Abstract
Background
Postoperative pulmonary complications (PPCs) seriously affect the postoperative prognosis of elderly patients underwent hip fracture surgery. Although methylprednisolone is increasingly used, the association between perioperative methylprednisolone and PPCs is still controversial. The study aims to determine whether perioperative administration of methylprednisolone is associated with PPCs in elderly patients during hip fracture surgery.
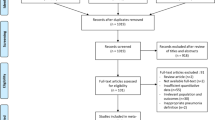
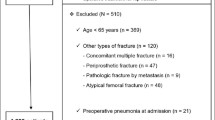
Patients and Methods
In this retrospective cohort study, records of 584 patients (≥ 65 years) who underwent hip fracture surgery between January 2013 and October 2020 were extracted. Univariate and multivariate regression analysis were performed to identify the risk factors for PPCs. To further explore the association between administration of methylprednisolone and PPCs, 53 patients received methylprednisolone and 53 patients without methylprednisolone were matched for the confounding factors using propensity score matching (PSM) analysis. The odds ratios (OR) and 95% confidence intervals (CI) for the above variables were analyzed.
Results
The incidence of PPCs during postoperative hospitalization was 6.83% (38/556) among the elderly patients following hip fracture surgery. Patients with PPCs had higher postoperative mortality rate, longer hospital stay, more hospitalization cost, and higher incidence of cardiac arrest (all P < 0.05). Multivariate logistic regression analysis showed that age, hypertension, hypoglycemia, hypoproteinemia and perioperative methylprednisolone were independent risk factors for PPCs. Moreover, administration of methylprednisolone was significantly correlated with PPCs both before PSM adjustment (OR = 3.25; 95% CI, 1.67 to 6.33; P = 0.001) and after PSM adjustment (OR = 6.68; 95% CI, 1.40 to 31.82; P = 0.017).
Conclusion
Perioperative administration of methylprednisolone is a risk factor for PPCs in elderly patients undergoing hip fracture surgery.

Similar content being viewed by others
References
Peeters CM, Visser E, Van de Ree CL et al (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury 47:1369–1382. https://doi.org/10.1016/j.injury.2016.04.018
Chang SC, Lai JI, Lu MC et al (2018) Reduction in the incidence of pneumonia in elderly patients after hip fracture surgery: an inpatient pulmonary rehabilitation program. Medicine (Baltimore) 97:e11845. https://doi.org/10.1097/MD.0000000000011845
Shin KH, Kim JJ, Son SW et al (2020) Early postoperative hypoalbuminaemia as a risk factor for postoperative pneumonia following hip fracture surgery. Clin Interv Aging 15:1907–1915. https://doi.org/10.2147/CIA.S272610
Brown CA, Boling J, Manson M et al (2012) Relation between prefracture characteristics and perioperative complications in the elderly adult patient with hip fracture. South Med J 105:306–310. https://doi.org/10.1097/SMJ.0b013e3182574bfd
Roche JJ, Wenn RT, Sahota O et al (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 331:1374. https://doi.org/10.1136/bmj.38643.663843.55
Fernandez-Bustamante A, Frendl G, Sprung J et al (2017) Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the perioperative research network investigators. JAMA Surg 152:157–166. https://doi.org/10.1001/jamasurg.2016.4065
Bohl DD, Sershon RA, Fillingham YA et al (2016) Incidence, risk factors, and sources of sepsis following total joint arthroplasty. J Arthroplast 31:2875–2879 e2872. https://doi.org/10.1016/j.arth.2016.05.031
Hu F, Jiang C, Shen J et al (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 43:676–685. https://doi.org/10.1016/j.injury.2011.05.017
Sabate S, Mazo V, Canet J (2014) Predicting postoperative pulmonary complications: implications for outcomes and costs. Curr Opin Anaesthesiol 27:201–209. https://doi.org/10.1097/ACO.0000000000000045
Gao Q, Mok HP, Wang WP et al (2014) Effect of perioperative glucocorticoid administration on postoperative complications following esophagectomy: a meta-analysis. Oncol Lett 7:349–356. https://doi.org/10.3892/ol.2013.1748
Skroubis G, Theofanis G, Spyropoulos C et al (2016) Preoperative high dose of methylprednisolone improves early postoperative pulmonary function, in super-obese patients undergoing open surgery; a prospective. Comparative Study J Gastrointest Surg 20:1959–1965. https://doi.org/10.1007/s11605-016-3281-1
Weijs TJ, Dieleman JM, Ruurda JP et al (2014) The effect of perioperative administration of glucocorticoids on pulmonary complications after transthoracic oesophagectomy: a systematic review and meta-analysis. Eur J Anaesthesiol 31:685–694. https://doi.org/10.1097/EJA.0000000000000093
Sato N, Koeda K, Ikeda K et al (2002) Randomized study of the benefits of preoperative corticosteroid administration on the postoperative morbidity and cytokine response in patients undergoing surgery for esophageal cancer. Ann Surg 236:184–190. https://doi.org/10.1097/00000658-200208000-00006
Yuan Z, Fu S, Mi L (2020) Risk factors of postoperative pulmonary infection in elderly patients with hip fracture (In Chinese). Chin J Bone Joint Injury 35. https://doi.org/10.7531/j.issn.1672-9935.2020.02.018
Bohl DD, Sershon RA, Saltzman BM et al (2018) Incidence, risk factors, and clinical implications of pneumonia after surgery for geriatric hip fracture. J Arthroplast. 33:e1551. https://doi.org/10.1016/j.arth.2017.11.068
Bohl DD, Saltzman BM, Sershon RA et al (2017) Incidence, risk factors, and clinical implications of pneumonia following total hip and knee arthroplasty. J Arthroplast. 32:1991–1995. https://doi.org/10.1016/j.arth.2017.01.004
