Abstract
Objective
Probable sarcopenia is a predictor of functional limitation in older adults. However, whether standard thresholds recommended by guides, or population-specific thresholds better predict impairment in functionality is an issue that needs to be enlightened. We aimed to study the associations of probable sarcopenia identified by the use of EWGSOP2 and population-specific thresholds with deterioration in functionality at follow-up and give prevalences of probable sarcopenia with different thresholds in older outpatients admitted to a tertiary health center.
Methods
In this retrospective, longitudinal follow-up study, we assessed handgrip strength (HGS) at the admission with a Jamar hand-dynamometer and diagnosed probable sarcopenia with standard and population-specific thresholds, i.e., 27 kg/16 kg, and 35 kg/20 kg in males/females, respectively. We evaluated activities of daily living (ADL) and instrumental ADL (IADL), with Katz and Lawton scales, at the admission and follow-up. To study whether probable sarcopenia was a predictor of impaired functionality, we defined two models for Cox regression analysis. We performed adjustments for age, sex, and nutritional status (assessed by Mini-Nutritional Assessment-Short Form) in Model 1 and defined Model 2 by adding low gait speed and frailty to the variables in Model 1.
Results
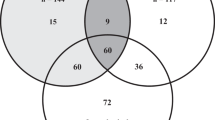
Among a total of 1970 patients, 195 had follow-up of median 560 days. The mean age was 75.5 ± 5.5, and 142 (72.8%) were female. In the basal evaluation, the prevalences of probable sarcopenia defined by the standard cut-offs and by population-specific cut-offs were 8.7% and 35.4%, respectively. In univariate analyses (Kaplan–Meier log-rank test), probable sarcopenia by population-specific cut-offs, but not EWGSOP2-cut-offs, was associated with deteriorations in both ADL (p = 0.04) and IADL (p < 0.001). In multivariate analyses, only the probable sarcopenia identified by population-specific cut-offs was independently associated with impairment in IADL in both models [HR (95%CI) = 1.88 (1.07–3.30), and 1.9 (1.04–3.6); for Model 1 and Model 2, respectively)].
Conclusion
Our findings suggested that the definition of probable sarcopenia identified by not standard, but population-specific thresholds more reliably predicted longitudinal deterioration of functionality in older outpatients. This finding might be considered as evidence supporting the use of population-specific cut-offs when the concern is sarcopenia diagnosis.



Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Angulo J, El Assar M, Rodríguez-Mañas L (2016) Frailty and sarcopenia as the basis for the phenotypic manifestation of chronic diseases in older adults. Mol Aspects Med 50:1–32
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Beaudart C, Zaaria M, Pasleau F et al (2017) Health outcomes of sarcopenia: a systematic review and meta-analysis. PLoS One 12:e0169548
Rosenberg IH (1989) Summary comments. Am J Clin Nutr 50:1231–1233
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) European working group on sarcopenia in older people. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–23
Muscaritoli M, Anker SD, Argilés J et al (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics.” Clin Nutr 29:154–159
Fielding RA, Vellas B, Evans WJ et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12:249–256
Morley JE, Abbatecola AM, Argiles JM et al (2011) Society on sarcopenia, cachexia and wasting disorders trialist workshop. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc 12:403–409
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558
Goodpaster BH, Park SW, Harris TB et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol Ser A 61:1059–1064
Woo J, Leung J, Morley JE (2015) Defining sarcopenia in terms of incident adverse outcomes. J Am Med Dir Assoc 16:247–252
da Silva Alexandre T, de Oliveira Duarte YA, Ferreira Santos JL et al (2014) Sarcopenia according to the european working group on sarcopenia in older people (EWGSOP) versus Dynapenia as a risk factor for disability in the elderly. J Nutr Health Aging 18:547–553
Bianchi L, Ferrucci L, Cherubini A et al (2016) The predictive value of the EWGSOP definition of sarcopenia: results from the InCHIANTI study. J Gerontol A Biol Sci Med Sci 71:259–264
Wennie Huang WN, Perera S, VanSwearingen J et al (2010) Performance measures predict onset of activity of daily living difficulty in community-dwelling older adults. J Am Geriatr Soc 58:844–852
Duchowny KA, Clarke PJ, Peterson MD (2018) Muscle weakness and physical disability in older Americans: longitudinal findings from the U.S. health and retirement study. J Nutr Health Aging 22:501–507
Morley JE, Malmstrom TK, Miller DK (2012) A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging 16:601–608
Rubenstein LZ, Harker JO, Salvà A et al (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56:M366–M372
Mearin F, Lacy BE, Chang L et al (2016) Bowel disorders [published online ahead of print, 2016 Feb 18]. Gastroenterology S0016-5085
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 31:721–727
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Grimmer K, Beaton K, Hendry K (2013) Identifying functional decline: a methodological challenge. Patient Relat Outcome Meas 4:37–48
