Abstract
Background
The prophylactic effect of exogenous melatonin and melatonin receptor agonists (MMRAs) on postoperative delirium (POD) in elderly patients remains controversial.
Objective
This study aimed to assess the prophylactic effect of MMRAs on POD by conducting a systemic review and meta-analysis of randomized controlled trials (RCTs).
Methods
We systematically searched four electronic databases including PubMed, Web of Science, Cochrane Library, and Embase for the eligible studies up to February 28, 2023. The Cochrane risk of bias tool was used for assessing the risk of bias in the included RCTs. The occurrence of POD was the primary outcome. The quality of evidence was evaluated by Grading of Recommendations Assessment, Development, and Evaluation.
Results
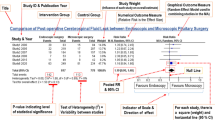
A total of 11 RCTs comprising patients (MMRA group: 777 patients and placebo group: 781 patients) were included. The results of the meta-analysis showed that the MMRA group had a lower occurrence of POD than the placebo group (risk ratio = 0.70, 95% confidence interval: 0.51–0.97, P < 0.05, I2 = 59%). The subgroup analysis showed that melatonin significantly reduced the occurrence of POD (moderate-quality evidence), whereas ramelteon and tryptophan had no significant impact (moderate-quality evidence).
Conclusion
Existing evidence suggested that perioperative use of melatonin can prevent POD in elderly patients.





Similar content being viewed by others
Availability of data and materials
The datasets supporting the conclusions of this article are supplemented along with the article.
References
Numan T, van den Boogaard M, Kamper AM et al (2017) Recognition of delirium in postoperative elderly patients: a multicenter study. J Am Geriatr Soc 65:1932–1938
Schubert M, Schürch R, Boettger S et al (2018) A hospital-wide evaluation of delirium prevalence and outcomes in acute care patients - a cohort study. BMC Health Serv Res 18:550
Iamaroon A, Wongviriyawong T, Sura-Arunsumrit P et al (2020) Incidence of and risk factors for postoperative delirium in older adult patients undergoing noncardiac surgery: a prospective study. BMC Geriatr 20:40
Wang B, Mu C, Tang X et al (2022) The relationship between mild cognitive impairment and postoperative delirium undergoing total knee arthroplasty: the PNDABLE study. Front Aging Neurosci 14:959510
Steenblock J, Braisch U, Brefka S et al (2023) Frailty index and its association with the onset of postoperative delirium in older adults undergoing elective surgery. BMC Geriatr 23:90
Wang LH, Jin TT, Zhang XW et al (2021) Risk factors and prevention for postoperative delirium after orthopedic surgery. Indian J Psychiatry 63:554–559
Bramley P, McArthur K, Blayney A et al (2021) Risk factors for postoperative delirium: an umbrella review of systematic reviews. Int J Surg (London, England) 93:106063
Yang Q, Wang J, Huang X et al (2020) Incidence and risk factors associated with postoperative delirium following primary elective total hip arthroplasty: a retrospective nationwide inpatient sample database study. BMC Psychiatry 20:343
Robinson TN, Eiseman B (2008) Postoperative delirium in the elderly: diagnosis and management. Clin Interv Aging 3:351–355
Shen QH, Li HF, Zhou XY et al (2020) Relation of serum melatonin levels to postoperative delirium in older patients undergoing major abdominal surgery. J Int Med Res 48:300060520910642
Oh ES, Fong TG, Hshieh TT et al (2017) Delirium in older persons: advances in diagnosis and treatment. JAMA 318:1161–1174
Song Y, Liu Y, Yuan Y et al (2021) Effects of general versus subarachnoid anaesthesia on circadian melatonin rhythm and postoperative delirium in elderly patients undergoing hip fracture surgery: a prospective cohort clinical trial. EBioMedicine 70:103490
Shigeta H, Yasui A, Nimura Y et al (2001) Postoperative delirium and melatonin levels in elderly patients. Am J Surg 182:449–454
Tordjman S, Chokron S, Delorme R et al (2017) Melatonin: pharmacology, functions and therapeutic benefits. Curr Neuropharmacol 15:434–443
de Rooij SE, van Munster BC (2013) Melatonin deficiency hypothesis in delirium: a synthesis of current evidence. Rejuvenation Res 16:273–278
