Abstract
Purpose
Climate change threatens progress achieved in global reductions of infectious disease rates over recent decades. This review summarizes literature on potential impacts of climate change on waterborne diseases, organized around a framework of questions that can be addressed depending on available data.
Recent Findings
A growing body of evidence suggests that climate change may alter the incidence of waterborne diseases, and diarrheal diseases in particular. Much of the existing work examines historical relationships between weather and diarrhea incidence, with a limited number of studies projecting future disease rates. Some studies take social and ecological factors into account in considerations of historical relationships, but few have done so in projecting future conditions.
Summary
The field is at a point of transition, toward incorporating social and ecological factors into understanding the relationships between climatic factors and diarrheal diseases and using this information for future projections. The integration of these components helps identify vulnerable populations and prioritize adaptation strategies.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Watts N, Adger WN, Ayeb-Karlsson S, Bai Y, Byass P, Campbell-Lendrum D, et al. The Lancet Countdown: tracking progress on health and climate change. Lancet. 2017;389:1151–64. https://doi.org/10.1016/S0140-6736(16)32124-9.
IPCC. Climate Change. In: Stocker TF, Qin D, Plattner G-K, Tignor M, Allen SK, Boschung J, et al., editors. The physical science basis. Contribution of working group I to the fifth assessment report of the intergovernmental panel on climate change. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2013. 2013. p. 1535 pp.
•• Levy K, Woster AP, Goldstein RS, Carlton EJ. Untangling the impacts of climate change on waterborne diseases: a systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ Sci Technol. 2016;50:4905–22. https://doi.org/10.1021/acs.est.5b06186. This is a systematic review of the epidemiological literature that describes key areas of agreement and evaluates the biological plausibility of these associations.
Smith KR, Woodward A, Campbell-Lendrum D, Chadee DD, Honda Y, Liu Q, et al. Human health: impacts, adaptation, and co-benefits. In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al., editors. Climate change 2014: impacts, adaptation, and vulnerability. Part a: global and sectoral aspects. Contribution of working group II to the fifth assessment report of the intergovernmental panel on climate change. Cambridge, United Kingdom. New York: Cambridge University Press; 2014. p. 709–54.
GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the global burden of disease study 2015. Lancet Infect Dis. 2017;17:909–48. https://doi.org/10.1016/S1473-3099(17)30276-1.
Troeger C, Colombara DV, Rao PC, Khalil IA, Brown A, Brewer TG, et al. Global disability-adjusted life-year estimates of long-term health burden and undernutrition attributable to diarrhoeal diseases in children younger than 5 years. Lancet Global Health. 2018;6:e255–e69. https://doi.org/10.1016/s2214-109x(18)30045-7.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61. https://doi.org/10.1016/S0140-6736(12)60560-1.
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2197–223. https://doi.org/10.1016/S0140-6736(12)61689-4.
Schaible UE,Kaufmann SH. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4:e115. https://doi.org/10.1371/journal.pmed.0040115.
Bartram J,Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med. 2010;7:e1000367. https://doi.org/10.1371/journal.pmed.1000367.
Sachs J. The end of poverty. New York: Penguin Press; 2005.
Campbell-Lendrum D, Woodruff R. Comparative risk assessment of the burden of disease from climate change. Environ Health Perspect. 2006;114:1935–41. https://doi.org/10.1289/ehp.8432.
McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859–69. https://doi.org/10.1016/s0140-6736(06)68079-3.
Curriero FC, Patz JA, Rose JB, Lele S. The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948–1994. Am J Public Health. 2001;91:1194–9.
Effler E, Isaacson M, Arntzen L, Heenan R, Canter P, Barrett T, et al. Factors contributing to the emergence of Escherichia coli O157 in Africa. Emerg Infect Dis. 2001;7:812–9. https://doi.org/10.3201/eid0705.017507.
Shiffman MA, Schneider R, Turner AG, Helms RW. Seasonality in water related intestinal disease in Guatemala. Int J Biometeorol. 1976;20:223–9.
Thomas MK, Charron DF, Waltner-Toews D, Schuster C, Maarouf AR, Holt JDA. Role of high impact weather events in waterborne disease outbreaks in Canada, 1975-2001. Int J Environ Health Res. 2006;16:167–80. https://doi.org/10.1080/09603120600641326.
Checkley W, Epstein LD, Gilman RH, Figueroa D, Cama RI, Patz JA, et al. Effects of El Nino and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355:442–50.
