Abstract
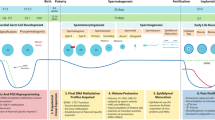
Human populations are exposed to a wide spectrum of environmental contaminants, some of which are considered reproductive toxins. The influence of such toxins on the male reproductive system has been investigated extensively in animal models, while epidemiological studies seek to understand the effect of human exposures. The basic tenant of epidemiological studies in male human reproduction is to infer how one or more substances alter the hormonal profile, seminal characteristics, or both. Determining if a substance alters semen quality may not always provide the underlying mechanism. The mechanisms by which toxins may alter human sperm and semen quality are typically examined as a function of hormonal changes and cellular damage. The possibility that more subtle epigenetic alterations underlie some of the reproductive changes has, until recently, received little attention. In this review, we discuss the roles of epigenetics in human spermatogenesis, while considering the impact of reproductive toxicants on the epigenome.

Similar content being viewed by others
Abbreviations
- BTB:
-
Blood-testis barrier
- BEB:
-
Blood-epididymis barrier
- LC:
-
Leydig cell
- SC:
-
Sertoli cell
- SSC:
-
Spermatogenic stem cell
- sncRNA:
-
Small noncoding RNAs
- BPA:
-
Bisphenol A
- DEHP:
-
Di(2-ethylhexyl) phthalate
- DBP:
-
Di-n-butyl phthalate
- e.d.:
-
Embryonic day
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rolland M, Le Moal J, Wagner V, et al. Decline in semen concentration and morphology in a sample of 26 609 men close to general population between 1989 and 2005 in France. Human Reproduction (Oxford, England). 2013;28(2):462–70. doi:10.1093/humrep/des415.
Jin J-M, Yang W-X. Molecular regulation of hypothalamus–pituitary–gonads axis in males. Gene. 2014;551(1):15–25. doi:10.1016/j.gene.2014.08.048.
Amann RP. The cycle of the seminiferous epithelium in humans: a need to revisit? J Androl. 2008;29(5):469–87. doi:10.2164/jandrol.107.004655.
Hai Y, Hou J, Liu Y, et al. The roles and regulation of Sertoli cells in fate determinations of spermatogonial stem cells and spermatogenesis. Semin Cell Dev Biol. 2014;29:66–75. doi:10.1016/j.semcdb.2014.04.007 .A comprehensive review of the importance of SCs in reproductive health
Aziz N, Fear S, Taylor C, et al. Human sperm head morphometric distribution and its influence on human fertility. Fertil Steril. 1998;70(5):883–91. doi:10.1016/S0015-0282(98)00317-3.
Balhorn R. The protamine family of sperm nuclear proteins. Genome Biol. 2007;8(9):227. doi:10.1186/gb-2007-8-9-227.
Brunner AM, Nanni P, Mansuy IM. Epigenetic marking of sperm by post-translational modification of histones and protamines. Epigenetics & Chromatin. 2014;7:2. doi:10.1186/1756-8935-7-2.
Hammoud SS, Nix DA, Zhang H, et al. Distinctive chromatin in human sperm packages genes for embryo development. Nature. 2009;460(7254):473–8 .http://www.nature.com/nature/journal/v460/n7254/suppinfo/nature08162_S1.html.
Carone BR, Hung J-H, Hainer SJ, et al. High resolution mapping of chromatin packaging in mouse ES cells and sperm. Dev Cell. 2014;30(1):11–22. doi:10.1016/j.devcel.2014.05.024.
Samans B, Yang Y, Krebs S, et al. Uniformity of nucleosome preservation pattern in mammalian sperm and its connection to repetitive DNA elements. Dev Cell. 2014;30(1):23–35. doi:10.1016/j.devcel.2014.05.023.
Johnson GD, Jodar M, Pique-Regi R et al. Nuclease footprints in sperm project past and future chromatin regulatory events. Sci Rep. 2016;6:25864. doi:10.1038/srep25864.
Wakeling SI, Miles DC, Western PS. Identifying disruptors of male germ cell development by small molecule screening in ex vivo gonad cultures. BMC Research Notes. 2013;6:168. doi:10.1186/1756-0500-6-168.
