Abstract
Background
Demographic shifts cause uncertain changes in the burden of coronary heart disease (CHD) in transitioning regions. We aimed to analyze the trends of CHD burden and its risk factors in Pudong, Shanghai, and explore prevention strategies for transitioning regions.
Methods
We analyzed CHD-related and CHD-specific deaths in Pudong from 2005 to 2020, including the crude mortality rate (CMR), age-standardized mortality rate worldwide (ASMRW), years of life lost (YLL), and age-specific proportions. We also examined the impact of population aging on the burden of CHD. The Joinpoint Regression Program was used to analyze trends, and the decomposition method was used to evaluate the impact of demographics on the mortality rate.
Results
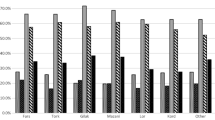
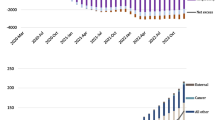
Of the 86,171 CHD-related deaths, 52,152 (60.52%) were CHD-specific deaths. For both CHD-related and CHD-specific deaths, there was a significant increase in the CMR, ASMRW, and YLL rate, except in the 70–79-year age group, which exhibited a distinctive and statistically significant decline in these rates (all P < 0.05). There were steadily increasing trends in the rates caused by aging from 2005 to 2020, with average annual percent changes (AAPCs) of 42.59% and 41.43%, respectively (all P < 0.05).
Conclusions
Our results indicate that the CHD burden in Pudong has been persistently increasing, but in the age group of 70–79 years, substantial declines were observed. The quality of primary healthcare services may be a critical point in addressing the overwhelming CHD burden.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, upon reasonable request.
References
Uncategorized References
Jousilahti P, Laatikainen T, Peltonen M et al (2016) Primary prevention and risk factor reduction in coronary heart disease mortality among working aged men and women in eastern Finland over 40 years: population based observational study. BMJ 352:i721
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222
Mensah GA, Roth GA, Fuster V (2019) The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol 74:2529–2532
The Writing Committee of the report on cardiovascular Health and diseases in China (2021) Report on cardiovascular health and diseases burden in China: an updated summary of 2020. Chin Circ J 36:521–545
Yip W, Fu H, Chen AT et al (2019) 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet 394:1192–1204
Luo Z, He Y, Ma G et al (2020) Years of life lost due to premature death and their trends in people with malignant neoplasm of female genital organs in Shanghai, China during 1995–2018: a population based study. BMC Public Health 20:1489
(2020) Bureau SPNAS: statistical yearbook of Shanghai Pudong New Area (PNA)-2020. China Statistics Press, Beijing
Li Lisheng ZJ, Zhao S (2020) Statistical yearbook of Shanghai Pudong new area (PNA)—2020. China Statistics Press, Beijing
Kim YE, Lee YR, Yoon SJ et al (2019) Years of life lost due to premature death in people with disabilities in Korea: the Korean National Burden of Disease Study Framework. J Korean Med Sci 34:e22
GBD 2015 DALYs and HALE Collaborators (2016) Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1603–1658
Trends and challenges for population and health during population aging—China, 2015–2050. China CDC Weekly 593
Hajar R (2017) Risk factors for coronary artery disease: historical perspectives. Heart Views 18:109–114
Ibsen H, Hilden T (1990) New views on the relationship between coronary heart disease and hypertension. J Intern Med 227:77–79
Sarwar N, Gao P, Seshasai SR et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375:2215–2222
Buddeke J, Bots ML, van Dis I et al (2019) Comorbidity in patients with cardiovascular disease in primary care: a cohort study with routine healthcare data. Br J Gen Pract 69:e398–e406
Roth GA, Mensah GA, Johnson CO et al (2020) Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 76:2982–3021
Ma LY, Chen WW, Gao RL et al (2020) China cardiovascular diseases report 2018: an updated summary. J Geriatr Cardiol 17:1–8
Druetz T (2018) Integrated primary health care in low- and middle-income countries: a double challenge. BMC Med Ethics 19:48
