Abstract
Objective
To determine the postoperative effectiveness of trimodal prehabilitation in older surgical patients.
Methods
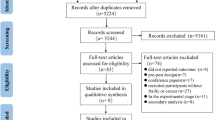
We searched Medline, PubMed, Embase, the Cochrane Library, Web of Science, and ClinicalTrials.gov for observational cohort studies and randomised controlled trials (RCTs) of older surgical patients who underwent trimodal prehabilitation. We performed a meta-analysis to estimate the pooled risk ratio (RR) for dichotomous data and weighted mean difference (MD) for continuous data. Primary outcomes were postoperative mortality and complications, and the secondary outcomes were the 6-min walk test (6MWT) at 4 and 8 weeks after surgery, readmission, and length of hospital stay (LOS). This systematic review and meta-analysis was registered with PROSPERO (registration number: CRD42020201347).
Results
We included 10 studies (four RCTs and six cohort studies) comprising 1553 older surgical patients (trimodal prehabilitation group, n = 581; control group, n = 972). There were no significant differences in postoperative mortality (RR 1.32; 95% confidence interval [CI] 0.52–3.35) and postoperative complications (RR 0.91; 95% CI 0.76–1.09). Prehabilitation did not reduce readmission (RR 0.92; 95% CI 0.61–1.38) and LOS (MD 0.10; 95% CI – 0.34–0.53). In a sub-analysis, trimodal prehabilitation did not significantly improve postoperative mortality, postoperative complications, readmission rates, or LOS when compared with standard care. However, trimodal prehabilitation significantly improved the 6MWT at 4 weeks after surgery (MD 37.49; 95% CI 5.81–69.18).
Conclusions
Our systematic review and meta-analysis demonstrated that trimodal prehabilitation did not reduce postoperative mortality and complications significantly but improved postoperative functional status in older surgical patients. Therefore, more high-quality trials are required.









Similar content being viewed by others
Availability of data and material
All data are fully available without restriction.
References
Weiser TG, Regenbogen SE, Thompson KD et al (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372:139–144. https://doi.org/10.1016/s0140-6736(08)60878-8
Wynter-Blyth V, Moorthy K (2017) Prehabilitation: preparing patients for surgery. BMJ 358:j3702. https://doi.org/10.1136/bmj.j3702
Lawrence VA, Hazuda HP, Cornell JE et al (2004) Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 199:762–772. https://doi.org/10.1016/j.jamcollsurg.2004.05.280
Aucoin S, McIsaac D (2019) Emergency general surgery in older adults: a review. Anesthesiol Clin 37:493–505. https://doi.org/10.1016/j.anclin.2019.04.008
Volkert D, Beck AM, Cederholm T et al (2019) ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr 38:10–47. https://doi.org/10.1016/j.clnu.2018.05.024
Levett DZ, Edwards M, Grocott M, Mythen M (2016) Preparing the patient for surgery to improve outcomes. Best Pract Res Clin Anaesthesiol 30:145–157. https://doi.org/10.1016/j.bpa.2016.04.002
Levett DZH, Grimmett C (2019) Psychological factors, prehabilitation and surgical outcomes: evidence and future directions. Anaesthesia 74(Suppl 1):36–42. https://doi.org/10.1111/anae.14507
Mavros MN, Athanasiou S, Gkegkes ID et al (2011) Do psychological variables affect early surgical recovery? PLoS ONE 6:e20306. https://doi.org/10.1371/journal.pone.0020306
Robinson TN, Wu DS, Pointer L et al (2013) Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 206:544–550. https://doi.org/10.1016/j.amjsurg.2013.03.012
Zhu M, Wei J, Chen W et al (2017) Nutritional Risk and Nutritional Status at Admission and Discharge among Chinese Hospitalized Patients: A Prospective, Nationwide, Multicenter Study. J Am Coll Nutr 36:357–363. https://doi.org/10.1080/07315724.2017.1304293