Kolstad EW, Johansson KA. Uncertainties associated with quantifying climate change impacts on human health: a case study for diarrhea. Environ Health Perspect. 2011;119:299–305. https://doi.org/10.1289/ehp.1002060.
•• Carlton EJ, Woster AP, DeWitt P, Goldstein RS, Levy KA. Systematic review and meta-analysis of ambient temperature and diarrhoeal diseases. Int J Epidemiol. 2016;45:117–30. https://doi.org/10.1093/ije/dyv296. This meta-analysis found evidence for a positive association between ambient temperature and all cause-diarrheal and bacterial diarrhea, but not viral diarrheal, highlighting heterogeneity in associations between temperature and diarrheal disease by pathogen.
• Philipsborn R, Ahmed SM, Brosi BJ, Levy K. Climatic drivers of Diarrheagenic Escherichia coli incidence: a systematic review and meta-analysis. J Infect Dis. 2016;214:6–15. https://doi.org/10.1093/infdis/jiw081. This meta-analysis found evidence to suggest cases of ETEC-associated diarrhea will increase under future climate scenarios and provides a model of data-driven pathogen and region-specific climate health projections.
Climate-and-health debate warms up. Lancet 1996;347:1567.
Bouma MJ, Sondorp HE, Health v d KHJ. climate change. Lancet. 1994;343:302–4.
Colwell R, Epstein P, Gubler D, Hall M, Reiter P, Shukla J, et al. Global climate change and infectious diseases. Emerg Infect Dis. 1998;4:451–2. https://doi.org/10.3201/eid0403.980327.
Cook GC. Effect of global warming on the distribution of parasitic and other infectious diseases: a review. J R Soc Med. 1992;85:688–91.
Epstein PR. Global warming and vector-borne disease. Lancet. 1998;351:1737; author reply 8. https://doi.org/10.1016/s0140-6736(05)77777-1.
Githeko AK, Lindsay SW, Confalonieri UE, Patz JA. Climate change and vector-borne diseases: a regional analysis. Bull World Health Organ. 2000;78:1136–47.
Gubler DJ. Resurgent vector-borne diseases as a global health problem. Emerg Infect Dis. 1998;4:442–50. https://doi.org/10.3201/eid0403.980326.
Haines A. Global warming and vector-borne disease. Lancet. 1998;351:1737–8. https://doi.org/10.1016/s0140-6736(05)77778-3.
Reiter P. Global warming and mosquito-borne disease in USA. Lancet. 1996;348:622. https://doi.org/10.1016/s0140-6736(05)64844-1.
Reiter P. Global-warming and vector-borne disease in temperate regions and at high altitude. Lancet. 1998;351:839–40. https://doi.org/10.1016/s0140-6736(05)78979-0.
Sutherst RW, Ingram JS, Scherm H. Global change and vector-borne diseases. Parasitol Today (Personal ed). 1998;14:297–9.
Astrom C, Rocklov J, Hales S, Beguin A, Louis V, Sauerborn R. Potential distribution of dengue fever under scenarios of climate change and economic development. EcoHealth. 2012;9:448–54. https://doi.org/10.1007/s10393-012-0808-0.
Bardosh KL, Ryan S, Ebi K, Welburn S, Singer B. Addressing vulnerability, building resilience: community-based adaptation to vector-borne diseases in the context of global change. Infect Dis Poverty. 2017;6:166. https://doi.org/10.1186/s40249-017-0375-2.
Purse BV, Masante D, Golding N, Pigott D, Day JC, Ibanez-Bernal S, et al. How will climate change pathways and mitigation options alter incidence of vector-borne diseases? A framework for leishmaniasis in south and Meso-America. PLoS One. 2017;12:e0183583. https://doi.org/10.1371/journal.pone.0183583.
Ramirez B. Support for research towards understanding the population health vulnerabilities to vector-borne diseases: increasing resilience under climate change conditions in Africa. Infect Dis Poverty. 2017;6:164. https://doi.org/10.1186/s40249-017-0378-z.
Smith DL, Perkins TA, Reiner RC Jr, Barker CM, Niu T, Chaves LF, et al. Recasting the theory of mosquito-borne pathogen transmission dynamics and control. Trans R Soc Trop Med Hyg. 2014;108:185–97. https://doi.org/10.1093/trstmh/tru026.
