Abstract
Background
Frailty associates with increased vulnerability to adverse health outcomes and reduced tolerance to medical interventions. Its impact on patients with chronic respiratory diseases, particularly beyond chronic obstructive pulmonary disease (COPD), remains poorly understood.
Aims
To evaluate the association between frailty index and 5-year mortality across different “spirometric” patterns and the variation in their occurring frailty determinants.
Methods
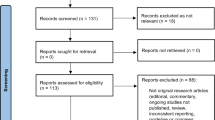
This study analyzed data from the SARA study, which enrolled 1968 older adults, to evaluate the association between frailty and 5-year mortality across different spirometric patterns. Frailty was assessed using the frailty index (FI), and spirometry was performed to determine lung function patterns. Hazard ratios (HRs) were calculated using Cox regression models, adjusting for age and sex.
Results
Among the study participants, 16% were classified as frail. Frailty was associated with a significantly increased risk of mortality across all spirometric patterns. The 5-year mortality rates were 34.3% in subjects with normal spirometry, 45.1% in those with obstructive defects, 55% in those with restrictive defects, and 42.6% in those with mixed airflow defects. The unadjusted HRs for mortality were 2.64 (95% CI 2.10–3.32) for the overall cohort, 2.24 (95% CI 1.48–3.40) for obstructive defects, 2.45 (95% CI 1.12–5.36) for restrictive defects, and 2.79 (95% CI 1.41–3.17) for mixed airflow defects. After adjusting for age and sex, the HRs remained statistically significant: 2.25 (95% CI 1.37–2.84) for the overall cohort, 2.08 (95% CI 1.37–3.18) for obstructive defects, 2.27 (95% CI 1.04–1.17) for restrictive defects, and 2.21 (95% CI 1.20–3.08) for mixed airflow defects.
Conclusion
Frailty is a common syndrome and is associated with a significantly increased risk of mortality. The FI provides valuable information for risk profiling and personalized interventions beyond age and lung function parameters. Including frailty assessment in clinical evaluations can aid in resource allocation and improve patient care in respiratory diseases.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, [SS]. The data are not publicly available due to italian law restrictions, since their containing information could compromise the privacy of research participants.
References
Clegg A, Young J, Iliffe S et al (2013) Frailty in elderly people. Lancet 381:752–762. https://doi.org/10.1016/S0140-6736(12)62167-9
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence of a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156. https://doi.org/10.1093/gerona/56.3.M146
Singer JP, Diamond JM, Gries CJ et al (2015) Frailty phenotypes disability, and outcomes in adult candidates for lung trasplantation. Am J Respir Crit Care Med 192:1325–1334. https://doi.org/10.1164/rccm.201506-1150OC
Dent E, Martin FC, Bergman H et al (2019) Management of frailty: opportunities, challenges, and future directions. Lancet 394:1376–1386. https://doi.org/10.1016/S0140-6736(19)31785-4
Turner G, Clegg A (2014) Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing 43:744–747. https://doi.org/10.1093/ageing/afu138
Clegg A, Bates C, Young J et al (2016) Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 45:353–360. https://doi.org/10.1093/ageing/afw039
Afilalo J, Karunananthan S, Eisenberg MK et al (2009) Role of frailty in patients with cardiovascular disease. Am J Cardiol 103:1616–1621. https://doi.org/10.1016/j.amjcard.2009.01.375
Canevelli M, Cesari M, Remiddi F et al (2017) Promoting the assessment of frailty in the clinical approach to cognitive disorders. Front Aging Neurosci 9:36. https://doi.org/10.3389/fnagi.2017.00036