Juul A, Almstrup K, Andersson A-M, et al. Possible fetal determinants of male infertility. Nat Rev Endocrinol. 2014;10(9):553–62. doi:10.1038/nrendo.2014.97.
Pitetti J-L, Calvel P, Zimmermann C, et al. An essential role for insulin and IGF1 receptors in regulating Sertoli cell proliferation, testis size, and FSH action in mice. Mol Endocrinol. 2013;27(5):814–27. doi:10.1210/me.2012-1258.
Jørgensen A, Nielsen JE, Perlman S, et al. Ex vivo culture of human fetal gonads: manipulation of meiosis signalling by retinoic acid treatment disrupts testis development. Hum Reprod. 2015;30(10):2351–63. doi:10.1093/humrep/dev194.
Altman E, Yango P, Moustafa R, et al. Characterization of human spermatogonial stem cell markers in fetal, pediatric, and adult testicular tissues. Reproduction (Cambridge, England). 2014;148(4):417–27. doi:10.1530/REP-14-0123.
Wu H, Hauser R, Krawetz SA, et al. Environmental susceptibility of the sperm epigenome during windows of male germ cell development. Current environmental health reports. 2015;2(4):356–66. doi:10.1007/s40572-015-0067-7.
Morris AJ, Taylor MF, Morris ID. Leydig cell apoptosis in response to ethane Dimethanesulphonate after both in vivo and in vitro treatment. J Androl. 1997;18(3):274–80. doi:10.1002/j.1939-4640.1997.tb01919.x.
Kelce WR, Zirkin BR. Mechanism by which ethane dimethanesulfonate kills adult rat leydig cells: involvement of intracellular glutathione. Toxicol Appl Pharmacol. 1993;120(1):80–8. doi:10.1006/taap.1993.1089.
Guo J, Zhou H, Su Z, et al. Comparison of cell types in the rat leydig cell lineage after ethane dimethanesulfonate treatment. Reproduction. 2013;145(4):371–80. doi:10.1530/rep-12-0465.
Woolveridge I, de Boer-Brouwer M, Taylor MF, et al. Apoptosis in the rat spermatogenic epithelium following androgen withdrawal: changes in apoptosis-related genes. Biol Reprod. 1999;60(2):461–70. doi:10.1095/biolreprod60.2.461.
Nandi S, Banerjee PP, Zirkin BR. Germ cell apoptosis in the testes of Sprague Dawley rats following testosterone withdrawal by ethane 1,2-dimethanesulfonate administration: relationship to Fas? Biol Reprod. 1999;61(1):70–5. doi:10.1095/biolreprod61.1.70.
Sharpe RM, Maddocks S, Kerr JB. Cell-cell interactions in the control of spermatogenesis as studied using leydig cell destruction and testosterone replacement. Am J Anat. 1990;188(1):3–20. doi:10.1002/aja.1001880103.
Tarulli GA, Stanton PG, Meachem SJ. Is the adult Sertoli cell terminally differentiated? Biol Reprod. 2012;87(1):13 . doi:10.1095/biolreprod.111.095091.1-1
Rebourcet D, O’Shaughnessy PJ, Monteiro A, et al. Sertoli cells maintain leydig cell number and peritubular Myoid cell activity in the adult mouse testis. PLoS One. 2014;9(8):e105687. doi:10.1371/journal.pone.0105687.
Qiu L, Zhang X, Zhang X, et al. Sertoli cell is a potential target for perfluorooctane sulfonate–induced reproductive dysfunction in male mice. Toxicol Sci. 2013;135(1):229–40. doi:10.1093/toxsci/kft129.
Xiao X, Mruk DD, Tang EI, et al. Environmental toxicants perturb human Sertoli cell adhesive function via changes in F-actin organization mediated by actin regulatory proteins. Hum Reprod. 2014;29(6):1279–91. doi:10.1093/humrep/deu011.