Sumilo D, Bormane A, Asokliene L, Vasilenko V, Golovljova I, Avsic-Zupanc T, et al. Socio-economic factors in the differential upsurge of tick-borne encephalitis in central and Eastern Europe. Rev Med Virol. 2008;18:81–95. https://doi.org/10.1002/rmv.566.
Brisbois BW, Ali SH. Climate change, vector-borne disease and interdisciplinary research: social science perspectives on an environment and health controversy. EcoHealth. 2010;7:425–38. https://doi.org/10.1007/s10393-010-0354-6.
Medlock JM, Leach SA. Effect of climate change on vector-borne disease risk in the UK. Lancet Infect Dis. 2015;15:721–30. https://doi.org/10.1016/s1473-3099(15)70091-5.
Parham PE, Waldock J, Christophides GK, Hemming D, Agusto F, Evans KJ, et al. Climate, environmental and socio-economic change: weighing up the balance in vector-borne disease transmission. Philos Trans R Soc Lond Ser B Biol Sci. 2015;370:20130551. https://doi.org/10.1098/rstb.2013.0551.
Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe. 2011;17:337–40. https://doi.org/10.1016/j.anaerobe.2011.05.016.
Tabachnick WJ. Challenges in predicting climate and environmental effects on vector-borne disease episystems in a changing world. J Exp Biol. 2010;213:946–54. https://doi.org/10.1242/jeb.037564.
Waldock J, Chandra NL, Lelieveld J, Proestos Y, Michael E, Christophides G, et al. The role of environmental variables on Aedes albopictus biology and chikungunya epidemiology. Pathogens Glob Health. 2013;107:224–41. https://doi.org/10.1179/2047773213y.0000000100.
Bambrick HJ, Capon AG, Barnett GB, Beaty RM, Burton AJ. Climate change and health in the urban environment: adaptation opportunities in Australian cities. Asia Pac J Public Health. 2011;23:67S–9. https://doi.org/10.1177/1010539510391774.
Sutherst RW. Global change and human vulnerability to vector-borne diseases. Clin Microbiol Rev. 2004;17:136–73.
Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect. 2014;122:1209–15. https://doi.org/10.1289/ehp.1306796.
Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117:61–7. https://doi.org/10.1289/ehp.11594.
Reid CE, Mann JK, Alfasso R, English PB, King GC, Lincoln RA, et al. Evaluation of a heat vulnerability index on abnormally hot days: an environmental public health tracking study. Environ Health Perspect. 2012;120:715–20. https://doi.org/10.1289/ehp.1103766.
Cann KF, Thomas DR, Salmon RL, Wyn-Jones AP, Kay D. Extreme water-related weather events and waterborne disease. Epidemiol Infect. 2013;141:671–86. https://doi.org/10.1017/S0950268812001653.
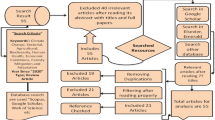
•• Lo Iacono G, Armstrong B, Fleming LE, Elson R, Kovats S, Vardoulakis S, et al. Challenges in developing methods for quantifying the effects of weather and climate on water-associated diseases: a systematic review. PLoS Negl Trop Dis. 2017;11:e0005659. https://doi.org/10.1371/journal.pntd.0005659. This systematic review describes statistical and modeling methods used to investigate relationships between climate and water-borne diseases, and outlines key analytical challenges. Figure 1 is a notable depiction of approaches to understanding these relationships.
Sterk A, Schijven J, de Nijs T,de Roda Husman AM. Direct and indirect effects of climate change on the risk of infection by water-transmitted pathogens. Environ Sci Technol. 2013:47:12648–12660. Doi:https://doi.org/10.1021/es403549s.
Jagai JS, Castronovo DA, Monchak J, Naumova EN. Seasonality of cryptosporidiosis: a meta-analysis approach. Environ Res. 2009;109:465–78. https://doi.org/10.1016/j.envres.2009.02.008.
Jagai JS, Sarkar R, Castronovo D, Kattula D, McEntee J, Ward H, et al. Seasonality of rotavirus in South Asia: a meta-analysis approach assessing associations with temperature, precipitation, and vegetation index. PLoS One. 2012;7:e38168. https://doi.org/10.1371/journal.pone.0038168.
Lal A, Baker MG, Hales S, French NP. Potential effects of global environmental changes on cryptosporidiosis and giardiasis transmission. Trends Parasitol. 2013;29:83–90. https://doi.org/10.1016/j.pt.2012.10.005.