Abete P, Basile C, Bulli G et al (2017) The Italian version of the “frailty index” based on deficits in health: a validation study. Aging Clin Exp Res 29:913–926. https://doi.org/10.1007/s40520-017-0793-9
Luo J, Zhang D, Tang W et al (2021) Impact on frailty on the risk of exacerbation and all-cause mortality in elderly patients with stable chronic obstructive pulmonary disease. Clin Interv Aging 16:593–601. https://doi.org/10.2147/CIA.S303852
Blanc PD, Annesi-Maesano I, Balmes JR et al (2019) The occupational burden of nonmalignant respiratory diseases. An Official American Thoracic Society and European Respiratory Society Statement. Am J Respir Crit Care Med 199:1312–1334. https://doi.org/10.1164/rccm.201904-0717ST
Vaz Fragoso CA, Enright PL, McAvay G et al (2012) Frailty and respiratory impairment in older persons. Am J Med 125:79–86. https://doi.org/10.1016/j.amjmed.2011.06.024
Kennedy CC, Novotny PJ, LeBrasseur NK et al (2019) Frailty and clinical outcomes in chronic obstructive pulmonary disease. Ann Am Thorac Soc 16:217–224. https://doi.org/10.1513/AnnalsATS.201803-175OC
Maddocks M, Kon SSC, Canavan JL et al (2016) Physical frailty and pulmonary rehabilitation in COPD: a prospective cohort study. Thorax 71:988–995. https://doi.org/10.1136/thoraxjnl-2016-208460
Kyung Park S, Richardson CR, Holleman RG et al (2013) Frailty in people with COPD, using the National Health and Nutrition Evaluation Survey Dataset (2003–2006). Heart Lung 42:163–170. https://doi.org/10.1016/j.hrtlng.2012.07.004
Lahousse L, Ziere G, Verlinden JA et al (2016) Risk of frailty in elderly with COPD: a population-based study. J Gerontol A Biol Sci Med Sci 71:689–695. https://doi.org/10.1093/gerona/glv154
Galizia G, Cacciatore F, Testa G et al (2011) Role of clinical frailty on long-term mortality of elderly subjects with and without chronic obstructive pulmonary disease. Aging Clin Exp Res 23:118–125. https://doi.org/10.1007/BF03351076
Mannino DM, Ford ES, Redd SC (2003) Obstructive and restrictive lung disease and functional limitation: data from the Third National Health and Nutrition Examination. J Intern Med 254:540–547. https://doi.org/10.1111/j.1365-2796.2003.01211.x
Scarlata S, Pedone C, Fimognari FL et al (2008) Restrictive pulmonary dysfunction at spirometry and mortality in the elderly. Respir Med 102:1349–1354. https://doi.org/10.1016/j.rmed.2008.02.021
Bellia V, Pistelli R, Catalano F et al (2000) Quality control of spirometry in the elderly, The SA.R.A. study. salute respiration nell’Anziano = respiratory health in the elderly. Am J Respir Crit Care Med 161:1094–1100. https://doi.org/10.1164/ajrccm.161.4.9810093
Graham BL, Steenbruggen I, Miller MR et al (2019) Standardization of spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med 200:e70–e88. https://doi.org/10.1164/rccm.201908-1590ST
Quanjer PH, Stanojevic S, Cole TJ et al (2012) ERS global lung function initiative. multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40:1324–1343. https://doi.org/10.1183/09031936.00080312
Scarlata S, Pedone C, Conte ME et al (2009) Accuracy of spirometry in diagnosing pulmonary restriction in elderly people. J Am Geriatr Soc 57:2107–2111. https://doi.org/10.1111/j.1532-5415.2009.02525.x
Pedone C, Scarlata S, Chiurco D et al (2012) Association of reduced total lung capacity with mortality and use of health services. Chest 141:1025–1030. https://doi.org/10.1378/chest.11-0899
Mannino DM (2022) Restricted spirometry through the lifespan. Lancet Respir Med 10:2–3. https://doi.org/10.1016/S2213-2600(21)00507-5
Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 1:323–336. https://doi.org/10.1100/tsw.2001.58
Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173:489–495. https://doi.org/10.1503/cmaj.050051
Rockwood K, Mitnitski A (2007) Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 62:722–727. https://doi.org/10.1093/gerona/62.7.722