Mazaud-Guittot S. Dissecting the phthalate-induced Sertoli cell injury: the fragile balance of proteases and their inhibitors. Biol Reprod. 2011;85(6):1091–3. doi:10.1095/biolreprod.111.095976.
Desdoits-Lethimonier C, Albert O, Le Bizec B, et al. Human testis steroidogenesis is inhibited by phthalates. Hum Reprod. 2012;27(5):1451–9. doi:10.1093/humrep/des069.
Hauser R, Meeker JD, Singh NP, et al. DNA damage in human sperm is related to urinary levels of phthalate monoester and oxidative metabolites. Hum Reprod. 2007;22(3):688–95. doi:10.1093/humrep/del428.
Duty SM, Silva MJ, Barr DB, et al. Phthalate exposure and human semen parameters. Epidemiology. 2003;14(3):269–77. doi:10.1097/01.ede.0000059950.11836.16.
Zhang Y, Cao Y, Shi H, et al. Could exposure to phthalates speed up or delay pubertal onset and development? A 1.5-year follow-up of a school-based population. Environ Int. 2015;83:41–9. doi:10.1016/j.envint.2015.06.005.
Liu C, Qian P, Yang L et al. Pubertal exposure to di-(2-ethylhexyl)-phthalate inhibits G9a-mediated histone methylation during spermatogenesis in mice. Archives of Toxicology. 2015:1–15. doi:10.1007/s00204–015–1529-2.
Habert R, Muczynski V, Grisin T, et al. Concerns about the widespread use of rodent models for human risk assessments of endocrine disruptors. Reproduction (Cambridge, England). 2014;147(4):R119–R29. doi:10.1530/REP-13-0497.
Johnson KJ, Heger NE, Boekelheide K. Of mice and men (and rats): phthalate-induced fetal testis endocrine disruption is species-dependent. Toxicol Sci. 2012;129(2):235–48. doi:10.1093/toxsci/kfs206 .An overview of the use of rodent models in assessing phthalate-induced testicular dysgenesis syndrome
Araki A, Mitsui T, Miyashita C, et al. Association between maternal exposure to di(2-ethylhexyl) phthalate and reproductive hormone levels in fetal blood: the Hokkaido study on environment and children's health. PLoS One. 2014;9(10):e109039. doi:10.1371/journal.pone.0109039.
Tomonari Y, Kurata Y, David RM, et al. Effect of di(2-ethylhexyl) phthalate (DEHP) on genital organs from juvenile common marmosets: I. Morphological and biochemical investigation in 65-week toxicity study. J Toxic Environ Health A. 2006;69(17):1651–72. doi:10.1080/15287390600630054.
Levi M, Hasky N, Stemmer SM, et al. Anti-Müllerian hormone is a marker for chemotherapy-induced testicular toxicity. Endocrinology. 2015;156(10):3818–27. doi:10.1210/en.2015-1310.
Hermann BP, Sukhwani M, Lin C-C, et al. Characterization, cryopreservation and ablation of spermatogonial stem cells in adult rhesus macaques. Stem cells (Dayton, Ohio). 2007;25(9):2330–8. doi:10.1634/stemcells.2007-0143.
Gajjar R, Miller SD, Meyers KE, et al. Fertility preservation in patients receiving cyclophosphamide therapy for renal disease. Pediatr Nephrol. 2014;30(7):1099–106. doi:10.1007/s00467-014-2897-1.
Kangasniemi M, Wilson G, Huhtaniemi I, et al. Protection against procarbazine-induced testicular damage by GnRH-agonist and antiandrogen treatment in the rat. Endocrinology. 1995;136(8):3677–80. doi:10.1210/endo.136.8.7628410.
Kreuser ED, D. K, E. T. The role of LHRH-analogues in protecting gonadal functions during chemotherapy and irradiation. Eur Urol. 1993;23(1):157–63 .discussion 63-4
Mamsen LS, Lutterodt MC, Andersen EW, et al. Cigarette smoking during early pregnancy reduces the number of embryonic germ and somatic cells. Hum Reprod. 2010;25(11):2755–61. doi:10.1093/humrep/deq215.