Lin L, Huang QX, Yang SS et al (2013) Melatonin in Alzheimer’s disease. Int J Mol Sci 14:14575–14593
Han Y, Wu J, Qin Z et al (2020) Melatonin and its analogues for the prevention of postoperative delirium: a systematic review and meta-analysis. J Pineal Res 68:e12644
Wang CM, Zhou LY (2022) Melatonin and melatonergic agents for the prevention of postoperative delirium: a meta-analysis of randomized placebo-controlled trials. Asian J Surg 45:27–32
Honda S, Furukawa K, Makuuchi R et al (2020) A phase II study of ramelteon for the prevention of postoperative delirium in elderly patients undergoing gastrectomy. Surg Today 50:1681–1686
Tanifuji T, Otsuka I, Okazaki S et al (2022) Preventive effects of preoperative ramelteon on postoperative delirium in Asian elderly population: a randomized, double-blind, placebo-controlled trial, and a systematic review and meta-analysis. Asian J Psychiatr 78:103282
Mohamed SA, Rady A, Youssry M et al (2022) Performance of melatonin as prophylaxis in geriatric patients with multifactorial risk for postoperative delirium development: a randomized comparative study. Turkish J Anaesthesiol Reanim 50:178–186
Fazel MR, Mofidian S, Mahdian M et al (2022) The effect of melatonin on prevention of postoperative delirium after lower limb fracture surgery in elderly patients: a randomized double blind clinical trial. Int J Burns Trauma 12:161–167
Esmaeili A, Fanoodi A, Ebrahimi A et al (2022) The efficacy of melatonin and clonidine in preventing emergence delirium in the elderly undergoing orthopedic surgery, neurosurgery, and general surgery: a placebo-controlled randomized clinical trial. J Kermanshah Univ Med Sci. https://doi.org/10.5812/jkums-128831
Zadeh FJ, Janatmakan F, Shafaeebejestan E et al (2021) Effect of melatonin on delirium after on-pump coronary artery bypass graft surgery: a randomized clinical trial. Iran J Med Sci 46:120–127
Shi Y (2021) Effects of melatonin on postoperative delirium after PCI in elderly patients: a randomized, single-center, double-blind, placebo-controlled trial. Heart Surg Forum 24:E893–E897
Lange PW, Clayton-Chubb DI, Watson R et al (2021) Results from a double blinded, randomised, placebo-controlled, feasibility trial of melatonin for the treatment of delirium in older medical inpatients. Intern Med J 51:33–41
Jaiswal SJ, Kang DY, Wineinger NE et al (2021) Objectively measured sleep fragmentation is associated with incident delirium in older hospitalized patients: analysis of data collected from an randomized controlled trial. J Sleep Res 30:e13205
Hollinger A, von Felten S, Sutter R et al (2020) Study protocol for a prospective randomised double-blind placebo-controlled clinical trial investigating a Better Outcome with Melatonin compared to Placebo Administered to normalize sleep-wake cycle and treat hypoactive ICU Delirium: the Basel BOMP-AID study. BMJ Open 10:e034873
Gandolfi JV, Di Bernardo APA, Chanes DAV et al (2020) The effects of melatonin supplementation on sleep quality and assessment of the serum melatonin in ICU patients: a randomized controlled trial. Crit Care Med 48:E1286–E1293
Barnes J, Sewart E, Armstrong R et al (2022) Melatonin for the prevention of postoperative delirium in older adults. Anaesthesia 77:7
Oh ES, Leoutsakos JM, Rosenberg PB et al (2021) Effects of Ramelteon on the prevention of postoperative delirium in older patients undergoing orthopedic surgery: the RECOVER randomized controlled trial. Am J Geriatr Psychiatry 29:90–100
Mahrose R, ElSerwi H, Maurice A et al (2021) Postoperative delirium after coronary artery bypass graft surgery: dexmedetomidine infusion alone or with the addition of oral melatonin. Egypt J Anaesth 37:62–68
Ford AH, Flicker L, Kelly R et al (2020) The healthy heart-mind trial: randomized controlled trial of melatonin for prevention of delirium. J Am Geriatr Soc 68:112–119
Gupta PK, Verma R, Kohli M et al (2019) The effect of Ramelteon on postoperative delirium in elderly patients: a randomised double-blind study. J Clin Diagn Res. https://doi.org/10.7860/JCDR/2019/42635.13384