Stenhagen M, Ekström H, Nordell E et al (2014) Both deterioration and improvement in activities of daily living are related to falls: a 6-year follow-up of the general elderly population study Good Aging in Skåne. Clin Interv Aging 9:1839–1846
Sager MA, Franke T, Inouye SK et al (1996) Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 156:645–652
Roberts HC, Denison HJ, Martin HJ et al (2011) A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 40:423–429
Dodds RM, Syddall HE, Cooper R et al (2014) Grip strength across the life course: normative data from twelve British studies. PLoS ONE 9:e113637
Bahat G, Aydin CO, Tufan A et al (2021) Muscle strength cutoff values calculated from the young reference population to evaluate sarcopenia in Turkish population. Aging Clin Exp Res 33:2879–2882
Feger DM, Willis SL, Thomas KR et al (2020) Incident instrumental activities of daily living difficulty in older adults: which comes first? Findings from the advanced cognitive training for independent and vital elderly study. Front Neurol 11:550577
Amigues I, Schott AM, Amine M et al (2013) Low skeletal muscle mass and risk of functional decline in elderly community-dwelling women: the prospective EPIDOS study. J Am Med Dir Assoc 14:352–357
Seidel D, Brayne C, Jagger C (2011) Limitations in physical functioning among older people as a predictor of subsequent disability in instrumental activities of daily living. Age Ageing 40:463–469
Legrand D, Vaes B, Matheï C et al (2014) Muscle strength and physical performance as predictors of mortality, hospitalization, and disability in the oldest old. J Am Geriatr Soc 62:1030–1038
Chaudhry SI, McAvay G, Ning Y et al (2010) Geriatric impairments and disability: the cardiovascular health study. J Am Geriatr Soc 58:1686–1692
Harris-Love MO, Benson K, Leasure E et al (2018) The influence of upper and lower extremity strength on performance-based sarcopenia assessment tests. J Funct Morphol Kinesiol 3:53
Reid KF, Fielding RA (2012) Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev 40:4–12
Purcell SA, MacKenzie M, Barbosa-Silva TG et al (2020) Sarcopenia prevalence using different definitions in older community-dwelling canadians. J Nutr Health Aging 24:783–790
Kim H, Hirano H, Edahiro A et al (2016) Sarcopenia: prevalence and associated factors based on different suggested definitions in community-dwelling older adults. Geriatr Gerontol Int 16:110–122
Bahat G, Tufan A, Kilic C et al (2020) Prevalence of sarcopenia and its components in community-dwelling outpatient older adults and their relation with functionality. Aging Male 23:424–430
Mayhew AJ, Amog K, Phillips S et al (2018) The prevalence of sarcopenia in community-dwelling older adults, an exploration of differences between studies and within definitions: a systematic review and meta-analyses. Age Ageing 48:48–56
Shafiee G, Keshtkar A, Soltani A et al (2017) Prevalence of sarcopenia in the world: a systematic review and meta-analysis of general population studies. J Diabetes Metab Disord 16:21
Bahat G, Tufan A, Tufan F et al (2016) Cut-off points to identify sarcopenia according to European Working Group on Sarcopenia in Older People (EWGSOP) definition. Clin Nutr 35:1557–1563
Bahat G, Tufan A, Kilic C et al (2019) Cut-off points for weight and body mass index adjusted bioimpedance analysis measurements of muscle mass. Aging Clin Exp Res 31:935–942
Pasco JA, Holloway-Kew KL, Tembo M et al (2019) Normative data for lean mass using FNIH criteria in an australian setting. Calcif Tissue Int 104:475–479
Savas S, Taşkıran E, Sarac FZ et al (2020) A cross-sectional study on sarcopenia using EWGSOP1 and EWGSOP2 criteria with regional thresholds and different adjustments in a specific geriatric outpatient clinic. Eur Geriatr Med 11:239–246
Boshnjaku A, Bahtiri A, Feka K et al (2022) Impact of using population-specific cut-points, self-reported health, and socio-economic parameters to predict sarcopenia: a cross-sectional study in community-dwelling kosovans aged 60 years and older. J Clin Med 11:5579
Acknowledgements
We would like to warmly thank Meryem Merve Oren for her contributions to the statistical analysis of this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization and data curation were contributed by GB and MEB. Formal analysis, investigation, and methodology were contributed by GB, CK, SO, and MEB. Project administration, resources, software, supervision, validation, visualization, writing—original draft, and writing—review and editing, were contributed by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. The data were previously presented orally at the annual meeting of the World Congress on Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases on March 24–27, 2022.
Ethical approval
Ethical approval for the study was granted by the local ethics committee (reference: 1586/2020).
Human and animal rights statement
The study design and all procedures involving human participants were in accordance with the ethical standards of the institutional research committee as well as the 1964 Helsinki Declaration and its subsequent amendments.
Consent to participate
Written informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bahat, G., Bozkurt, M.E., Ozkok, S. et al. The longitudinal associations of sarcopenia definitions with functional deterioration: a comparative study. Aging Clin Exp Res 35, 2089–2099 (2023). https://doi.org/10.1007/s40520-023-02498-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02498-5