Abstract
Background
Differentiating whether disparities in outcomes for sepsis among racial groups are due to differences in hospital care versus pre-hospitalization factors is an important step in developing effective strategies to reduce these disparities. As such, we examined the association between race and case fatality rates among hospitalizations for sepsis.
Methods
This was a case-control study of hospitalizations for sepsis in all acute-care, non-federal California hospitals during 2011. The association between hospital mortality and race was examined using hierarchical logistic regression analysis.
Results
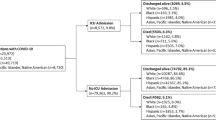
Among 131,831 hospitalizations for sepsis, the unadjusted case fatality rates were 15.1 % in whites, 14.0 % in blacks, 13.8 % in Hispanics, and 16.2 % in Asians (P < 0.001). Compared to whites, the odds of hospital mortality was 0.84 (95 % CI 0.79–0.89) for blacks, 0.88 (95 % CI 0.84–0.92) for Hispanics, and 0.93 (95 % CI 0.87–0.98) for Asians after controlling for patient, healthcare systems, and hospital-level factors. There was no difference in the variability of sepsis mortality across hospitals between racial groups. The range of case fatality rates for sepsis among hospitals was 8.3–22.9 % for whites, 9.1–20.5 % for blacks, 7.0–19.1 % for Hispanics, and 10.0–23.0 % for Asians.
Conclusion
Case fatality rates for sepsis hospitalizations are lower in minority racial groups in California. Future studies and interventions that seek to reduce racial disparities in sepsis need to focus on pre-hospitalization factors that contribute to population-level racial differences in sepsis outcomes.

Similar content being viewed by others
References
Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21(6):667–9. doi:10.1111/j.1525-1497.2006.0512.x.
Stith AY. NAIoMCoUaERaEDiHC, Board on Health Policy, Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: National Academcy Press; 2002.
Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177(3):279–84. doi:10.1164/rccm.200703-480OC.
Esper AM, Moss M, Lewis CA, Nisbet R, Mannino DM, Martin GS. The role of infection and comorbidity: factors that influence disparities in sepsis. Crit Care Med. 2006;34(10):2576–82. doi:10.1097/01.ccm.0000239114.50519.0e.
Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–54. doi:10.1056/NEJMoa022139.
Mayr FB, Yende S, Linde-Zwirble WT, Peck-Palmer OM, Barnato AE, Weissfeld LA, et al. Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA J Am Med Assoc. 2010;303(24):2495–503. doi:10.1001/jama.2010.851.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–10.
Mayr FB, Yende S, D’Angelo G, Barnato AE, Kellum JA, Weissfeld L, et al. Do hospitals provide lower quality of care to Black patients for pneumonia? Crit Care Med. 2010;38(3):759–65. doi:10.1097/CCM.0b013e3181c8fd58.
Epstein AM, Ayanian JZ. Racial disparities in medical care. N Engl J Med. 2001;344(19):1471–3. doi:10.1056/NEJM200105103441911.
Barnato AE, Berhane Z, Weissfeld LA, Chang CC, Linde-Zwirble WT, Angus DC. Racial variation in end-of-life intensive care use: a race or hospital effect? Health Serv Res. 2006;41(6):2219–37. doi:10.1111/j.1475-6773.2006.00598.x.
Banta JE, Joshi KP, Beeson L, Nguyen HB. Patient and hospital characteristics associated with inpatient severe sepsis mortality in California, 2005–2010. Crit Care Med. 2012;40(11):2960–6. doi:10.1097/CCM.0b013e31825bc92f.
Healthcare Cost and Utilization Project (HCUP) databases, 2014. Agency for healthcare research and quality, Rockville, MD http://hcup-usahrqgov/databasesjsp Accessed Jun 16, 2015.
Office of Statewide Health Planning and Development. Hospital Data/Financial. www.oshpd.ca.gov/HID/Dataflow/HospMain.html.. June 16, 2015.
Chang DW, Huynh R, Sandoval E, Han N, Coil CJ, Spellberg BJ. Volume of fluids administered during resuscitation for severe sepsis and septic shock and the development of the acute respiratory distress syndrome. J Crit Care. 2014;29(6):1011–5. doi:10.1016/j.jcrc.2014.06.005.
Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2012. doi:10.1097/MLR.0b013e318268ac86.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637. doi:10.1097/CCM.0b013e31827e83af.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31(4):1250–6. doi:10.1097/01.CCM.0000050454.01978.3B.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49(12):1429–33.
Morris CN. Parametric empirical bayes inference: theory and applications. J Am Stat Assoc. 1983;78(381):47–55. doi:10.2307/2287098.
Normand S-LT, Glickman ME, Gatsonis CA. Statistical methods for profiling providers of medical care: issues and applications. J Am Stat Assoc. 1997;92(439):803–14. doi:10.2307/2965545.
Seymour CW, Iwashyna TJ, Ehlenbach WJ, Wunsch H, Cooke CR. Hospital-level variation in the use of intensive care. Health Serv Res. 2012;47(5):2060–80. doi:10.1111/j.1475-6773.2012.01402.x.
Prescott HC, Kepreos KM, Wiitala WL, Iwashyna TJ. Temporal changes in the influence of hospitals and regional healthcare networks on severe sepsis mortality. Crit Care Med. 2015. doi:10.1097/ccm.0000000000000970.
Acknowledgments
Contributions
Drs. Sandoval and Chang are the guarantors of the contents in the manuscript including the data and analysis.
Dr. Sandoval contributed to analyzing and interpreting the data and drafted the submitted article.
Dr. Chang contributed to acquiring, analyzing, and interpreting the data; reviewed and revised the article critically for important intellectual content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Eric Sandoval has no conflicts of interest to report. Dr. Dong Chang has no conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Sandoval, E., Chang, D.W. Association Between Race and Case Fatality Rate in Hospitalizations for Sepsis. J. Racial and Ethnic Health Disparities 3, 625–634 (2016). https://doi.org/10.1007/s40615-015-0181-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-015-0181-0