Abstract
Objective
Quality improvement (QI) tools can identify and address health disparities. This paper describes the use of resident prescriber profiles in a novel QI curriculum to identify racial and ethnic differences in antidepressant and antipsychotic prescribing.
Methods
The authors extracted medication orders written by 111 psychiatry residents over an 18-month period from an electronic medical record and reformatted these into 6133 unique patient encounters. Binomial logistic models adjusted for covariates assessed racial and ethnic differences in antipsychotic or antidepressant prescribing in both emergency and inpatient psychiatric encounters. A multinomial model adjusted for covariates then assessed racial and ethnic differences in primary diagnosis. Models also examined interactions between gender and race/ethnicity.
Results
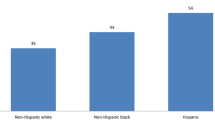
Black (adjusted OR 0.66; 95% CI, 0.50–0.87; p < 0.01) and Latinx (adjusted OR, 0.65; 95% CI, 0.49–0.86; p < 0.01) patients had lower odds of receiving antidepressants relative to White patients despite diagnosis. Black and Latinx patients were no more likely to receive antipsychotics than White patients when adjusted for diagnosis. Black (adjusted OR 3.85; 95% CI, 2.9–5.2) and Latinx (adjusted OR 1.60; 95% CI, 1.1–2.3) patients were more likely to receive a psychosis than a depression diagnosis when compared to White patients. Gender interactions with race/ethnicity did not significantly change results.
Conclusions
Our findings suggest that racial/ethnic differences in antidepressant prescription likely result from alternatively higher diagnosis of psychotic disorders and prescription of antipsychotics in Black and Latinx patients. Prescriber profiles can serve as a powerful tool to promote resident QI learning around the effects of structural racism on clinical care.


Similar content being viewed by others
References
Agency for Healthcare Research and Quality. Module 4. Approaches to quality improvement [Internet]. 2013 [cited 2020 Sep 27]. Available from: http://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html
Wagner R, Koh N, Bagian J, Weiss K, For the CLER program. Issue brief #4: health care disparities [internet]. Chicago, Illinois, USA: Accreditation Council for Graduate Medical Education; 2016. Available from: https://www.acgme.org/Portals/0/PDFs/CLER/CLER_Health_Care_Disparities_Issue_Brief.pdf. Accessed 16 Sept 2020
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century [Internet]. Washington (DC): National Academies Press (US); 2001 [cited 2020 Sep 16]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK222274/
Sivashanker K, Gandhi TK. Advancing safety and equity together. N Engl J Med Massachusetts Medical Society. 2020;382:301–3.
Wells K, Sherbourne C, Schoenbaum M, Ettner S, Duan N, Miranda J, et al. Five-year impact of quality improvement for depression: results of a group-level randomized controlled trial. Arch Gen Psychiatry. 2004;61:378–86.
Li L, Gupta N, Wasser T. A novel initiative contextualizing quality improvement and systems based practice in psychiatric clinical teaching settings. J Ment Health Train Educ Pract. 2019;14:156–63.
Rohrbaugh R, Federman DG, Borysiuk L, Sernyak M. Utilizing VA information technology to develop psychiatric resident prescription profiles. Acad Psychiatry. 2009;33:27–30.
Cook TB, Reeves GM, Teufel J, Postolache TT. Persistence of racial disparities in prescription of first-generation antipsychotics in the USA. Pharmacoepidemiol Drug Saf. 2015;24:1197–206.
Lisotto MJ. Mental health disparities: Hispanics and Latinos [Internet]. American Psychiatric Association; 2017. https://www.Mental-Health-Facts-for-Hispanic-Latino.pdf. Accessed 17 Sept 2020
Simpson SM, Krishnan LL, Kunik ME, Ruiz P. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatry Q. 2007;78:3–14.
EPIC. Verona, WI; 2020.
Tableau. Seattle, WA; 2019.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria; 2013.
McGregor B, Li C, Baltrus P, Douglas M, Hopkins J, Wrenn G, et al. Racial and ethnic disparities in treatment and treatment type for depression in a national sample of Medicaid recipients. Psychiatr Serv. 2020;71:663–9.
Olbert CM, Nagendra A, Buck B. Meta-analysis of black vs. white racial disparity in schizophrenia diagnosis in the United States: do structured assessments attenuate racial disparities? J Abnorm Psychol. 2018;127:104–15.