Sobinoff AP, Sutherland JM, Beckett EL, et al. Damaging legacy: maternal cigarette smoking has long-term consequences for male offspring fertility. Hum Reprod. 2014;29(12):2719–35. doi:10.1093/humrep/deu235.
Audi SSSS. Effect of cigarette smoke on body weight, food intake and reproductive organs in adult albino rats. Indian J Exp Biol. 44(7):562–5.
Esakky P, Hansen DA, Drury AM, et al. Cigarette smoke condensate induces aryl hydrocarbon receptor-dependent changes in gene expression in spermatocytes. Reprod Toxicol. 2012;34(4):665–76. doi:10.1016/j.reprotox.2012.10.005.
Ku WW, Wine RN, Chae BY, et al. Spermatocyte toxicity of 2-methoxyethanol (ME) in rats and Guinea pigs: evidence for the induction of apoptosis. Toxicol Appl Pharmacol. 1995;134(1):100–10. doi:10.1006/taap.1995.1173.
Sams C, Jones K, Warren N, et al. Towards a biological monitoring guidance value for acrylamide. Toxicol Lett. 2015;237(1):30–7. doi:10.1016/j.toxlet.2015.05.018.
Nixon BJ, Stanger SJ, Nixon B, et al. Chronic exposure to acrylamide induces DNA damage in male germ cells of mice. Toxicol Sci. 2012;129(1):135–45. doi:10.1093/toxsci/kfs178 .This study demonstrates that chronic exposure at physiologically relevant doses of acrylamide , a potential human carcinogen , can alter sperm DNA integrity in mice
Nixon BJ, Katen AL, Stanger SJ, et al. Mouse spermatocytes express CYP2E1 and respond to acrylamide exposure. PLoS One. 2014;9(5):e94904. doi:10.1371/journal.pone.0094904.
DuTeaux SB, Hengel MJ, DeGroot DE, et al. Evidence for trichloroethylene Bioactivation and adduct formation in the rat epididymis and efferent ducts. Biol Reprod. 2003;69(3):771–9. doi:10.1095/biolreprod.102.014845.
Dacheux J-L, Dacheux F. New insights into epididymal function in relation to sperm maturation. Reproduction. 2014;147(2):R27–42. doi:10.1530/rep-13-0420 .A review of the influence of the epididymal proteins and environment on sperm maturation in preparation for fertilization
Sullivan R, Saez F. Epididymosomes, prostasomes, and liposomes: their roles in mammalian male reproductive physiology. Reproduction. 2013;146(1):R21–35. doi:10.1530/rep-13-0058.
Shum WW, Smith TB, Cortez-Retamozo V, et al. Epithelial basal cells are distinct from dendritic cells and macrophages in the mouse epididymis. Biol Reprod. 2014;90(5):90 . doi:10.1095/biolreprod.113.116681.1-10
Mathur SS. Sperm motility on postcoital testing correlates with male autoimmunity to sperm. Fertil Steril. 41(1):81–7.
Close CE, Roberts PL, Berger RE. Cigarettes, alcohol and marijuana are related to pyospermia in infertile men. J Urol. 1990;144(4):900–3.
Zhu Z, Xu W, Dai J, et al. The alteration of protein profile induced by cigarette smoking via oxidative stress in mice epididymis. Int J Biochem Cell Biol. 2013;45(3):571–82. doi:10.1016/j.biocel.2012.12.007.
Kaur S, Bansal MP. Protective role of dietary-supplemented selenium and vitamin E in heat-induced apoptosis and oxidative stress in mice testes. Andrologia. 2015;47(10):1109–19. doi:10.1111/and.12390.
Hendin BN, Kolettis PN, Sharma RK, et al. Varicocele is associated with elevated spermatozoal reactive oxygen species production and diminished seminal plasma antioxidant capacity. J Urol. 1999;161(6):1831–4. doi:10.1016/S0022-5347(05)68818-0.
KP N, SSR A, FF P, et al. Relationship of interleukin-6 with semen characteristics and oxidative stress in patients with varicocele. Urology. 2004;64(5):1010–3. doi:10.1016/j.urology.2004.05.045.