Bousquet-Dion G, Awasthi R, Loiselle SÈ et al (2018) Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol 57:849–859. https://doi.org/10.1080/0284186X.2017.1423180
Chen BP, Awasthi R, Sweet SN et al (2017) Four-week prehabilitation program is sufficient to modify exercise behaviors and improve preoperative functional walking capacity in patients with colorectal cancer. Support Care Cancer 25:33–40. https://doi.org/10.1007/s00520-016-3379-8
Gillis C, Li C, Lee L et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121:937–947. https://doi.org/10.1097/aln.0000000000000393
Li C, Carli F, Lee L et al (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27:1072–1082. https://doi.org/10.1007/s00464-012-2560-5
Minnella EM, Bousquet-Dion G, Awasthi R et al (2017) Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer: a five-year research experience. Acta Oncol 56:295–300. https://doi.org/10.1080/0284186x.2016.1268268
Fulop A, Lakatos L, Susztak N et al (2020) The effect of trimodal prehabilitation on the physical and psychological health of patients undergoing colorectal surgery: a randomised clinical trial. Anaesthesia 76:82–90. https://doi.org/10.1111/anae.15215
Wang B, Shelat VG, Chow JJL et al (2020) Prehabilitation Program Improves Outcomes of Patients Undergoing Elective Liver Resection. J Surg Res 251:119–125. https://doi.org/10.1016/j.jss.2020.01.009
Bruns ER, van den Heuvel B, Buskens CJ et al (2016) The effects of physical prehabilitation in elderly patients undergoing colorectal surgery: a systematic review. Colorectal Dis 18:O267-277. https://doi.org/10.1111/codi.13429
Lyons N, Bernardi K, Olavarria O et al (2020) Prehabilitation among Patients Undergoing Non-Bariatric Abdominal Surgery: A Systematic Review. J Am Coll Surg 231:480–489. https://doi.org/10.1016/j.jamcollsurg.2020.06.024
Vasta S, Papalia R, Torre G et al (2020) The Influence of Preoperative Physical Activity on Postoperative Outcomes of Knee and Hip Arthroplasty Surgery in the Elderly: A Systematic Review. J Clin Med 9:969. https://doi.org/10.3390/jcm9040969
Forbes C, Swan F, Greenley S et al (2020) Physical activity and nutrition interventions for older adults with cancer: a systematic review. J Cancer Surviv 14:689–711. https://doi.org/10.1007/s11764-020-00883-x
Gillis C, Buhler K, Bresee L et al (2018) Effects of Nutritional Prehabilitation, With and Without Exercise, on Outcomes of Patients Who Undergo Colorectal Surgery: A Systematic Review and Meta-analysis. Gastroenterology 155:391-410.e394. https://doi.org/10.1053/j.gastro.2018.05.012
Looijaard S, Slee-Valentijn MS, Otten RHJ et al (2018) Physical and Nutritional Prehabilitation in Older Patients With Colorectal Carcinoma: A Systematic Review. J Geriatr Phys Ther 41:236–244. https://doi.org/10.1519/jpt.0000000000000125
Chia CL, Mantoo SK, Tan KY (2016) “Start to finish trans-institutional transdisciplinary care”: a novel approach improves colorectal surgical results in frail elderly patients. Colorectal Dis 18:O43-50. https://doi.org/10.1111/codi.13166
Carli F, Bousquet-Dion G, Awasthi R et al (2020) Effect of Multimodal Prehabilitation vs Postoperative Rehabilitation on 30-Day Postoperative Complications for Frail Patients Undergoing Resection of Colorectal Cancer: A Randomized Clinical Trial. JAMA Surg 155:233–242. https://doi.org/10.1001/jamasurg.2019.5474
van der Vlies E, Smits AB, Los M et al (2020) Implementation of a preoperative multidisciplinary team approach for frail colorectal cancer patients: Influence on patient selection, prehabilitation and outcome. J Geriatr Oncol 11:1237–1243. https://doi.org/10.1016/j.jgo.2020.04.011