Minsky S, Vega W, Miskimen T, Gara M, Escobar J. Diagnostic patterns in Latino, African American, and European American psychiatric patients. Arch Gen Psychiatry. 2003;60:637–44.
Sonik RA, Creedon TB, Progovac AM, Carson N, Delman J, Delman D, et al. Depression treatment preferences by race/ethnicity and gender and associations between past healthcare discrimination experiences and present preferences in a nationally representative sample. Soc Sci Med. 2020;253:112939.
Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41:479–89.
Balsa AI, McGuire TG. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. J Health Econ. 2003;22:89–116.
Jimenez DE, Bartels SJ, Cardenas V, Dhaliwal SS, Alegría M. Cultural beliefs and mental health treatment preferences of ethnically diverse older adult consumers in primary care. Am J Geriatr Psychiatry. 2012;20:533–42.
Vale MD, Good M-JD. Transcending the profession: psychiatric patients’ experiences of trust in clinicians. J Health Soc Behav. 2020;61:208–22.
Lewis-Fernández R, Aggarwal NK, Ladson Hinton, Devon E. Hinton, Laurence J. Kirmayer. DSM-5® Handbook on the cultural formulation interview [Internet]. Washington, DC: American Psychiatric Publishing; 2016 [cited 2020 Sep 28]. Available from: https://www.appi.org/dsm-5_handbook_on_the_cultural_formulation_interview
Silva MA, Paris M, Añez LM. CAMINO: integrating context in the mental health assessment of immigrant Latinos. Prof Psychol Res Pract American Psychological Association. 2017;48:453–60.
Bourgois P, Holmes SM, Sue K, Quesada J. Structural vulnerability: operationalizing the concept to address health disparities in clinical care. Acad Med. 2017;92:299–307.
Scheper-Hughes N. Embodied knowledge: thinking with the body in critical medical anthropology. In: Borofsky R, editor. Assessing cultural anthropology. New York: McGraw-Hill, Inc.; 1994.
Metzl JM. Protest psychosis: how schizophrenia became a black disease. Boston: Beacon Press; 2010.
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–63.
Crear-Perry J, Maybank A, Keeys M, Mitchell N, Godbolt D. Moving towards anti-racist praxis in medicine. Lancet Elsevier. 2020;396:451–3.
Ross PT, Lypson ML, Byington CL, Sánchez JP, Wong BM, Kumagai AK. Learning from the past and working in the present to create an antiracist future for academic medicine. Acad Med. 2020;95:1781–6.
Cerdeña JP, Plaisime MV, Tsai J. From race-based to race-conscious medicine: how anti-racist uprisings call us to act. Lancet. Elsevier. 2020;396:1125–8.
Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–33.
Cook BL, McGuire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care: methods and practical issues. Health Serv Res. 2012;47:1232–54.
Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez MH, Jewell ST, Matsoukas K, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5:117–40.
Lam PW, Wong BM. Harnessing the power of residents as change agents in quality improvement. Academic Medicine [Internet]. 2020 [cited 2020 Sep 28];Publish Ahead of Print. Available from: https://journals.lww.com/academicmedicine/Abstract/9000/Harnessing_the_Power_of_Residents_as_Change_Agents.96993.aspx?utm_source=sfmc&utm_medium=email&utm_campaign=amexpress&utm_content=newsletter%0d
Funding
Dr. Wasser’s salary is funded in part by the State of Connecticut, Department of Mental Health and Addiction Services, but this publication does not express the views of the Department of Mental Health and Addiction Services or the State of Connecticut. Ms. Cerdeña is supported by the Robert Wood Johnson Foundation Health Policy Research Scholars program and the National Institutes of Health Medical Scientist Training Program (T32 T32GM136651). The views and opinions expressed are those of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Rohrbaugh is an Academic Psychiatry editorial board member. Manuscripts that are authored by a member of the Editorial Board undergo the same editorial review process applied to all manuscripts, including double-blinded peer review. On behalf of the remaining authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cerdeña, I., Holloway, T., Cerdeña, J.P. et al. Racial and Ethnic Differences in Psychiatry Resident Prescribing: a Quality Improvement Education Intervention to Address Health Equity. Acad Psychiatry 45, 13–22 (2021). https://doi.org/10.1007/s40596-021-01397-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40596-021-01397-z