Chen X, Wang Y, Strauss J et al (2021) China health and retirement longitudinal study (CHARLS). In: Gu D, Dupre ME (eds) Encyclopedia of gerontology and population aging. Springer International Publishing, Cham, pp 948–956
Zantinge EM, van den Berg M, Smit HA et al (2014) Retirement and a healthy lifestyle: opportunity or pitfall? A narrative review of the literature. Eur J Public Health 24:433–439
Yan Z, Xiang N, Meng J et al (2022) Understanding the effect of retirement on health behaviors in China: causality, heterogeneity and time-varying effect. Front Public Health 10:952072
Afaya RA, Bam V, Azongo TB et al (2020) Medication adherence and self-care behaviours among patients with type 2 diabetes mellitus in Ghana. PLoS ONE 15:e0237710
Guiding opinions on further promoting the comprehensive reform and development of the municipal community health service. https://www.shanghai.gov.cn/nw49248/20210412/d0ce5c3d164d422ab179e59ccb5576c2.html. Accessed 26 June 2023
Haiqin ZX (2021) Effect of “1+1+1” type of contracted family doctor services in the management of post-PCI patients. Chin Gen Practice 24:80–83
Huang J, Zhang T, Wang L et al (2019) The effect of family doctor-contracted services on noncommunicable disease self-management in Shanghai. China Int J Health Plan Manage 34:935–946
Xiao N, Long Q, Tang X et al (2014) A community-based approach to non-communicable chronic disease management within a context of advancing universal health coverage in China: progress and challenges. BMC Public Health. https://doi.org/10.1186/1471-2458-14-S2-S2
Guidance on the comprehensive promotion of family doctor system in this city. https://www.yicai.com/news/100095345.html. Accessed 26 June 2023
Jia P, Wang Y, Yang M et al (2022) Inequalities of spatial primary healthcare accessibility in China. Soc Sci Med 314:115458
Zou C, Liao XY, Spicer J et al (2020) Ten years’ GP training in China: progress and challenges. Br J Gen Pract 70:511–512
Huang Y, Zhao H, Deng Q et al (2023) Association of neighborhood physical activity facilities with incident cardiovascular disease. Int J Health Geogr 22:16
Glei DA, Landau DA, Goldman N et al (2005) Participating in social activities helps preserve cognitive function: an analysis of a longitudinal, population-based study of the elderly. Int J Epidemiol 34:864–871
Yang Y (2017) The practice and exploration of Shanghai recreational trail system planning. Proc Eng 198:127–138
Lloyd-Jones D, Adams RJ, Brown TM et al (2010) Executive summary: heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation 121:948–954
Lloyd-Jones DM (2010) Cardiovascular risk prediction: basic concepts, current status, and future directions. Circulation 121:1768–1777
Obas V, Vasan RS (2018) The aging heart. Clin Sci (Lond) 132:1367–1382
Eswaran M (1998) One explanation for the demographic transition in developing countries. Oxf Econ Pap 50:237–265
Gaziano TA, Bitton A, Anand S et al (2010) Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol 35:72–115
Acknowledgements
The authors thank all the participants in the vital statistics system of Pudong New Area from 2005 to 2020 for their great work in data collection and assuring high-quality data.
Funding
This study was funded by a grant from the Shanghai Municipal Program for Medical Leading Talents (2019LJ15 to SJ) and the Shanghai Public Health System Construction Three-Year Action Plan Outstanding Youth Talent Training Program (GWV-10.2-YQ43 to YC).
Author information
Authors and Affiliations
Contributions
YX, JZ, ML, and XL drafted and revised the manuscript. XL, YC, RL, QW, and YX participated in the collection, analysis, and interpretation of the data. YX, JZ, WD, ML, XL, and SJ contributed to data collection and suggestions for analysis. XL and SJ conceived the study, participated in its design and coordination and critically revised the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Y., Wang, Q., Zou, J. et al. CHD-related/specific mortality of 3.17 million people in a transitioning region: trends, risk factors, and prevention. Aging Clin Exp Res 35, 3147–3156 (2023). https://doi.org/10.1007/s40520-023-02618-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02618-1