Searle S, Mitnitski A, Gahbauer E et al (2008) A standard procedure for creating a frailty index. BMC Geriatr 8:24. https://doi.org/10.1186/1471-2318-8-24
Dent E, Kowal P, Hoogendijk EO et al (2016) Frailty measurement in research and clinical practice: A review. Eur J Intern Med 31:3–10. https://doi.org/10.1016/j.ejim.2016.03.007
Scarlata S, Finamore P, Laudisio A et al (2021) Association between frailty index, lung function, and major clinical determinants in chronic obstructive pulmonary disease. Aging Clin Exp Res 33:2165–2173. https://doi.org/10.1007/s40520-021-01878-z
Gale NS, Albarrati AM, Munnery MM et al (2018) Frailty: A global measure of the multisystem impact of COPD. Chron Respir Dis 15:347–355. https://doi.org/10.1177/1479972317752763
Aliberti MJR, Szlejf C, Avelino-Silva VI et al (2021) COVID-19 is not over and age is not enough: Using frailty for prognostication in hospitalized patients. J Am Geriatr Soc 69:1116–1127. https://doi.org/10.1111/jgs.17146
Cesari M, Costa N, Hoogendijk EO et al (2016) How the frailty index may support the allocation of health care resources: an example from the INCUR Study. J Am Med Dir Assoc 17:448–450. https://doi.org/10.1016/j.jamda.2016.02.007
Basile G, Catalano A, Mandraffino G et al (2019) Frailty modifications and prognostic impact in older patients admitted in acute care. Aging Clin Exp Res 31:151–155. https://doi.org/10.1007/s40520-018-0989-7
Kelaiditi E, Andrieu S, Cantet C et al (2016) Frailty Index and Incident Mortality, Hospitalization, and Institutionalization in Alzheimer’s Disease: Data From the ICTUS Study. J Gerontol A Biol Sci Med Sci 71:543–548. https://doi.org/10.1093/gerona/glv137
Balducci L, Colloca G, Cesari M et al (2010) Assessment and treatment of elderly patients with cancer. Surg Oncol 19:117–123. https://doi.org/10.1016/j.suronc.2009.11.008
Drummond MB, Wise RA, John M et al (2010) Accuracy of death certificates in COPD: analysis from the TORCH trial. COPD 7:179–185. https://doi.org/10.3109/15412555.2010.481695
GBD Chronic Respiratory Disease Collaborators (2020) Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med 8:585–596. https://doi.org/10.1016/S2213-2600(20)30105-3
Acknowledgements
Not applicable.
Funding
This study was not founded.
Author information
Authors and Affiliations
Contributions
SS: conceptualization, methodology, data analysis, writing and editing original draft preparation. SZ: writing—original draft preparation. PF: writing—original draft preparation, CRO: writing—reviewing and editing, supervision. NS: development or design of methodology, provision of study materials. RAI: provision of study materials, supervision. CP: provision of study materials, supervision. MC: writing—reviewing and editing, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no affiliations with or involvement in any organization or entity with any financial or nonfinancial interest related to this manuscript. They also deny any perceived or real conflict of interest related with the publication of the present scientific work.
Ethical approval and consent to participate
The study protocol has been complied in accordance the tenets of the Helsinki Declaration and has been approved by the Coordinating Centre Ethical Committee at the University of Palermo (Protocol Code: 3/276). A written informed consent was signed for inclusion prior to the start of the study from all subjects.
Statement of human and animal rights
The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Scarlata, S., Zotti, S., Finamore, P. et al. Frailty in the chronic respiratory patient: association with mortality and clinical features in obstructive, restrictive, and mixed spirometric patterns. Aging Clin Exp Res 35, 2573–2581 (2023). https://doi.org/10.1007/s40520-023-02535-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02535-3