Levy K, Hubbard AE, Eisenberg JN. Seasonality of rotavirus disease in the tropics: a systematic review and meta-analysis. Int J Epidemiol. 2009;38:1487–96. https://doi.org/10.1093/ije/dyn260.
Kovats RS, Edwards SJ, Charron D, Cowden J, D'Souza RM, Ebi KL, et al. Climate variability and campylobacter infection: an international study. Int J Biometeorol. 2005;49:207–14. https://doi.org/10.1007/s00484-004-0241-3.
Naumova EN, Jagai JS, Matyas B, De Maria A Jr, MacNeill IB, Griffiths JK. Seasonality in six enterically transmitted diseases and ambient temperature. Epidemiol Infect. 2007;135:281–92. https://doi.org/10.1017/s0950268806006698.
Guzman Herrador BR, de Blasio BF, MacDonald E, Nichols G, Sudre B, Vold L, et al. Analytical studies assessing the association between extreme precipitation or temperature and drinking water-related waterborne infections: a review. Environ Health: Glob Access Sci Source. 2015;14:29. https://doi.org/10.1186/s12940-015-0014-y.
Kulinkina AV, Mohan VR, Francis MR, Kattula D, Sarkar R, Plummer JD, et al. Seasonality of water quality and diarrheal disease counts in urban and rural settings in South India. Sci Rep. 2016;6:20521. https://doi.org/10.1038/srep20521.
Phung D, Huang C, Rutherford S, Chu C, Wang X, Nguyen M, et al. Association between climate factors and diarrhoea in a Mekong Delta area. Int J Biometeorol. 2015;59:1321–31. https://doi.org/10.1007/s00484-014-0942-1.
Thiam S, Diene AN, Sy I, Winkler MS, Schindler C, Ndione JA, et al. Association between childhood Diarrhoeal incidence and climatic factors in urban and rural settings in the Health District of Mbour, Senegal. Int J Environ Res Public Health. 2017;14 https://doi.org/10.3390/ijerph14091049.
Wangdi K, Spatial CAC. Temporal patterns of diarrhoea in Bhutan 2003-2013. BMC Infect Dis. 2017;17:507. https://doi.org/10.1186/s12879-017-2611-6.
Yun J, Greiner M, Holler C, Messelhausser U, Rampp A, Klein G. Association between the ambient temperature and the occurrence of human Salmonella and campylobacter infections. Sci Rep. 2016;6:28442. https://doi.org/10.1038/srep28442.
Bhavnani D, Goldstick JE, Cevallos W, Trueba G, Eisenberg JN. Impact of rainfall on diarrheal disease risk associated with unimproved water and sanitation. Am J Trop Med Hyg. 2014;90:705–11. https://doi.org/10.4269/ajtmh.13-0371.
Fonseca PA, Hacon Sde S, Reis VL, Costa D, Brown IF. Using satellite data to study the relationship between rainfall and diarrheal diseases in a Southwestern Amazon basin. Cien Saude Colet. 2016;21:731–42. https://doi.org/10.1590/1413-81232015213.20162015.
Gleason JA, Fagliano JA. Effect of drinking water source on associations between gastrointestinal illness and heavy rainfall in New Jersey. PLoS One. 2017;12:e0173794. https://doi.org/10.1371/journal.pone.0173794.
• Jagai JS, DeFlorio-Barker S, Lin CJ, Hilborn ED, Wade TJ. Sanitary sewer overflows and emergency room visits for gastrointestinal illness: analysis of Massachusetts data, 2006-2007. Environ Health Perspect. 2017;125:117007. https://doi.org/10.1289/ehp2048. This study provides evidence that areas with combined sewer systems may be particularly vulnerable to increases in GI illness following heavy rainfall events.
Jagai JS, Li Q, Wang S, Messier KP, Wade TJ, Extreme Precipitation HED. Emergency room visits for gastrointestinal illness in areas with and without combined sewer systems: an analysis of Massachusetts data, 2003-2007. Environ Health Perspect. 2015;123:873–9. https://doi.org/10.1289/ehp.1408971.
Emont JP, Ko AI, Homasi-Paelate A, Ituaso-Conway N, Nilles EJ. Epidemiological investigation of a diarrhea outbreak in the South Pacific Island nation of Tuvalu during a severe La Nina-associated drought emergency in 2011. Am J Trop Med Hyg. 2017;96:576–82. https://doi.org/10.4269/ajtmh.16-0812.