Plongthongkum N, Diep DH, Zhang K. Advances in the profiling of DNA modifications: cytosine methylation and beyond. Nat Rev Genet. 2014;15(10):647–61. doi:10.1038/nrg3772.
Hammoud Saher S, Low Diana HP, Yi C, et al. Chromatin and transcription transitions of mammalian adult germline stem cells and spermatogenesis. Cell Stem Cell. 2014;15(2):239–53. doi:10.1016/j.stem.2014.04.006.
Molaro A, Hodges E, Fang F, et al. Sperm methylation profiles reveal features of epigenetic inheritance and evolution in primates. Cell. 2011;146(6):1029–41. doi:10.1016/j.cell.2011.08.016.
Jiang L, Zhang J, Wang J-J, et al. Sperm, but not oocyte, DNA methylome is inherited by zebrafish early embryos. Cell. 2013;153(4):773–84. doi:10.1016/j.cell.2013.04.041.
Sigurdsson MI, Smith AV, Bjornsson HT, et al. Distribution of a marker of germline methylation differs between major families of transposon-derived repeats in the human genome. Gene. 2012;492(1):104–9. doi:10.1016/j.gene.2011.10.046.
Smith ZD, Chan MM, Mikkelsen TS, et al. A unique regulatory phase of DNA methylation in the early mammalian embryo. Nature. 2012;484(7394):339–44. doi:10.1038/nature10960.
Jones EL, Mudrak O, Zalensky AO. Kinetics of human male pronuclear development in a heterologous ICSI model. J Assist Reprod Genet. 2010;27(6):277–83. doi:10.1007/s10815-010-9402-y.
Messerschmidt DM, Knowles BB, Solter D. DNA methylation dynamics during epigenetic reprogramming in the germline and preimplantation embryos. Genes Dev. 2014;28(8):812–28. doi:10.1101/gad.234294.113.
Donkin I, Versteyhe S, Ingerslev Lars R, et al. Obesity and bariatric surgery drive epigenetic variation of spermatozoa in humans. Cell Metab. 2016;23:1–10. doi:10.1016/j.cmet.2015.11.004.
Denham J, O'Brien BJ, Harvey JT, et al. Genome-wide sperm DNA methylation changes after 3 months of exercise training in humans. Epigenomics. 2015;7(5):717–31. doi:10.2217/epi.15.29.
Miao M, Zhou X, Li Y, et al. LINE-1 hypomethylation in spermatozoa is associated with bisphenol a exposure. Andrologie. 2014;2(1):138–44. doi:10.1111/j.2047-2927.2013.00166.x.
Radford EJ, Ito M, Shi H, et al. In utero undernourishment perturbs the adult sperm methylome and is linked to metabolic disease transmission. Science (New York, NY). 2014;345(6198):1255903. doi:10.1126/science.1255903.
Jenkins TG, Aston KI, Trost C, et al. Intra-sample heterogeneity of sperm DNA methylation. Mol Hum Reprod. 2015;21(4):313–9. doi:10.1093/molehr/gau115.
Aston KI, Uren PJ, Jenkins TG, et al. Aberrant sperm DNA methylation predicts male fertility status and embryo quality. Fertil Steril. 2015;104(6):1388–97. doi:10.1016/j.fertnstert.2015.08.019 .e5. This study provides evidence that the sperm methylome can predict fertility and embryonic health
Utsuno H, Miyamoto T, Oka K, et al. Morphological alterations in protamine-deficient spermatozoa. Hum Reprod. 2014;29(11):2374–81. doi:10.1093/humrep/deu225.
Iranpour FG. Impact of sperm chromatin evaluation on fertilization rate in intracytoplasmic sperm injection. Adv Biol Res. 2014;3:229. doi:10.4103/2277-9175.145719.
Nili HA, Mozdarani H, Aleyasin A. Correlation of sperm DNA damage with protamine deficiency in Iranian subfertile men. Reprod BioMed Online. 2009;18(4):479–85. doi:10.1016/S1472-6483(10)60123-X.