Chen C, Chen X, Chen J et al (2022) Association between preoperative hs-crp/albumin ratio and postoperative sirs in elderly patients: a retrospective observational cohort study. J Nutr Health Aging 26:352–359. https://doi.org/10.1007/s12603-022-1761-4
Li X, Chen C, Wei X et al (2018) Retrospective comparative study on postoperative pulmonary complications after orthotopic liver transplantation using the Melbourne Group Scale (MGS-2) Diagnostic Criteria. Ann Transplant 23:377–386. https://doi.org/10.12659/AOT.907883
Gallart L, Canet J (2015) Post-operative pulmonary complications: understanding definitions and risk assessment. Best Pract Res Clin Anaesthesiol 29:315–330. https://doi.org/10.1016/j.bpa.2015.10.004
Odor PM, Bampoe S, Gilhooly D et al (2020) Perioperative interventions for prevention of postoperative pulmonary complications: systematic review and meta-analysis. BMJ 368:m540. https://doi.org/10.1136/bmj.m540
Xiang G, Dong X, Xu T et al (2020) A Nomogram for prediction of postoperative pneumonia risk in elderly hip fracture patients. Risk Manag Healthc Policy 13:1603–1611. https://doi.org/10.2147/RMHP.S270326
de Miguel AM, Roca Chacon O, Martinez-Alonso M et al (2018) Hip fracture in the elderly patient: prognostic factors for mortality and functional recovery at one year. Rev Esp Geriatr Gerontol 53:247–254. https://doi.org/10.1016/j.regg.2018.04.447
Zhao K, Zhang J, Li J et al (2020) In-hospital postoperative pneumonia following geriatric intertrochanteric fracture surgery: incidence and risk factors. Clin Interv Aging 15:1599–1609. https://doi.org/10.2147/CIA.S268118
Numata T, Nakayama K, Fujii S et al (2018) Risk factors of postoperative pulmonary complications in patients with asthma and COPD. BMC Pulm Med 18:4. https://doi.org/10.1186/s12890-017-0570-8
Graham EM, Atz AM, Butts RJ et al (2011) Standardized preoperative corticosteroid treatment in neonates undergoing cardiac surgery: results from a randomized trial. J Thorac Cardiovasc Surg 142:1523–1529. https://doi.org/10.1016/j.jtcvs.2011.04.019
Sumida M, Inaba H, Isawa E et al (1999) Prevention by methylprednisolone of increased circulating tumor necrosis factor-alpha levels and lung injury associated with systemic inflammatory response syndrome due to intraperitoneal hyperthermia. Anesth Analg 88:771–776. https://doi.org/10.1097/00000539-199904000-00017
Sauerland S, Nagelschmidt M, Mallmann P et al (2000) Risks and benefits of preoperative high dose methylprednisolone in surgical patients: a systematic review. Drug Saf 23:449–461. https://doi.org/10.2165/00002018-200023050-00007
MT K. Endocrine Pharmacology. In: Hemmings HC Jr ET, ed. Pharmacology and physiology for anesthesia: foundations and clinical application. 2nd ed.: Philadelphia, Elsevier; 2019:708–731.
Matsutani T, Onda M, Sasajima K et al (1998) Glucocorticoid attenuates a decrease of antithrombin III following major surgery. J Surg Res 79:158–163. https://doi.org/10.1006/jsre.1998.5404
Takeda S, Takeda S, Kim C et al (2003) Preoperative administration of methylprednisolone attenuates cytokine-induced respiratory failure after esophageal resection. J Nippon Med Sch 70:16–20. https://doi.org/10.1272/jnms.70.16
Jeong H, Choi JW, Ahn HJ et al (2019) The effect of preventive use of corticosteroids on postoperative complications after esophagectomy: a retrospective cohort study. Sci Rep 9:11984. https://doi.org/10.1038/s41598-019-48349-0
Xu Y, Lai C, Xu G et al (2019) Risk factors of ventilator-associated pneumonia in elderly patients receiving mechanical ventilation. Clin Interv Aging 14:1027–1038. https://doi.org/10.2147/CIA.S197146
Kardos P, Wencker M, Glaab T et al (2007) Impact of salmeterol/fluticasone propionate versus salmeterol on exacerbations in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med 175:144–149. https://doi.org/10.1164/rccm.200602-244OC
Wedzicha JA, Calverley PM, Seemungal TA et al (2008) The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med 177:19–26. https://doi.org/10.1164/rccm.200707-973OC
Tornatore KM, Logue G, Venuto RC et al (1994) Pharmacokinetics of methylprednisolone in elderly and young healthy males. J Am Geriatr Soc 42:1118–1122. https://doi.org/10.1111/j.1532-5415.1994.tb06219.x
Funding
This study was supported partly by the National Natural Science Foundation of China (Grant No. 82102297 and 81974296), Basic and Applied Basic Research Foundation of Guangdong Province (Grant No. 2019A1515110020) and Natural Science Foundation of Guangdong Province (Grant No. 2018A0303130224 and 2022A1515012603).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Consent to participate
Not applicable.
Consent for publication
All authors approved the publication of this manuscript.
Ethics Approval
The present study was conducted in accordance with the Declaration of Helsinki and the protocol was approved by the Ethics Committee of our hospital on 14 May 2019 (No.[2019]02–609-02). The requirement for informed consent and clinical trial registration were waived by the committee.
Availability of Data and Material
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, J., Chen, C., Cheng, N. et al. Perioperative administration of methylprednisolone was associated with postoperative pulmonary complications in elderly patients undergoing hip fracture surgery. Aging Clin Exp Res 34, 2005–2012 (2022). https://doi.org/10.1007/s40520-022-02166-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02166-0