Thompson CN, Zelner JL, Nhu Tdo H, Phan MV, Hoang Le P, Nguyen Thanh H, et al. The impact of environmental and climatic variation on the spatiotemporal trends of hospitalized pediatric diarrhea in ho chi Minh City, Vietnam. Health Place. 2015;35:147–54. https://doi.org/10.1016/j.healthplace.2015.08.001.
Xu X, Ding G, Zhang Y, Liu Z, Liu Q, Jiang B. Quantifying the impact of floods on bacillary dysentery in Dalian City, China, from 2004 to 2010. Disaster Med Public Health Prep. 2017;11:190–5. https://doi.org/10.1017/dmp.2016.90.
Mellor JE, Levy K, Zimmerman J, Elliott M, Bartram J, Carlton E, et al. Planning for climate change: the need for mechanistic systems-based approaches to study climate change impacts on diarrheal diseases. Sci Total Environ. 2016;548-549:82–90. https://doi.org/10.1016/jscitotenv2015.12.087.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2224–60. https://doi.org/10.1016/S0140-6736(12)61766-8.
Murray C, Lopez A, editors. The global burden of disease : a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996.
WHO. World health report 2002: Reducing risks, promoting healthy life. Geneva2002.
•• Howard G, Calow R, Macdonald A, Climate Change BJ. Water and sanitation: likely impacts and emerging trends for action. Annu Rev Environ Resour. 2016;41:253–76. https://doi.org/10.1146/annurev-environ-110615-085856. This is an extensive review of the relationship between climate change and water and sanitation services, emphasizing management and policy responses to improve the resilience of these services.
IPCC. Summary for policymakers. In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, Chatterjee M, Ebi KL, Estrada YO, Genova RC, Girma B, Kissel ES, Levy AN, MacCracken S, Mastrandrea PR, White LL, editors. Climate change, vol. 2014. Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel of Climate Change. Cambridge University Press; 2014. p. 1–32.
Carlton EJ, Eisenberg JN, Goldstick J, Cevallos W, Trostle J, Levy K. Heavy rainfall events and diarrhea incidence: the role of social and environmental factors. Am J Epidemiol. 2014;179:344–52. https://doi.org/10.1093/aje/kwt279.
• Martinez PP, King AA, Yunus M, Faruque AS, Differential PM. Enhanced response to climate forcing in diarrheal disease due to rotavirus across a megacity of the developing world. Proc Natl Acad Sci U S A. 2016;113:4092–7. https://doi.org/10.1073/pnas.1518977113. This study describes associations between extreme precipitation and gastrointestinal-related hospital admissions, providing evidence that risks may vary by age and season.
Bush KF, O'Neill MS, Li S, Mukherjee B. Hu H, Ghosh S et al. associations between extreme precipitation and gastrointestinal-related hospital admissions in Chennai, India. Environ Health Perspect. 2014;122:249–54. https://doi.org/10.1289/ehp.1306807.
Xu Z, Liu Y, Ma Z, Sam Toloo G, Hu W, Tong S. Assessment of the temperature effect on childhood diarrhea using satellite imagery. Sci Rep. 2014;4:5389. https://doi.org/10.1038/srep05389.
Pickering AJ,Davis J. Freshwater availability and water fetching distance affect child health in sub-Saharan Africa. Environ Sci Technol. 2012;46:2391–7. https://doi.org/10.1021/es203177v.
Eisenhauer IF, Hoover CM, Remais JV, Monaghan A, Celada M, Carlton EJ. Estimating the risk of domestic water source contamination following precipitation events. Am J Trop Med Hyg. 2016;94(6):1403–6. https://doi.org/10.4269/ajtmh.15-0600.
Boithias L, Choisy M, Souliyaseng N, Jourdren M, Quet F, Buisson Y, et al. Hydrological regime and water shortage as drivers of the seasonal incidence of diarrheal diseases in a tropical montane environment. PLoS Negl Trop Dis. 2016;10:e0005195. https://doi.org/10.1371/journal.pntd.0005195.
Kniel KE, Spanninger P. Preharvest food safety under the influence of a changing climate. Microbiol Spectr. 2017;5 https://doi.org/10.1128/microbiolspec.PFS-0015-2016.
Liu C, Hofstra N, Franz E. Impacts of climate change on the microbial safety of pre-harvest leafy green vegetables as indicated by Escherichia coli O157 and Salmonella spp. Int J Food Microbiol. 2013;163(28):119–28. https://doi.org/10.1016/j.ijfoodmicro.2013.02.026.