Fortes MRS, Satake N, Corbet DH, et al. Sperm protamine deficiency correlates with sperm DNA damage in Bos indicus bulls. Andrologie. 2014;2(3):370–8. doi:10.1111/j.2047-2927.2014.00196.x.
Collins AR. Measuring oxidative damage to DNA and its repair with the comet assay. Biochim Biophys Acta Gen Subj. 2014;1840(2):794–800. doi:10.1016/j.bbagen.2013.04.022.
Soumillon M, Necsulea A, Weier M, et al. Cellular source and mechanisms of high transcriptome complexity in the mammalian testis. Cell Rep. 2013;3(6):2179–90. doi:10.1016/j.celrep.2013.05.031.
Sendler E, Johnson GD, Mao S, et al. Stability, delivery and functions of human sperm RNAs at fertilization. Nucleic Acids Res. 2013;41(7):4104–17. doi:10.1093/nar/gkt132.
Jodar M, Sendler E, Krawetz SA. The protein and transcript profiles of human semen. Cell Tissue Res. 2015;363(1):85–96. doi:10.1007/s00441-015-2237-1 .A review of the information that high-throughput technologies have revealed about the structure and function of sperm and seminal factors
Johnson GD, Sendler E, Lalancette C, et al. Cleavage of rRNA ensures translational cessation in sperm at fertilization. Mol Hum Reprod. 2011;17(12):721–6. doi:10.1093/molehr/gar054.
Jodar M, Selvaraju S, Sendler E, et al. The presence, role and clinical use of spermatozoal RNAs. Hum Reprod Update. 2013;19(6):604–24. doi:10.1093/humupd/dmt031.
Fang P, Zeng P, Wang Z, et al. Estimated diversity of messenger RNAs in each murine spermatozoa and their potential function during early zygotic development. Biol Reprod. 2014;90(5):94 . doi:10.1095/biolreprod.114.117788.1-11
Sharma U, Conine CC, Shea JM, et al. Biogenesis and function of tRNA fragments during sperm maturation and fertilization in mammals. Science. 2016;351(6271):391–6. doi:10.1126/science.aad6780 .This study demonstrates the importance of sperm RNAs obtained during epididymal transit on offspring development and health , in a mouse model
Liu W-M, Pang RTK, Chiu PCN, et al. Sperm-borne microRNA-34c is required for the first cleavage division in mouse. Proc Natl Acad Sci U S A. 2012;109(2):490–4. doi:10.1073/pnas.1110368109.
Yuan S, Tang C, Zhang Y, et al. Mir-34b/c and mir-449a/b/c are required for spermatogenesis, but not for the first cleavage division in mice. Biology Open. 2015;4(2):212–23. doi:10.1242/bio.201410959.
Jodar M, Sendler E, Moskovtsev SI, et al. Absence of sperm RNA elements correlates with idiopathic male infertility. Sci Transl Med. 2015;7(295):295re6-re6. doi:10.1126/scitranslmed.aab1287 .This study identifies germline RNAs with potential roles as biomarkers of male infertility
García-López J, Alonso L, Cárdenas DB, et al. Diversity and functional convergence of small noncoding RNAs in male germ cell differentiation and fertilization. RNA. 2015;21(5):946–62. doi:10.1261/rna.048215.114.
Starega-Roslan J, Galka-Marciniak P, Krzyzosiak WJ. Nucleotide sequence of miRNA precursor contributes to cleavage site selection by dicer. Nucleic Acids Res. 2015;43(22):10939–51. doi:10.1093/nar/gkv968.
Rajan KS, Ramasamy S. Retrotransposons and piRNA: the missing link in central nervous system. Neurochem Int. 2014;77:94–102. doi:10.1016/j.neuint.2014.05.017.
Watanabe T. Cheng E-c, Zhong M et al. retrotransposons and pseudogenes regulate mRNAs and lncRNAs via the piRNA pathway in the germline. Genome Res. 2015;25(3):368–80. doi:10.1101/gr.180802.114.