Robinson TN, Dunn CL, Adams JC et al (2014) Tryptophan supplementation and postoperative delirium–a randomized controlled trial. J Am Geriatr Soc 62:1764–1771
de Jonghe A, van Munster BC, Goslings JC et al (2014) Effect of melatonin on incidence of delirium among patients with hip fracture: a multicentre, double-blind randomized controlled trial. CMAJ 186:E547–E556
Sultan SS (2010) Assessment of role of perioperative melatonin in prevention and treatment of postoperative delirium after hip arthroplasty under spinal anesthesia in the elderly. Saudi J Anaesth 4:169–173
Khaing K, Nair BR (2021) Melatonin for delirium prevention in hospitalized patients: a systematic review and meta-analysis. J Psychiatr Res 133:181–190
Yamaguchi Y, Mihara T, Taguri M et al (2014) Melatonin receptor agonist for the prevention of postoperative delirium in elderly patients: a randomized, double-blind, Placebo-Controlled Trial. Intensive Care Med 40:S246
Yu CL, Carvalho AF, Thompson T et al (2023) Ramelteon for delirium prevention in hospitalized patients: an updated meta-analysis and trial sequential analysis of randomized controlled trials. J Pineal Res 74:e12857
Mohamed SA, Rady A, Youssry M et al (2022) Performance of melatonin as prophylaxis in geriatric patients with multifactorial risk for postoperative delirium development: a randomized comparative study. Turkish J Anaesthesiol Reanim 50:178–186
Yin XL, Li JC, Xue R et al (2022) Melatonin pretreatment prevents propofol-induced sleep disturbance by modulating circadian rhythm in rats. Exp Neurol 354:114086
Stepnowsky CJ, Ancoli-Israel S (2008) Sleep and its disorders in seniors. Sleep Med Clin 3:281–293
Yang R, Xu XX, Liu H et al (2022) The impact of morning surgery or afternoon surgery on postoperative sleep quality and melatonin levels of elderly patients: a prospective, randomized study. Nat Sci Sleep 14:1677–1686
Taylor J, Parker M, Casey CP et al (2022) Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: a prospective cohort study. Br J Anaesth 129:219–230
Xie Z, Swain CA, Ward SA et al (2014) Preoperative cerebrospinal fluid β-Amyloid/Tau ratio and postoperative delirium. Ann Clin Transl Neurol 1:319–328
Rehman SU, Ikram M, Ullah N et al (2019) Neurological enhancement effects of melatonin against brain injury-induced oxidative stress, neuroinflammation, and neurodegeneration via AMPK/CREB signaling. Cells 8:760
Vincent B (2018) Protective roles of melatonin against the amyloid-dependent development of Alzheimer’s disease: a critical review. Pharmacol Res 134:223–237
Mahanna-Gabrielli E, Miano TA, Augoustides JG et al (2018) Does the melatonin receptor 1B gene polymorphism have a role in postoperative delirium? PLoS ONE 13:e0207941
Lalanne S, Fougerou-Leurent C, Anderson GM et al (2021) Melatonin: from pharmacokinetics to clinical use in autism spectrum disorder. Int J Mol Sci 22:1490
Mistraletti G, Sabbatini G, Taverna M et al (2010) Pharmacokinetics of orally administered melatonin in critically ill patients. J Pineal Res 48:142–147
Acknowledgements
The authors thank Bullet Edits Limited for their assistance in English language editing and proofreading of the manuscript.
Funding
This research was supported by the Zhejiang Provincial Traditional Chinese Medical. Innovation Team of China under Grant No. 2022-19 and Project of Jiaxing Science and Technology Bureau (2021AY30021).
Author information
Authors and Affiliations
Contributions
LJ assisted in conceptualization, methodology, and writing—original draft; LL was involved in project administration, resources, and supervision; YC and KL performed formal analysis, investigation, and validation; QS contributed to project administration.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have agreed to publish this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, Ls., lai, L., Chen, Yj. et al. Prophylactic effect of exogenous melatonin and melatonin receptor agonists on postoperative delirium in elderly patients: a systemic review and meta-analysis of randomized controlled trials. Aging Clin Exp Res 35, 2323–2331 (2023). https://doi.org/10.1007/s40520-023-02564-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02564-y