van Rooijen SJ, Molenaar CJL, Schep G et al. (2019) Making patients fit for surgery: Introducing a four pillar multimodal prehabilitation program in colorectal cancer. Am J Phys Med Rehabil 98:888–896. https://doi.org/10.1097/PHM.0000000000001221
Bradley A, Marshall A, Stonehewer L et al (2013) Pulmonary rehabilitation programme for patients undergoing curative lung cancer surgery. Eur J Cardiothorac Surg 44:e266–e271. https://doi.org/10.1093/ejcts/ezt381
Wan X, Wang W, Liu J et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Pecorelli N, Fiore JF, Gillis C Jr et al (2016) The six-minute walk test as a measure of postoperative recovery after colorectal resection: further examination of its measurement properties. Surg Endosc 30:2199–2206. https://doi.org/10.1007/s00464-015-4478-1
Luther A, Gabriel J, Watson R et al (2018) The Impact of Total body prehabilitation on post-operative outcomes after major abdominal surgery: a systematic review. World J Surg 42:2781–2791. https://doi.org/10.1007/s00268-018-4569-y
Hughes MJ, Hackney RJ, Lamb PJ et al (2019) Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg 43:1661–1668. https://doi.org/10.1007/s00268-019-04950-y
Chou Y, Kuo H, Shun S (2018) Cancer prehabilitation programs and their effects on quality of life. Oncol Nurs Forum 45:726–736. https://doi.org/10.1188/18.Onf.726-736
Daniels SL, Lee MJ, George J et al (2020) Prehabilitation in elective abdominal cancer surgery in older patients: systematic review and meta-analysis. BJS Open. https://doi.org/10.1002/bjs5.50347,10.1002/bjs5.50347
Mouch CA, Kenney BC, Lorch S et al (2020) Statewide prehabilitation program and episode payment in medicare beneficiaries. J Am Coll Surg 230:306–313. https://doi.org/10.1016/j.jamcollsurg.2019.10.014
Klainin-Yobas P, Oo WN, Suzanne Yew PY et al (2015) Effects of relaxation interventions on depression and anxiety among older adults: a systematic review. Aging Ment Health 19:1043–1055. https://doi.org/10.1080/13607863.2014.997191
Tew GA, Ayyash R, Durrand J et al (2018) Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery. Anaesthesia 73:750–768. https://doi.org/10.1111/anae.14177
Zhu M, Cui H, Chen W et al (2020) Guidelines for parenteral and enteral nutrition in geriatric patients in China. AGING MEDICINE 3:110–124. https://doi.org/10.1002/agm2.12110
Bolshinsky V, Li M, Ismail H et al (2018) Multimodal prehabilitation programs as a bundle of care in gastrointestinal cancer surgery: a systematic review. Dis Colon Rectum 61:124–138. https://doi.org/10.1097/dcr.0000000000000987
Faithfull S, Turner L, Poole K et al (2019) Prehabilitation for adults diagnosed with cancer: A systematic review of long-term physical function, nutrition and patient-reported outcomes. Eur J Cancer Care 28:e13023. https://doi.org/10.1111/ecc.13023
Funding
None.
Author information
Authors and Affiliations
Contributions
LCY and LZH performed data acquisition and screening. LCY and LXL participated in data analysis. LCY and ZMW were responsible for the concept and designed the study. LCY, LZH, LXL and ZMW discussed rational and revised the manuscript. ZMW made final approval of the version to be published. All the authors discussed the results and made devotion to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Statement of human and animal rights
Not applicable.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, C., Lu, Z., Zhu, M. et al. Trimodal prehabilitation for older surgical patients: a systematic review and meta-analysis. Aging Clin Exp Res 34, 485–494 (2022). https://doi.org/10.1007/s40520-021-01929-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01929-5