Klengel T, Dias BG, Ressler KJ. Models of intergenerational and transgenerational transmission of risk for psychopathology in mice. Neuropsychopharmacology. 2016;41(1):219–31. doi:10.1038/npp.2015.249 .An overview of the transmission of neurological disease risk across generations , a concept that can be extended to environmental exposures
Gapp K, Jawaid A, Sarkies P, et al. Implication of sperm RNAs in transgenerational inheritance of the effects of early trauma in mice. Nat Neurosci. 2014;17(5):667–9. doi:10.1038/nn.3695.
Fullston T, Ohlsson Teague EMC, Palmer NO, et al. Paternal obesity initiates metabolic disturbances in two generations of mice with incomplete penetrance to the F2 generation and alters the transcriptional profile of testis and sperm microRNA content. FASEB J. 2013;27(10):4226–43. doi:10.1096/fj.12-224048.
Dias BG, Ressler KJ. Parental olfactory experience influences behavior and neural structure in subsequent generations. Nat Neurosci. 2014;17(1):89–96. doi:10.1038/nn.3594.
Cossetti C, Lugini L, Astrologo L, et al. Soma-to-germline transmission of RNA in mice xenografted with human tumour cells: possible transport by exosomes. PLoS One. 2014;9(7):e101629. doi:10.1371/journal.pone.0101629 .A proof-of-principle study demonstrating that mouse sperm can acquire RNAs from somatic cells in distant tissues
Johnson GD, Mackie P, Jodar M, et al. Chromatin and extracellular vesicle associated sperm RNAs. Nucleic Acids Res. 2015;43(14):6847–59. doi:10.1093/nar/gkv591.
Chen Q, Yan M, Cao Z, et al. Sperm tsRNAs contribute to intergenerational inheritance of an acquired metabolic disorder. Science. 2016;351(6271):397–400. doi:10.1126/science.aad7977.
Shea Jeremy M, Serra Ryan W, Carone Benjamin R, et al. Genetic and epigenetic variation, but not diet, shape the sperm methylome. Dev Cell. 2015;35(6):750–8. doi:10.1016/j.devcel.2015.11.024.
Lambrot R, Xu C, Saint-Phar S, et al. Low paternal dietary folate alters the mouse sperm epigenome and is associated with negative pregnancy outcomes. Nat Commun. 2013;4:2889. doi:10.1038/ncomms3889.
Terashima M, Barbour S, Ren J, et al. Effect of high fat diet on paternal sperm histone distribution and male offspring liver gene expression. Epigenetics. 2015;10(9):861–71. doi:10.1080/15592294.2015.1075691.
van de Werken C, van der Heijden GW, Eleveld C, et al. Paternal heterochromatin formation in human embryos is H3K9/HP1 directed and primed by sperm-derived histone modifications. Nat Commun. 2014;5:5868. doi:10.1038/ncomms6868.
Guerrero-Bosagna C, Covert TR, Haque MM, et al. Epigenetic transgenerational inheritance of vinclozolin induced mouse adult onset disease and associated sperm epigenome biomarkers. Reproductive toxicology (Elmsford, NY). 2012;34(4):694–707. doi:10.1016/j.reprotox.2012.09.005.
Guerrero-Bosagna C, Savenkova M, Haque MM, et al. Environmentally induced epigenetic transgenerational inheritance of altered Sertoli cell transcriptome and epigenome: molecular etiology of male infertility. PLoS One. 2013;8(3):e59922. doi:10.1371/journal.pone.0059922.
Doyle TJ, Bowman JL, Windell VL, et al. Transgenerational effects of di-(2-ethylhexyl) phthalate on testicular germ cell associations and spermatogonial stem cells in mice. Biol Reprod. 2013;88(5):112. doi:10.1095/biolreprod.112.106104.
Dobrzyńska M, Tyrkiel E, Derezińska E, et al. Two generation reproductive and developmental toxicity following subchronic exposure of pubescent male mice to di(2-ethylhexyl)phthalate. Annals of Agricultural and Environmental Medicine. 2012;19(1):31–7.