Hellberg RS, Chu E. Effects of climate change on the persistence and dispersal of foodborne bacterial pathogens in the outdoor environment: a review. Crit Rev Microbiol. 2016;42:548–72. https://doi.org/10.3109/1040841x.2014.972335.
Miraglia M, Marvin HJ, Kleter GA, Battilani P, Brera C, Coni E, et al. Climate change and food safety: an emerging issue with special focus on Europe. Food Chem Toxicol: Int J Publ Br Ind Biol Res Assoc. 2009;47:1009–21. https://doi.org/10.1016/jfct2009.02.005.
• Hodges M, Belle JH, Carlton EJ, Liang S, Li H, Luo W, et al. Delays in reducing waterborne and water-related infectious diseases in China under climate change. Nat Clim Chang. 2014;4:1109–15. https://doi.org/10.1038/nclimate2428. This study is one of the few projections of water borne diseases under future climate scenarios that jointly considers the impact of different levels of water and sanitation infrastructure investment on future disease burden.
Mellor J, Kumpel E, Ercumen A, Zimmerman J. Systems Approach to Climate, Water, and Diarrhea in Hubli-Dharwad, India. Environ Sci Technol. 2016;50:13042–51. https://doi.org/10.1021/acs.est.6b02092.
Bonabeau E. Agent-based modeling: methods and techniques for simulating human systems. Proc Natl Acad Sci U S A. 2002;99(Suppl 3):7280–7. https://doi.org/10.1073/pnas.082080899.
Stephen DM, Barnett AG. Using microsimulation to estimate the future health and economic costs of salmonellosis under climate change in Central Queensland, Australia. Environ Health Perspect. 2017;125:127001. https://doi.org/10.1289/ehp1370.
Rutter CM, Zaslavsky AM, Feuer EJ. Dynamic microsimulation models for health outcomes: a review. Med Decis Mak: Int J Soc Med Decis Mak. 2011;31:10–8. https://doi.org/10.1177/0272989x10369005.
Institute of Medicine Forum on Microbial Threats. The National Academies Collection: Reports funded by National Institutes of Health. In: Global issues in water, sanitation, and health: workshop summary. Washington (DC): National Academy of Sciences; 2009.
Rose JB, Epstein PR, Lipp EK, Sherman BH, Bernard SM, Patz JA. Climate variability and change in the United States: potential impacts on water- and foodborne diseases caused by microbiologic agents. Environ Health Perspect. 2001;109(Suppl 2):211–21.
USGCRP. The impacts of climate change on human health in the United States: a scientific assessment. Washington, DC: U.S. Global Change Research Program; 2016.
Perry D, Bennett D, Boudjou U, Hahn M, McLellan S, Elizabeth S. Effect of climate change on sewer overflows in Milwaukee. Proc Water Environ Fed. 2012;2012:1857–66. https://doi.org/10.2175/193864712811725546.
• Mukabutera A, Thomson DR, Hedt-Gauthier BL, Atwood S, Basinga P, Nyirazinyoye L, et al. Exogenous factors matter when interpreting the results of an impact evaluation: a case study of rainfall and child health programme intervention in Rwanda. Tropical Med Int Health. 2017;22:1505–13. https://doi.org/10.1111/tmi.12995. This study highlights the importance of considering precipitation as a confounder when assessing child health intervention outcomes.
• Climate-resilient water safety plans. Managing health risks associated with climate variability and change. Geneva: World Health Organization; 2017. This document outlines strategies for future drinking water safety in a changing climate with a focus on identification of hazards and development of control measures.
Howard G, Bartram J. Vision 2030: the resilience of water supply and sanitation in the face of climate change. Technical report. Geneva: WHO; 2009.
Howard G, Charles K, Pond K, Brookshaw A, Hossian R, Bartram J. Securing 2020 vision for 2030: climate change and ensuring resilience in water and sanitation services. J Water Climate. 2010;01(1):2–1655.
Acknowledgments
Karen Levy is supported by the National Institute for Allergy and Infectious Diseases, NIH (grant 1K01AI103544). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Water and Health
Rights and permissions
About this article
Cite this article
Levy, K., Smith, S.M. & Carlton, E.J. Climate Change Impacts on Waterborne Diseases: Moving Toward Designing Interventions. Curr Envir Health Rpt 5, 272–282 (2018). https://doi.org/10.1007/s40572-018-0199-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-018-0199-7