population. J Nutr. 2010;140(10):1855–63.
Bach-Faig A, Berry EM, Lairon D, Reguant J, Trichopoulou A, Dernini S, et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011;14(12A):2274–84. https://doi.org/10.1017/S1368980011002515.
Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8):1093–100.
Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Donati MB, et al. Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. Eur J Prev Cardiol. 2016;23(4):400–7. https://doi.org/10.1177/2047487315569409.
Gong Y, Tian G, Xue H, Zhang X, Zhao Y, Cheng G. Higher adherence to the ‘vegetable-rich’ dietary pattern is related to longer telomere length in women. Clin Nutr. 2017.
Noel SE, Newby P, Ordovas JM, Tucker KL. Adherence to an (n-3) fatty acid/fish intake pattern is inversely associated with metabolic syndrome among Puerto Rican adults in the greater Boston Area–3. J Nutr. 2010;140(10):1846–54.
Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Dietary patterns and markers of systemic inflammation among Iranian women. J Nutr. 2007;137(4):992–8.
Brunner EJ, Mosdøl A, Witte DR, Martikainen P, Stafford M, Shipley MJ, et al. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87(5):1414–21.
Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000;72(4):912–21.
Murtaugh MA, Herrick JS, Sweeney C, Baumgartner KB, Guiliano AR, Byers T, et al. Diet composition and risk of overweight and obesity in women living in the southwestern United States. J Am Diet Assoc. 2007;107(8):1311–21.
Flores M, Macias N, Rivera M, Lozada A, Barquera S, Rivera-Dommarco J, et al. Dietary patterns in Mexican adults are associated with risk of being overweight or obese–3. J Nutr. 2010;140(10):1869–73.
Stern D, Piernas C, Barquera S, Rivera JA, Popkin BM. Caloric beverages were major sources of energy among children and adults in Mexico, 1999–2012. J Nutr. 2014;144(6):949–56. https://doi.org/10.3945/jn.114.190652.
Mattei J, Noel SE, Tucker KL. A meat, processed meat, and French fries dietary pattern is associated with high allostatic load in Puerto Rican older adults. J Am Diet Assoc. 2011;111(10):1498–506.
Siega-Riz AM, Sotres-Alvarez D, Ayala GX, Ginsberg M, Himes JH, Liu K, et al. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am J Clin Nutr. 2014;99(6):1487–98.
Montoya JA, Salinas JJ, Barroso CS, Mitchell-Bennett L, Reininger B. Nativity and nutritional behaviors in the Mexican origin population living in the US-Mexico border region. J IMMIGR MINOR HEALT. 2011;13(1):94–100.
Fitzgerald N, Damio G, Segura-Pérez S, Pérez-Escamilla R. Nutrition knowledge, food label use, and food intake patterns among Latinas with and without type 2 diabetes. J Am Diet Assoc. 2008;108(6):960–7.
Valdez L, Amezquita A, Hooker S, Garcia D. Mexican-origin male perspectives of diet-related behaviors associated with weight management. Int J Obes. 2017;41(12):1824–30.
Maskarinec G, Novotny R, Tasaki K. Dietary patterns are associated with body mass index in multiethnic women. J Nutr. 2000;130(12):3068–72.
Koopman KE, Caan MW, Nederveen AJ, Pels A, Ackermans MT, Fliers E, et al. Hypercaloric diets with increased meal frequency, but not meal size, increase intrahepatic triglycerides: a randomized controlled trial. Hepatology. 2014;60(2):545–53.
Tucker KL. Dietary patterns, approaches, and multicultural perspective. Appl Physiol Nutr Metab. 2010;35(2):211–8.
Funding
This work was supported by the National Institutes of Health and the National Institute of Diabetes and Digestive Kidney Diseases, grant 1R01DK099277.
Author information
Authors and Affiliations
Contributions
MAG, ML, MB, CW, CDA, SH, and SVL conceptualized the study; NL, SG, AT, KV, ES, VS, and SVL were involved in study administration and data collection; MAG, ML, MB, CW, CDA, SH, and SVL analyzed and interpreted the data; MAG and SVL wrote the manuscript. All authors reviewed, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
All interested women with confirmed eligibility provided written informed consent prior to data collection. All study materials and procedures were approved by the Kaiser Permanente Center for Health Research, Virginia Garcia Memorial Health Center, and Arizona State University Institutional Review Boards.
Conflict of Interest
The authors declare that they have no conflict of interest.
Disclaimer
The National Institutes of Health and the National Institute of Diabetes and Digestive Kidney Diseases had no role in the design, analysis or writing of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arias-Gastélum, M., Lindberg, N.M., Leo, M.C. et al. Dietary Patterns with Healthy and Unhealthy Traits Among Overweight/Obese Hispanic Women with or at High Risk for Type 2 Diabetes. J. Racial and Ethnic Health Disparities 8, 293–303 (2021). https://doi.org/10.1007/s40615-020-00782-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00782-y