Manikkam M, Tracey R, Guerrero-Bosagna C, et al. Plastics derived endocrine disruptors (BPA, DEHP and DBP) induce epigenetic transgenerational inheritance of obesity, reproductive disease and sperm epimutations. PLoS One. 2013;8(1):e55387. doi:10.1371/journal.pone.0055387.
Iqbal K, Tran DA, Li AX, et al. Deleterious effects of endocrine disruptors are corrected in the mammalian germline by epigenome reprogramming. Genome Biol. 2015;16(1):59. doi:10.1186/s13059-015-0619-z.
Lombó M, Fernández-Díez C, González-Rojo S, et al. Transgenerational inheritance of heart disorders caused by paternal bisphenol a exposure. Environ Pollut. 2015;206:667–78. doi:10.1016/j.envpol.2015.08.016.
Li G, Chang H, Xia W, et al. F0 maternal BPA exposure induced glucose intolerance of F2 generation through DNA methylation change in Gck. Toxicol Lett. 2014;228(3):192–9. doi:10.1016/j.toxlet.2014.04.012.
Doshi T, D’souza C, Vanage G. Aberrant DNA methylation at Igf2–H19 imprinting control region in spermatozoa upon neonatal exposure to bisphenol a and its association with post implantation loss. Mol Biol Rep. 2013;40(8):4747–57. doi:10.1007/s11033-013-2571-x.
Eustache F, Mondon F, Canivenc-Lavier MC, et al. Chronic dietary exposure to a low-dose mixture of Genistein and vinclozolin modifies the reproductive Axis, testis transcriptome, and fertility. Environ Health Perspect. 2009;117(8):1272–9. doi:10.1289/ehp.0800158.
Gazo I, Linhartova P, Shaliutina A, et al. Influence of environmentally relevant concentrations of vinclozolin on quality, DNA integrity, and antioxidant responses of sterlet Acipenser ruthenus spermatozoa. Chem Biol Interact. 2013;203(2):377–85. doi:10.1016/j.cbi.2013.01.004.
Stouder C, Paoloni-Giacobino A. Transgenerational effects of the endocrine disruptor vinclozolin on the methylation pattern of imprinted genes in the mouse sperm. Reproduction. 2010;139(2):373–9. doi:10.1530/rep-09-0340.
O'Flaherty CM, Chan PT, Hales BF, et al. Sperm chromatin structure components are differentially repaired in cancer survivors. J Androl. 2012;33(4):629–36. doi:10.2164/jandrol.111.015388.
Maselli J, Hales BF, Chan P, et al. Exposure to bleomycin, etoposide, and cis-platinum alters rat sperm chromatin integrity and sperm head protein profile. Biol Reprod. 2012;86(5):166 . doi:10.1095/biolreprod.111.098616.1-10
Berthaut I, Montjean D, Dessolle L, et al. Effect of temozolomide on male gametes: an epigenetic risk to the offspring? J Assist Reprod Genet. 2013;30(6):827–33. doi:10.1007/s10815-013-9999-8.
Zhu H, Li K, Liang J, et al. Changes in the levels of DNA methylation in testis and liver of SD rats neonatally exposed to 5-aza-2′-deoxycytidine and cadmium. J Appl Toxicol. 2011;31(5):484–95. doi:10.1002/jat.1673.
Acknowledgments
The graduate student assistantship to M.S.E. from Wayne State University’s Center for Molecular Medicine and Genetics is gratefully acknowledged. This work was supported in part by the Charlotte B. Failing Professorship to S.A.K.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
M.S. Estill and S.A. Krawetz declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article contains references to studies with human or animal subjects performed by one of the authors. All studies involving human biological specimens were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Additional information
This article is part of the Topical Collection on Environmental Epigenetics
Rights and permissions
About this article
Cite this article
Estill, M.S., Krawetz, S.A. The Epigenetic Consequences of Paternal Exposure to Environmental Contaminants and Reproductive Toxicants. Curr Envir Health Rpt 3, 202–213 (2016). https://doi.org/10.1007/s40572-016-0101-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-016-0101-4